Grafting techniques for Peyronie’s disease
Introduction
Peyronie’s disease (PD) is an acquired fibrotic condition with the formation of plaque(s) in the tunica albuginea of the penis (1-3). PD can lead to the following symptoms: penile plaque(s), curvature, penile deformities (such as hourglass), shortening, painful erections, and erectile dysfunction (ED) (4-9). The most recognized presentation in affected patients is penile curvature that can lead to inability to have sexual intercourse (1,7,10-13). In the stable phase of the disease, surgical therapy may be considered in order to correct significant penile curvature, with the correct indications.
Surgical therapy of PD is subdivided in three main procedures: (I) plication techniques; (II) grafting techniques with partial plaque excision/incision followed by closure of the tunica albuginea defect with various grafts; and (III) correction of curvature with penile prosthesis implantation in patients with ED not responding to medical therapy (5,14). This article is focused on grafting techniques, with special attention given to indications, preoperative considerations, patient counseling, and technique outcomes. The aim of this review is to provide an overview of recent articles that have reported clinical outcomes of grafting techniques, and to discuss novel grafts and grafting techniques. In October 2015, a PubMed database search was performed to research studies on PD grafting techniques that were published between 2010 and 2015. Search keywords included PD, surgery, surgical therapy, grafting, grafting techniques, and grafts. Articles reporting plication techniques, penile prosthesis implantation, and case reports were excluded. Moreover, papers that included congenital penile curvature cases, and series not published in English were excluded. Finally, animal and experimental models, as well as comparative studies, were also excluded from this review.
Indications for surgical therapy
Surgical therapy remains the gold standard to correct penile curvature in stable PD. In general, surgical correction for curvature is indicated when the PD duration is >12 months, and when the stable phase of PD is >6 months. Moreover, the patient should be pain-free. It is required that the patient be unable to perform sexual intercourse due to the significant degree of penile curvature. This is of utmost importance, as surgical therapy can be associated with adverse outcomes, i.e., postoperative ED, sensory loss at the glans penis, or penile shortening.
Patients suffering from PD should be counseled that all therapeutic options available today are symptomatic, i.e., they can relieve symptoms associated with the disease, but there is no healing or reversal of the actual condition. This aspect is especially important in the surgical treatment of penile curvature, as the risk of curvature recurrence is 10–33% (1,15). Therefore, surgical treatment for penile curvature should only be performed in the stable phase of the disease in order to minimize the risk of recurrence.
Generally, plication techniques are applied when penile curvature is <60°. The result is penile straightening by shortening the convex side of the curvature. The most familiar plication technique is the Nesbit procedure (16). The main adverse effect associated with plication is shortening of erect penile length; the more severe the curvature, the more pronounced the postoperative penile shortening. Penile curvatures >60° will worsen penile shortening effect after plication, often leading to patient dissatisfaction (17,18).
Grafting techniques
In penile curvatures >60°, the preferred surgical treatment is a grafting technique, as these procedures aim to maintain penile length (7,15). This technique requires either a plaque incision or partial plaque excision at the point of maximum curvature. This results in a tunica albuginea defect, which is then closed by various autologous or non-autologous grafts. Penile straightening with this technique is achieved by stretching the concave side of curvature, lessening the risk of penile shortening. Thus, grafting techniques can also be indicated when patients develop a short penis from PD, to avoid further shortening with plication. Moreover, the presence of an hourglass deformity is another indication for a grafting technique, as this deformity can develop as a result of extensive plaque formation in the tunica albuginea with concentric narrowing of the cavernous bodies. Grafting techniques are more complex than plication as they require extensive dissection and lifting of the neurovascular bundle within Buck’s fascia. Postoperative ED risk is higher with grafting techniques than with plication, therefore patients need to have documented preoperative erectile rigidity (Erection Hardness Score ≥3) (5). In this regard, it should be emphasized that a proper preoperative assessment of erectile function is strongly recommended. Initially, total plaque excision was performed in the surgical treatment of PD, with the objective of removing all of the plaques of the affected tunica albuginea. However, these early excision procedures resulted in higher rates of postoperative ED (19). Currently, total plaque excision is not commonly performed and not recommended. Grafting techniques indications for PD are listed in Table 1.
