The role of pre-operative androgen stimulation in hypospadias surgery
Introduction
Hypospadias, one of the most common malformations of male genitalia, is shown to be increasing in incidence (1). The aim of hypospadias surgery is to reconstruct the urethra to the tip of the glans, and to achieve an excellent cosmetic result. The surgical approach is a technically demanding procedure with well-defined complications, including glans dehiscence, urethrocutaneous fistula, meatal stenosis and unsatisfactory cosmesis due to penile scarring. In order to improve the functional and cosmetic results, the use of hormonal stimulation before hypospadias correction has been accepted as a relatively common practice for some decades (2,3). Testosterone use was first reported in 1971 (4) and it has been applied as the hormone of choice for the forthcoming investigations. Nevertheless, despite the widespread use of hormonal stimulation, its use has been rarely reported and consequently remains controversial. Because of the scarcity of randomized and controlled clinical trials on this topic, the establishment of a standard protocol has not been concluded yet. Our objectives were to review the associated studies on androgen treatment prior to hypospadias surgery, the metabolism of the efficacy of testosterone on penile growth, to define the indications, dosage, duration and the route of administration of androgens in hypospadias management.
Hormonal stimulation before hypospadias surgery
To improve the surgical results, androgen stimulation has been recommended since it is believed to temporarily promote phallic growth, which makes the correction easier and results in fewer complications (5,6). Most previous studies have revealed temporary increase in penile length, glans circumference and tissue vascularity with the use of testosterone, dihydrotestosterone (DHT) and human chorionic gonadotropin (2,7). Despite the current use of hormone therapy before hypospadias surgery, its real benefit regarding the surgical results is yet to be defined.
The studies concerning this therapy, mostly non-randomized ones, involve limited numbers of patients and do not evaluate important variables in treatment regimens, adverse effects and surgical outcome. Similarly, there has been no enough study that has clearly shown a clinically beneficial effect of preoperative hormonal treatment, such as an increase in surgical success rates or a decrease in surgical complications. Although not statistically significant, a prospective nonrandomized study showed that patients treated with preoperative testosterone actually had a higher risk of complications (8). It was a retrospective study involving highly heterogeneous groups regarding number of children, time of stimulation and type of hormone used. Another important point is that hormone stimulation was used only in the more severe hypospadias cases.
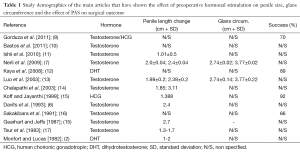
In a systematic review comparing the results of different types of hormone therapy for hypospadias correction, it was concluded that the effect of preoperative hormonal stimulation on surgical outcomes remains unclear and needs further studies with higher quality (9). Even though all 14 studies investigated androgen treatment before the hypospadias surgery, there were considerable heterogeneity regarding the methods, patient selection, hormones, drug dosage and outcome report in the studies, making the realization of this meta-analysis even more difficult (Table 1).
Full table
Koff and Jayanthi reported the benefit of HCG with an increase in growth of the penile shaft proximal to the urethral meatus, corpus spongiosum thickening and a decrease in the severity of chordee, with no method of evaluation of the degree of curvature to be specified (15). They reported statistically significant penile growth, especially in the proximal portion of the penis, moving the ectopic urethral meatus toward the tip of the glans, a characteristic that was not evaluated in other studies. This study indicated a change in the type of surgery required, avoiding use of pedicle flaps and tube repairs in one-fourth of the boys and only one case of urethral fistula after onlay repair in the 12 boys was reported. A reduction of penile curvature was also observed in a randomized controlled trial in which preoperative DHT administration objectively decreased the rate of complications and subjectively improved cosmesis after hypospadias repair (12).
Unfortunately, there is not a randomized clinical study in the literature comparing the use of DHT to testosterone or HCG, to support its beneficial effect. In other words, one cannot find any clinical trials comparing penile growth after use of any of the hormones to another type of hormone. Studies that compared the topical and parenteral administration of testosterone did not demonstrate significant differences in penile length between the routes of application (7,14).