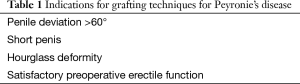
Full table
Surgical approach for grafting techniques
The surgical approach for PD treatment is similar for all grafting techniques. First, a circumcising skin incision and penile degloving down to the base of the penis is performed to provide exposure of the entire penile shaft. Beginning next to the urethra, Buck’s fascia is, most commonly, opened on both sides. This is followed by careful lateral dissection and mobilization of the neurovascular bundle. It is also possible to perform a medial dissection of the neurovascular bundle through the bed of the dorsal vein (5). However, in the case of an hourglass deformity, lateral dissection of the neurovascular bundle is strongly recommended for adequate exposure of the lateral parts of the tunica albuginea. An artificial erection is achieved, either by injecting saline into the corporal bodies or administration of a vasoactive agent, to clearly identify the point of maximum curvature. Subsequently, plaque incision or a partial plaque excision is performed at the point of maximum curvature on the concave side of curvature. Plaque incision is most commonly accomplished with a modified H- or double Y-incision. Partial plaque excision is usually executed by excising an ellipsoid part of the tunica albuginea at the point of maximum curvature, with the resulting defect then extended laterally (5,7,14). There are also other techniques which result in a rectangular defect of the tunica albuginea once the partial plaque excision or incision is completed (20,21). During this step, it is crucial not to violate the underlying erectile tissues, as this may result in postoperative ED. The graft of choice is then adjusted to the defect and secured to the tunica with a continuous suture. If collagen fleece is used as graft, no exact adjustment and sewing in the defect is needed (14). An artificial erection is then performed to confirm the watertight closure of the tunica albuginea and satisfactory correction of the curvature. Finally, Buck’s fascia is closed on both sides by a running suture, and the penile skin is approximated with interrupted sutures.
Available grafting materials
After plaque incision or partial plaque excision, the resultant tunica albuginea defect must be closed in order to restore the integrity of the tunica and the penis. There are several grafting materials for this purpose (Table 2) (5,14,17,19,22-33). Synthetic grafting materials like polytetrafluoroethylene (Gore-Tex®/Teflon®, Gore Inc., Flagstaff, AZ, USA) or polyethylene terephthalate (Dacron®, DuPont, Wilmington, DE, USA) were previously used in the surgical treatment of PD. However, due to the risk of infection, inflammatory response, fibrosis, rejection reaction, allergic reaction, or contracture due to inelasticity of the material, these grafts are not recommended any more (5,34). Today, two graft types are mainly used: autologous grafts (e.g., saphenous vein, buccal mucosa) and non-autologous grafts (allografts/xenografts). The use of autologous grafts necessitates a second incision for harvesting, which, in turn, leads to greater morbidity and prolonged operative time. Complications associated with harvesting of the autologous material include wound healing disorders, infection, scarring, swelling, pain, numbness, and possible lymphedema (30,33). For this reason, there is a growing interest among urologists to use non-autologous “off-the-shelf” grafts (tissue-engineered materials) like pericardium, small intestinal submucosa (SIS), or collagen fleece (5,14).
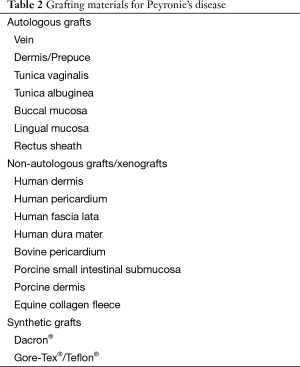
Full table
Ideal graft characteristics
The search for the ideal graft for PD surgery is ongoing. Up to date, no single available graft has emerged as the best option for the surgical repair of PD. The ideal requirements for a graft for PD reconstructive surgery include: availability, resistance to infection, lack of contraction, promotes hemostasis, preserve erectile capacity, be cost-effective, and should not prolong operative time; off-the-shelf grafts should be packaged in various sizes to fit the patient’s tunical defects. Unfortunately, the ideal graft has not yet been developed, and there are no robust data from well-designed comparative studies to determine the best graft type for PD surgery. This issue demands further research to examine histological and mechanical characteristics of different graft materials, and to evaluate corresponding clinical outcomes. There are current attempts to create an autologous tissue-engineered endothelialized graft derived from a skin biopsy (35). In an animal model, this graft has shown robust tensile forces that adequately preserve the veno-occlusive mechanism. Such attempts to create an artificial tunica albuginea, however, need further investigation both in vitro and in animal models before such material can be used in human subjects.
Surgical outcomes
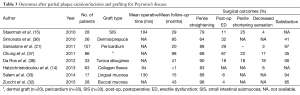
Table 3 summarizes the plaque incision or partial plaque excision and grafting for PD literature published since 2010 (14,15,21,32,33,36-38).
Full table
Staerman et al. reported on their experience with SIS grafting following plaque incision in 28 patients (15). After a mean follow-up of 29 months, penile straightening was achieved in 79% of patients, while 25% of patients experienced penile shortening, and postoperative ED was 11%. It is noteworthy that recurrence of curvature occurred in 33% of patients. The authors concluded that patients should be informed about the risk of recurrent curvature, and, in the case of failure, the possibility of a repeat surgical intervention. In regard to the SIS as graft, it should be mentioned that there was one rejection reaction documented and, as such, patients need to be informed preoperatively about this rare complication.
In another series that included 26 PD patients, Simonato et al. described their grafting experience with a penile dermal flap (36). In this study, a preputial flap was harvested, prepared with sandpaper, and placed in the defect of the tunica albuginea after an H-shaped plaque incision. Mean follow-up in this study was 95 months. Complete penile straightening was achieved in 64% of patients, and postoperative ED was observed in 32% of the study cohort. Only 41% of patients were satisfied with the procedure and the end result. As an interesting complication, 41% of patients undergoing the dermal flap grafting developed inclusion cysts at the surgical site, at a mean of 8 months postoperatively. These patients were recommended surgical cyst resection. Because of these results, the authors abandoned using this grafting material, and strongly advised against the use of dermal flap as potential graft for PD grafting surgery. According to the results of this study, the dermal graft cannot be recommended for reconstruction of the tunica albuginea defect in PD surgery.
In a multicenter study, Sansalone et al. presented long-term results of partial plaque excision and grafting with bovine pericardium (21). This study included 157 PD patients in the stable phase, who underwent surgery in four different centers. Only patients with adequate preoperative erectile function (IIEF-5 score ≥15, and peak systolic velocity ≥ 35 cm/s on color duplex sonography) were included in this study. Patients not displaying these parameters were offered penile prosthesis implantation. By performing a double Y-incision at the point of maximum curvature with consequent stretching of the penile shaft, the authors achieved penile length gain in all patients (median length gain 2.5 cm). After a median follow-up of 20 months, 88% of patients showed a completely straight penis. Twenty-nine percent of patients experienced ED and required phosphodiesterase-type 5 (PDE-5) inhibitors to achieve adequate rigidity. Ninety-seven percent of patients were satisfied with the surgical results. This study concludes that proper preoperative patient selection is key to success and leads to a higher rate of patient satisfaction. Again, it should be mentioned that proper preoperative assessment of erectile function is crucial before planning a grafting technique, by means of the IIEF questionnaire, and color duplex Doppler imaging. In order to avoid worsening of ED after surgery and thus avoiding dissatisfied patients, a penile prosthesis implantation in combination with penile curvature correction should be recommended in patients with PD and poor preoperative erectile function.