Metabolism
Although the etiology of hypospadias is still unclear, defects anywhere along the pathway of androgen production could potentially be responsible for the occurrence of hypospadias (18). Hypoplastic development of the phallus is thought to render repair of hypospadias more difficult, and often limits functional and cosmetic results. Therefore, preoperative androgen therapy seems to be useful to enlarge the penis, make the repair less difficult and decrease the possibility of complications.
Only the “one randomized study” evaluating effects of topical testosterone (twice daily for 30 days) on the histological neovascularization revealed that use of 1% testosterone propionate ointment before hypospadias surgery promotes an increase in both the number and volume density of blood vessels. Histologic evaluation of the prepuce, which was immunohistochemically stained for von Willebrand factor revealed an increase in the absolute number of blood vessels per high power field and increased blood volume density in patients who received treatment, supporting the theory of neovascularization (10).
In a preliminary study evaluating the effects of DHT local stimulation in hypospadias repair on genital skin morphology, an enormous mitotic activity resembling a basal cell carcinoma pattern of the skin was shown (19). The dermal cells are known to increase their production of mitogenic factors in response to androgens without evolving no pathological changes or alterations in enzyme levels, e.g., due to treatment with androgenic alopecia cell media in vitro (20). Furthermore, it has been shown that DHT provides high local concentrations at the site of application, and serum concentration remains within the normal range, although the exact dose of the application is not accurately assignable (21). In adults, transdermal DHT gel decreases the level of free testosterone while increasing the levels of follicle-stimulating hormone and luteinizing hormone; however, the effect that DHT might have in prepubertal boys is unknown.
In addition, some basic science research studies have demonstrated that androgens may inhibit the epithelialization phase of wound healing, and the wounds in castrated mice and in rats treated with 5alpha-reductase inhibitors were found to heal more rapidly than in controls (22).
Testosterone treatment
Given the clinical uncertainty and lack of high quality evidence to support the value of testosterone for hypospadias repair, preoperative testosterone has been described and used as a method to allow for increase in available foreskin, penile length, glans circumference and neovascularity of the tissues. Therefore, it would improve enhance the surgical outcomes in patients with hypospadias.
The desired therapeutic effect of testosterone has been achieved with local and systemic administration in some studies (7,14). It has been suggested that since externally administered DHT does not require 5 alpha-reductase, it could be more effective than testosterone in enlarging the external genitalia (23). After binding to specific receptor proteins and translocation into the nucleus DHT initiates protein synthesis and stimulates the anabolic effects, i.e., increased mitotic activity, cell turnover time and thickness of the epidermis (24).
In a recent meta-analysis evaluating the effect of preoperative hormonal stimulation on postoperative complications in patients with hypospadias, no strong conclusions could have been drawn regarding the effect of testosterone on surgical outcomes (9). The studies, except two of them, were of low quality and lacked standardized reporting of important patient and surgical details. Since hypospadias repair is complex and involves several variables, such as anatomical variations, surgical technique, tissue handling, suture material and stenting, it is difficult to compare the complication rates. They reported that the patients taking part in this review underwent different surgical techniques such as OIF, TIP, Koyanagi urethroplasty, 2-stage repair and buccal mucosa graft repair, decreasing in order.
The only well designed, randomized study in the literature has evaluated the efficacy of transdermal DHT on the complications and cosmetic results of primary hypospadias surgery and showed that DHT improves outcomes. One major flaw is patient selection, with most patients having mild hypospadias (coronal in 70%, penile in 24% and penoscrotal in 5%). The conclusion we can make from this study is that further well designed randomized studies with similar patients in each group are required.
Despite these limitations, although preoperative hormonal stimulation has been thought to improve surgical results, it is interesting to see that the result of the recent pooled analysis suggests a possible relationship between hormonal use and increased complication rates in patients with severe hypospadias (9). But, this discrepancy was thought to be a result of a selection bias, because of the selected patients exposed to hormonal treatment included those with some of the most severe anatomical defects and unfavorable tissue characteristics.