Chung et al. assessed long-term results after PD graft surgery (minimum follow-up of 5 years) (37). The authors performed a retrospective analysis that included 86 patients, however, only 46 patients were available for follow-up. Twenty patients underwent a grafting technique with dermal graft, 33 patients with pericardium, and 33 patients with SIS. In total, penile straightening was achieved in 68% of patients after grafting in this series. Mean follow-up of this study was 98 months. At the time of follow-up, 50% of patients with dermal graft, 87% with pericardium, and 76% with SIS graft reported recurrence of curvature. Twenty-two percent of all patients noted penile shortening. Regarding erectile function, 67% of all patients had postoperative ED and subsequently needed PDE-5 inhibitors or intracavernous injections to achieve adequate penile rigidity. Altered sensation or glans hypoesthesia was reported in 17% of the group. The overall patient satisfaction in this study, assessed by a 5-point scale, was 2.6, with more than 65% of patients being dissatisfied with the outcomes of PD graft surgery. Penile length loss and development of de-novo ED were the main reasons for patient dissatisfaction. Sixty-one percent of patients reported they would not be willing to undergo the same procedure if given the option again. These results were contrary to previously published short-term results from the same unit, which showed, overall, more encouraging outcomes after grafting surgery in PD with the same graft types (39). The authors concluded that even though short-term results are encouraging, many patients experience poor satisfaction outcomes at 5-year follow-up.
The dissuasive results of this study reflect the importance of preoperative patient counseling to planning a surgical approach in PD. Patients must be informed preoperatively in detail about possible complications and negative outcomes associated with the specific surgical approach. It is important that the patient understands that surgery has its limitations and, more important, that it is unlikely for any surgical intervention to return the penis to its original state (length, shape, rigidity). Adequate preoperative patient counseling leads to higher satisfaction rates after surgery.
In a study by Da Ros et al., the authors describe long-term results after grafting with an autologous tunical albugineal crural graft (38). The authors included 33 patients with PD. Mean follow-up after surgery was 41 months. Complete penile straightening was achieved in 90% of patients, while penile shortening occurred in 18% of patients. Eighteen percent of the study cohort experienced ED postoperatively and required either PDE-5 inhibitors or intracavernous injections. Hypoesthesia at the glans penis was reported by 18% of patients. The patient satisfaction rate in this study was as high as 90%. However, this technique requires an additional perineal incision for harvesting of one or two albugineal crural grafts. Consequently, the graft has to be prepared to remove all residual ischiocavernous muscle before placing and sewing it into the tunical defect. This accounts for longer operative times, and may also lead to complications at the site where the autologous material was harvested. Unfortunately, the authors did not report on operative times in their series. The authors did, however, indicate that this technique can be associated with increased risk of postoperative ED due to potential damages to the neurovascular bundle during dissection of the crura. Moreover, the diminution of the crural compartment of the cavernous bodies might impair the hemodynamics of the penis. Despite this potential risk, the rate of postoperative ED in this series was within the expected range after grafting for PD.
Hatzichristodoulou et al. described, in a more recent study, their experience with collagen fleece as novel graft material for PD reconstructive surgery in 63 patients (14). The authors reported early results after correction of penile curvature in patients with stable PD, by partial plaque excision followed by grafting with a self-adhesive collagen fleece. The collagen fleece used as graft (TachoSil®, Baxter Healthcare Corporation, CA, USA) is coated with tissue sealant and therefore has self-adhesive properties. The graft is moistened with physiological saline and then placed on the tunical defect after partial plaque excision or incision. It is important that the fleece overlaps the defect at each side for at least 5 mm. Exact adjustment and sewing into the defect, as performed with other grafts, is omitted, thus, one major advantage of this graft method is the reduced operative time. Another advantage is the hemostatic effect provided by the fleece. The costs of the collagen fleece are lower compared to other grafts (e.g., 4-layer-SIS). The authors of this feasibility study reported the mean operative time was 94 min. Total penile straightening (no residual curvature) was achieved in 83% of patients. 17% had mild residual curvature of <10° at the end of surgery. Of the study cohort, 92% experienced normal glans sensibility, with only 8% reporting diminished sensation at the time of discharge from hospital. Early results of this study are encouraging. However, long-term results are necessary to confirm these findings and to evaluate more clinical and objective outcomes.
The results of a small series of 17 PD patients who underwent grafting with lingual mucosa were reported by Salem et al. (33). After a mean follow-up of 15 months, the authors reported complete penile straightening in 88% of subjects. De-novo ED after surgery was observed in 6% of patients. Ninety-four percent of the cohort was satisfied with the surgery result. Despite these encouraging outcomes, the study is limited by the small patient number and the short follow-up. Moreover, the authors reported on donor site complications, such as swelling, numbness, and pain. It should also be mentioned that the operative time of this approach is longer due to harvesting and preparing the autologous tissue to be used as a graft. Mean operative time in this study was 130 min, which is longer than other grafting techniques in PD (14). Long-term follow-up data from a larger cohort is required to confirm these initial results.
A similar graft, buccal mucosa, was used for grafting surgery by Zucchi et al. (32). They included 32 patients; however, only 28 patients were available for follow-up. At a mean follow-up of 43 months, the authors reported total straightening of the penis was achieved in 96% and de-novo ED occurred in 4% of patients. The authors reported a patient satisfaction rate of 85%. As noted, one should keep in mind that it requires additional time to harvest and prepare the buccal mucosa and to close the subsequent iatrogenic defect. Unfortunately, there is no operative time mentioned. In this study, discomfort at the donor site (cheek) was reported as a complication. A main limitation of this study is its retrospective nature.
Postoperative management
There are several strategies regarding the postoperative management of patients with PD after grafting procedures. The transurethral catheter is usually removed on the first postoperative day (33,36). Loose or compressive dressing around the penis is recommended for at least 24 h to avoid hematoma formation (14,15,20,36). Patients should refrain from sexual intercourse and sexual activities for 4–6 weeks postoperatively (21,30,38). Despite limited data, postoperative rehabilitation is recommended in order to reduce the risk of postoperative ED, enhance recovery of erectile function, reduce the risk of penile length loss after surgery, and optimize straightening of the penis (1,5,7,30). Massage and stretching of the penis twice a day starts 2 weeks after surgery for a period of 4 weeks. Nocturnal PDE-5 inhibitors have been recommended in order to improve nocturnal erections, reduce the risk of postoperative ED, stretch the penis, and improve oxygenation to the applied graft (40). This should start 7–10 days after surgery for a period of 6 weeks. The use of external penile traction devices has been encouraged to reduce postoperative penile shortening. Penile traction therapy is recommended to start 2–3 weeks after surgery on a daily basis for 2–8 h, for a period of 3 months (1,7).
Complications
Preoperative counseling with a fully documented, signed consent by patients who undergo surgical therapy for PD is imperative. Realistic expectations have to be set, as it is crucial that the PD patient understands that there are surgical limitations to length gains. The most important risk associated with surgical therapy for PD is penile shortening that can occur with any surgical technique. The risk of shortening is, in theory, less with grafting techniques (18). This is an important aspect as almost all patients have already experienced penile shortening associated with their PD (7). Recurrent curvature after successful surgical therapy can occur in 10–33% of cases, specifically when a new episode of PD occurs (1,15). As stated, there is no healing of the PD condition. In this context, persistent curvature may also be present after surgery. However, when the post-operative curvature is <20°, most patients are “functionally straight” and satisfied. The risk of postoperative ED can be as high as 67% (37). This is also very important to document as up to 58% of PD patients have ED at the time of PD presentation (7). Change or decrease of penile sensation (penile hypoesthesia, glans numbness) is a complication that has been reported in 3–31% of cases (14,21,31). This is important, as it can lead to orgasmic dysfunction in some patients. However, most cases will resolve spontaneously in the majority of patients with time.