Several studies have shown an advantage with a statistically significant increase in penile length and glans circumference, and an induction of neovascularization (5,7,15). In a study by Snodgrass, the measurement of glans with in boys undergoing hypospadias repair and newborns undergoing circumcision was documented. Around 25% of boys with distal and 60% with proximal hypospadias were found to have a glans width less than that of the average normal newborn (25). It was found that use of parenteral testosterone 25 mg IM once (monthly for 3 months) in patients with a “significantly smaller penis” has increased penile length and glans circumference significantly with no crucial side effects, such as delay in bone age (13). In another study evaluating the effects of topical 10% testosterone propionate cream (twice daily for 4 weeks) prior to surgery, the authors have noted an increase in dorsal penile length and variable testosterone levels during treatment (23). Sakakibara et al. reported 66.7% overall success rate after primary repair in children with either penoscrotal, scrotal or perineal hypospadias after the use of topical testosterone cream (16).
We randomized 75 children with primary hypospadias who received daily application of 2.5% DHT (3 months) prior to surgery or who underwent TIP hypospadias repair without pretreatment. We have reported a significantly lower complication rate (glandular dehiscence, fistulas) and reoperation in the DHT group compared to a control one (12). There were fewer reoperations for fistulas (1 vs. 4, P>0.05), glanular dehiscence (0 vs. 3, P<0.05) and meatal stenosis (0 vs. 2, P>0.05) performed in patients who underwent DHT treatment than patients without treatment. We also considered penile cosmesis to be improved by DHT pretreatment (moderate-to-severe scarring in 2 patients in treatment group vs. 16 patients in no treatment group). Scar formation after hypospadias repair is an important parameter for cosmetic assessment, and it was found to be significantly lower in children receiving DHT treatment. Due to the proved importance of psychosocial satisfaction and the development of self-esteem in later periods of life, the prevention of scar formation with DHT is thought to be an important parameter for the cosmetic outcome after hypospadias repair. Finally we suggested that pretreatment with DHT transdermal gel is beneficial in decreasing complication and reoperation rates after hypospadias repair, as well as improving cosmetic results.
Indications of preoperative testosterone use
The use of testosterone in male children with a genital defect is not a new concept. But, one can easily realize that testosterone use in clinical practice is not well known. There is a limited data about the current state of its use in the surgical correction of hypospadias in the literature.
Many studies have demonstrated that the effect of parenteral testosterone on penile growth and the prepuce up to the day of surgery is significant in the correction of severe cases of hypospadias. In order to facilitate glanuloplasty, parenteral testosterone therapy has been applied to enlarge the glans particularly in boys with micropenis (13). Similarly, human chorionic gonadotropin pretreatment before severe hypospadias caused the disproportional growth of the hypospadiac phallus, turning the meatus distally, as well as decreasing the severity of chordee (23).
The only study to characterize the practice patterns of pediatric urologists in the USA revealed that although many of them use testosterone prior to hypospadias repair, their approach remain highly variable. In this very recent study, the use of testosterone is primarily used in patients with proximal hypospadias, small appearing penis, reduced glans circumference or reduced urethral plate. They have recommended further prospective studies to create guidelines that can be followed by providers who are actively using preoperative androgen stimulation (26).
The use of testosterone prior to hypospadias repair has been used on patients with microphallic hypospadias or those with a length below what is considered the normal length of a penis of a newborn infant 3.5±0.4 cm (27). Some studies suggested DHT application only in highly selected multiple redo hypospadias procedures, especially in the cases of no genital skin was available for urethral repair, extensive scarring was found, and known surgical techniques were limited in number and choice (19).
Although many articles on the results of hypospadias surgery have been published, only a few have discussed cosmetic results after the repair. The studies have mostly been interested in functional results, therefore there is a lack of information about scar formation after hypospadias repair in the literature.
In a study investigating the effects of hypospadias surgery on psychosexual adjustment, approximately one fourth of patients were dissatisfied with penile appearance and consequently desired cosmetic improvement (28). The reasons for dissatisfaction especially were related to penile scars such as skin tags, skin bridges and keloid scar formation; persistent chordee; meatal configuration and glanular shape, with the consequence that up to 40% of adolescents want to correct the surgical results.
It has been reported that the healing of the coronal sulcus is difficult after reconstructive surgery, due to its poor vascularization. Additionally, dissection of the penile skin and the urethral plate in the coronal sulcus may completely impede coronal vascularization (29). Up to now, corticosteroids have been used to increase scar elasticity and retractability of the foreskin. Kaya et al. have focused on the scar formation after hypospadias repair in boys who used DHT and found a significantly lower rate of scar formation. Finally, they hypothesized that this benefit might be explained by the angiogenesis effects of DHT (12). Part of the rationale for using DHT was to increase the vascularity of the penile skin as an adjunct to wound healing. Naturally continued investigation into the use of supplemental hormones to evaluate the long-term effects in patients with hypospadias is needed.
Dose, duration and routes of application of the treatment
It has been proposed that better surgical conditions might be obtained in the case of hormonal treatment prior to hypospadias surgery, favoring better local skin conditions, increasing penile length and glans circumference resulting in reduced surgical complications.
However, there is no consensus about the details of the hormonal treatment, being all empiric regimens and with lack of data to support one or another therapy. There are still disagreements about the choice of hormone therapy, duration, the appropriate dose and routes of application (topical or parenteral) in the literature.
Some authors have observed significant effects on penile length by using a fixed dose of parenteral testosterone in all patients (25 mg, 1×/mo) (13,29), while the others have adapted the dose to the weight of the child (2 mg/kg/week) (7,15). Those who advocate intramuscular testosterone explain that the rate and degree of absorption of topical testosterone is variable as evidenced by variation in serum testosterone levels, and topical use requires parental compliance for the child to receive the appropriate frequency and dosage (15,16). Contrary to the topical treatment of testosteron, the relatively predictable increase in serum testosterone levels was reported to be an advantage of the parenteral route (14,16).
The variable results have been reported with the use of intramuscular and topical testosterone to stimulate penile growth in the management of hypospadias, but there is no significant difference between these routes of administration. Additionally, transdermal creams and gels were found to provide high local concentrations at the site of application. However, the randomized studies have found no significant difference in outcome with topical or intramuscular routes of administration (7).
Another point of concern is the timing of surgery after DHT cessation, because the cessation time of testosterone therapy prior to surgery is also variable. In some studies topical testosterone application was ceased one week prior to surgery (15), whereas some others skipped doses of intramuscular testosterone if penile length and glans circumference had noticeably increased with the first or first two doses (13). Gorduza et al. gave monthly intramuscular injections and stopped when penile length was at or above 35 mm. They revealed that patients who received the treatment less than 3 months before undergoing surgery presented with a much higher complication rate (50% fistula rate) than those treated more than 3 months prior to surgery (26.3%, P>0.34) (8). They showed that hormonal stimulation might have negative effects on surgery outcomes, affect negatively on the surgery outcomes, most likely due to low event rates. But, in addition to the hormonal treatment itself, the timing of the treatment and the timing between hormonal stimulation and the operation may have influenced surgical outcomes. So, the results of this study certainly can not be used as a reference for comparisons or indications for treatment.
The observation of the increased vascularity and therefore the probability of increased intraoperative bleeding in a human skin transplant model with the treatment of human foreskin with testosterone (30) has led to the termination of DHT treatment at least 1 month preoperatively (12).
As mentioned before, the current studies are still lacking in standardization of drug selection as well as the respective dose regimens and routes of administration. The concision of literature regarding hormonal stimulation limits providing a strict evaluation of the benefits of hormone therapy, the optimal hormone or the type of administration, and androgens really improve surgical outcome or not. A clear documentation of the hormonal agent, the dose and timing of the treatment as well as the criteria used to select patients for treatment is needed to standardize the use of hormonal stimulation before the surgery by means of further investigation.
Side effects
The use of human chorionic gonadotropin and androgens in the management of cryptorchidism and hypospadias provides evidence that hormonal manipulation is often clinically well tolerated. Although the previous studies relating to hormonal stimulation have shown an advantage with an increase in penile length and glans circumference, with no significant side effects (17), there are still some concerns regarding the potential negative side effects such as pubic hair growth and occasional aggressive behavior that reliably resolve with cessation of therapy (5).