Conclusions
Grafting techniques represent the preferred surgical treatment in patients with stable PD, penile curvature >60°, short penis, or an hourglass deformity. Patients who are scheduled for a grafting surgery, however, must have satisfactory preoperative erectile rigidity. Preoperatively, the patient needs to be fully counseled about adverse effects and negative outcomes, such as diminished sensation at the glans penis or diminished erectile function. Various grafts have been used for closure of the tunica albuginea defect following plaque incision or partial plaque excision. Today, autologous and non-autologous grafts (“off-the-shelf” grafts) are used widely. Each graft type has its advantages and disadvantages. There is no “ideal” graft that can be recommended. Surgeon experience, careful patient selection, patient preference, and type of penile deformity will affect the choice of graft. Moreover, availability and costs of grafts will limit and guide their use in penile reconstructive surgery for PD.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Levine LA, Burnett AL. Standard operating procedures for Peyronie's disease. J Sex Med 2013;10:230-44. [Crossref] [PubMed]
- Mulhall JP, Creech SD, Boorjian SA, et al. Subjective and objective analysis of the prevalence of Peyronie's disease in a population of men presenting for prostate cancer screening. J Urol 2004;171:2350-3. [Crossref] [PubMed]
- Tal R, Hall MS, Alex B, et al. Peyronie's disease in teenagers. J Sex Med 2012;9:302-8. [Crossref] [PubMed]
- Hatzichristodoulou G, Lahme S. Peyronie's Disease. In: Merseburger AS, Kuczyk MM, Moul JW, editors. Urology at a Glance. New York: Springer-Verlag Berlin Heidelberg; 2014:225-36.
- Kadioglu A, Küçükdurmaz F, Sanli O. Current status of the surgical management of Peyronie's disease. Nat Rev Urol 2011;8:95-106. [Crossref] [PubMed]
- Larsen SM, Levine LA. Review of non-surgical treatment options for Peyronie's disease. Int J Impot Res 2012;24:1-10. [Crossref] [PubMed]
- Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med 2010;7:2359-74. [Crossref] [PubMed]
- Smith JF, Walsh TJ, Lue TF. Peyronie's disease: a critical appraisal of current diagnosis and treatment. Int J Impot Res 2008;20:445-59. [Crossref] [PubMed]
- Nelson CJ, Mulhall JP. Psychological impact of Peyronie's disease: a review. J Sex Med 2013;10:653-60. [Crossref] [PubMed]
- Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol 2006;175:2115-8; discussion 2118. [Crossref] [PubMed]
- Acikgoz A, Gokce E, Asci R, et al. Relationship between penile fracture and Peyronie's disease: a prospective study. Int J Impot Res 2011;23:165-72. [Crossref] [PubMed]
- Hatzichristodoulou G. Conservative therapy of Peyronie's disease - update 2015. Urologe A 2015;54:641-7. [Crossref] [PubMed]
- Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's disease: AUA Guideline. J Urol 2015;194:745-53. [Crossref] [PubMed]
- Hatzichristodoulou G, Gschwend JE, Lahme S. Surgical therapy of Peyronie's disease by partial plaque excision and grafting with collagen fleece: feasibility study of a new technique. Int J Impot Res 2013;25:183-7. [Crossref] [PubMed]
- Staerman F, Pierrevelcin J, Ripert T, et al. Medium-term follow-up of plaque incision and porcine small intestinal submucosal grafting for Peyronie's disease. Int J Impot Res 2010;22:343-8. [Crossref] [PubMed]
- Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol 1965;93:230-2. [PubMed]
- Gur S, Limin M, Hellstrom WJ. Current status and new developments in Peyronie's disease: medical, minimally invasive and surgical treatment options. Expert Opin Pharmacother 2011;12:931-44. [Crossref] [PubMed]
- Kueronya V, Miernik A, Stupar S, et al. International multicentre psychometric evaluation of patient-reported outcome data for the treatment of Peyronie's disease. BJU Int 2015;115:822-8. [Crossref] [PubMed]