Some transient side effects on child’s behaviour, appearance of pubic hair, the increased risk of preoperative bleeding as well as increased erections have been reported in a recent trial of systemic testosterone treatment (8). Studies that have not demonstrated a significant difference in penile length revealed a greater occurrence of the pigmentation of the genitals, pubic hair growth, and skin irritation at the site of application associated with topical use (7,12,14,15), suggesting that intramuscular hormone therapy is preferable to topical therapy (2).
Since topical medications is not absorbed through the gastrointestinal system, they don't undergo first pass hepatic metabolism and are associated with minimal side effects. On the other hand, the parenteral injection of hormones might limit parental compliance, particularly when injection of the hormone is not mandatory. It was reported that a bad early experience with injections may generate anxiety in children, which can make the next injection experience worse, resulting in pain (31). With the experience of a 3-month period, the secondary effects of transdermal DHT gel were minimal, and only complaints of irritating symptoms on the penile skin were reported in some children (12). One-third of our patients has experienced temporary pruritus and erythema, as well as darkening of the penile skin, which disappeared after treatment discontinuation.
None of the studies in a recent systematic review in which 283 patients received some form of hormonal treatment, revealed any persistent side effects related to hormonal stimulation (9). Of these studies, only a few had adequately compared complication rates, and the majority were of low methodological quality. In one study, dose related emesis in 1 of 12 patients receiving IM testosterone, leading to cessation of therapy was reported (15).
In the case of intraoperative and postoperative complications, the data in the literature is not homogeneous regarding description of complications. The studies that reported absence of intraoperative complications subjectively, have mainly referred to absence of important bleeding that was difficult to control (5,14).
Studies concerning over delay in bone age or accelerated linear height have not shown any evidence about the possible effects on bone maturation. But, further studies seem to be needed to determine bone age on a long-term basis (5-7,30).
Conclusions
Significant increase in penile length and glans circumference in hypospadiac children who received hormonal stimulation prior to repair has been revealed in some studies. In addition to functional outcome, a preliminary randomized study has suggested that DHT pretreatment is of use in improving cosmetic outcome.
Nevertheless, there is still a limited knowledge about the current practices of pediatric urologists in hormonal treatment before the surgery. Well designed randomized studies with similar patients in each group seem to be required to confirm that children receiving hormonal treatment have fewer complications than children who undergo surgery alone. These studies should include a larger number of patients and a placebo group, and penile size and hormone levels should be evaluated as objective measures of efficacy and safety.
In order to develop a treatment guideline of hormonal stimulation before hypospadias repair, continues investigation including the standardized dosing protocols of the agent, well reported technical details of procedures in patients classified according to severity of hypospadias must be reported.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Paoluzzi LJ. Is hypospadias an environmental birth defect? Dialogues Pediatric Urol 2000;23:2-4.
- Monfort G, Lucas C. Dehydrotestosterone penile stimulation in hypospadias surgery. Eur Urol 1982;8:201-3. [PubMed]
- Hypospadie Hohenfellner R. Akt Urol 1995;26:153-8.
- Immergut M, Boldus R, Yannone E, et al. The local application of testosterone cream to the prepubertal phallus. J Urol 1971;105:905-6. [PubMed]
- Gearhart JP, Jeffs RD. The use of parenteral testosterone therapy in genital reconstructive surgery. J Urol 1987;138:1077-8. [PubMed]
- Davits RJ, van den Aker ES, Scholtmeijer RJ, et al. Effect of parenteral testosterone therapy on penile development in boys with hypospadias. Br J Urol 1993;71:593-5. [PubMed]
- Nerli RB, Koura A, Prabha V, et al. Comparison of topical versus parenteral testosterone in children with microphallic hypospadias. Pediatr Surg Int 2009;25:57-9. [PubMed]
- Gorduza DB, Gay CL, de Mattos E. Does androgen stimulation prior to hypospadias surgery increase the rate of healing complications? - A preliminary report. J Pediatr Urol 2011;7:158-61. [PubMed]
- Wright I, Cole E, Farrokhyar F, et al. Effect of preoperative hormonal stimulation on postoperative complication rates after proximal hypospadias repair: a systematic review. J Urol 2013;190:652-59. [PubMed]
- Bastos AN, Oliveira LR, Ferrarez CE, et al. Structural study of prepuce in hypospadias--does topical treatment with testosterone produce alterations in prepuce vascularization? J Urol 2011;185:2474-8. [PubMed]
- Ishii T, Hayashi M, Suwanai A, et al. The effect of intramuscular testosterone enanthate treatment on stretched penile length in prepubertal boys with hypospadias. Urology 2010;76:97-100. [PubMed]
- Kaya C, Bektic J, Radmayr C, et al. The efficacy of dihydrotestosterone transdermal gel before primary hypospadias surgery: a prospective, controlled, randomized study. J Urol 2008;179:684-8. [PubMed]
- Luo CC, Lin JN, Chiu CH, et al. Use of parenteral testosterone prior to hypospadias surgery. Pediatr Surg Int 2003;19:82-4. [PubMed]
- Chalapathi G, Rao KL, Chowdhary SK, et al. Testosterone therapy in microphallic hypospadias: topical or parenteral? J Pediatr Surg 2003;38:221-3. [PubMed]
- Koff SA, Jayanthi VR. Preoperative treatment with human chorionic gonadotropin in infancy decreases the severity of proximal hypospadias and chordee. J Urol 1999;162:1435-9. [PubMed]
- Sakakibara N, Nonomura K, Koyanagi T, et al. Use of testosterone ointment before hypospadias repair. Urol Int 1991;47:40-3. [PubMed]
- Tsur H, Shafir R, Shachar J, et al. Microphallic hypospadias: testosterone therapy prior to surgical repair. Br J Plast Surg 1983;36:398-400. [PubMed]
- Baskin LS. Hypospadias and urethral development. J Urol 2000;163:951-6. [PubMed]
- Orkiszewski M. Dihydrotestosteron (DHT) local stimulation in hypospadias surgery. J Androl 1985;6:107.
- Wilson JD, Walker JD. The conversion of testosterone to 5 alpha-androstan-17 beta-ol-3-one (dihydrotestosterone) by skin slices of man. J Clin Invest 1969;48:371-9. [PubMed]
- Charmandari E, Dattani MT, Perry LA, et al. Kinetics and effect of percutaneous administration of dihydrotestosterone in children. Horm Res 2001;56:177-81. [PubMed]
- Gilliver SC, Ruckshanthi JP, Hardman MJ, et al. 5alpha-dihydrotestosterone (DHT) retards wound closure by inhibiting re-epithelialization. J Pathol 2009;217:73-82. [PubMed]
- Hamada K, Randall VA. Inhibitory autocrine factors produced by the mesenchyme-derived hair follicle dermal papilla may be a key to male pattern baldness. Br J Dermatol 2006;154:609-18. [PubMed]
- Freinkel RK. Other endocrine diseases. In: Freedberg IM, Eisen AZ, Wolff K, et al. eds. Fitzpatrick’s Dermatology in General Medicine. 5th ed. New York: McGraw-Hill, 1999:1976-86.
- Bush NC, DaJusta D, Snodgrass WT. Glans penis width in patients with hypospadias compared to healthy controls. J Pediatr Urol 2013;9:1188-91. [PubMed]
- Malik RD, Liu DB. Survey of pediatric urologists on the preoperative use of testosterone in the surgical correction of hypospadias. J Pediatr Urol 2014;10:840-3. [PubMed]
- Flatau E, Josefsberg Z, Reisner SH, et al. Letter: Penile size in the newborn infant. J Pediatr 1975;87:663-4. [PubMed]
- Mureau MA, Slijper FM, Nijman RJ, et al. Psychosexual adjustment of children and adolescents after different types of hypospadias surgery: a norm-related study. J Urol 1995;154:1902-7. [PubMed]
- Yerkes EB, Adams MC, Miller DA, et al. Coronal cuff: a problem site for buccal mucosal grafts. J Urol 1999;162:1442-4. [PubMed]
- Stern JM, Chen J, Peters SB, et al. Testosterone treatment of human foreskin in a novel transplant model. Urology 2004;63:999-1003. [PubMed]
- Fowler-Kerry S, Lander JR. Management of injection pain in children. Pain 1987;30:169-75. [PubMed]