- Segal RL, Burnett AL. Surgical management for Peyronie's disease. World J Mens Health 2013;31:1-11. [Crossref] [PubMed]
- Levine LA. Partial plaque excision and grafting (PEG) for Peyronie's disease. J Sex Med 2011;8:1842-5. [Crossref] [PubMed]
- Sansalone S, Garaffa G, Djinovic R, et al. Long-term results of the surgical treatment of Peyronie's disease with Egydio's technique: a European multicentre study. Asian J Androl 2011;13:842-5. [Crossref] [PubMed]
- Cormio L, Zucchi A, Lorusso F, et al. Surgical treatment of Peyronie's disease by plaque incision and grafting with buccal mucosa. Eur Urol 2009;55:1469-75. [Crossref] [PubMed]
- Craatz S, Spanel-Borowski K, Begemann JF, et al. The dorsal lamina of the rectus sheath: a suitable grafting material for the penile tunica albuginea in Peyronie's disease? BJU Int 2006;97:134-7. [Crossref] [PubMed]
- Hsu GL, Chen HS, Hsieh CH, et al. Long-term results of autologous venous grafts for penile morphological reconstruction. J Androl 2007;28:186-93. [Crossref] [PubMed]
- Kalsi JS, Christopher N, Ralph DJ, et al. Plaque incision and fascia lata grafting in the surgical management of Peyronie's disease. BJU Int 2006;98:110-4; discussion 114-5. [Crossref] [PubMed]
- Kim DH, Lesser TF, Aboseif SR. Subjective patient-reported experiences after surgery for Peyronie's disease: corporeal plication versus plaque incision with vein graft. Urology 2008;71:698-702. [Crossref] [PubMed]
- Knoll LD. Use of porcine small intestinal submucosal graft in the surgical management of Peyronie's disease. Urology 2001;57:753-7. [Crossref] [PubMed]
- Knoll LD. Use of small intestinal submucosa graft for the surgical management of Peyronie's disease. J Urol 2007;178:2474-8; discussion 2478. [Crossref] [PubMed]
- Levine LA, Estrada CR, Storm DW, et al. Peyronie disease in younger men: characteristics and treatment results. J Androl 2003;24:27-32. [PubMed]
- Levine LA, Larsen SM. Surgery for Peyronie's disease. Asian J Androl 2013;15:27-34. [Crossref] [PubMed]
- Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med 2008;5:2221-8; discussion 2229-30. [Crossref] [PubMed]
- Zucchi A, Silvani M, Pastore AL, et al. Corporoplasty using buccal mucosa graft in Peyronie disease: is it a first choice? Urology 2015;85:679-83. [Crossref] [PubMed]
- Salem EA, Elkady EH, Sakr A, et al. Lingual mucosal graft in treatment of Peyronie disease. Urology 2014;84:1374-7. [Crossref] [PubMed]
- Brannigan RE, Kim ED, Oyasu R, et al. Comparison of tunica albuginea substitutes for the treatment of Peyronie's disease. J Urol 1998;159:1064-8. [Crossref] [PubMed]
- Imbeault A, Bernard G, Ouellet G, et al. Surgical option for the correction of Peyronie's disease: an autologous tissue-engineered endothelialized graft. J Sex Med 2011;8:3227-35. [Crossref] [PubMed]
- Simonato A, Gregori A, Varca V, et al. Penile dermal flap in patients with Peyronie's disease: long-term results. J Urol 2010;183:1065-8. [Crossref] [PubMed]
- Chung E, Clendinning E, Lessard L, et al. Five-year follow-up of Peyronie's graft surgery: outcomes and patient satisfaction. J Sex Med 2011;8:594-600. [Crossref] [PubMed]
- Da Ros CT, Graziottin TM, Ribeiro E, et al. Long-term follow-up of penile curvature correction utilizing autologous albugineal crural graft. Int Braz J Urol 2012;38:242-7; discussion 248-9. [Crossref] [PubMed]
- Kovac JR, Brock GB. Surgical outcomes and patient satisfaction after dermal, pericardial, and small intestinal submucosal grafting for Peyronie's disease. J Sex Med 2007;4:1500-8. [Crossref] [PubMed]
- Levine LA, Greenfield JM, Estrada CR. Erectile dysfunction following surgical correction of Peyronie's disease and a pilot study of the use of sildenafil citrate rehabilitation for postoperative erectile dysfunction. J Sex Med 2005;2:241-7. [Crossref] [PubMed]


