Pros, cons, and ethics of HPV vaccine in teens—Why such controversy?
Benefits of HPV vaccination (pros of vaccination)
Human papillomavirus (HPV) remains the most commonly sexually transmitted infection in both males and females. The current US estimate of new HPV infections is over 6.2 million cases each year (1,2). Many of these infections are asymptomatic and subclinical in nature, but certain viral serotypes have been implicated in causing cervical and penile carcinomas as well as anogenital, vulvar, vaginal, and oropharyngeal carcinomas. There are more than 150 documented HPV viruses with about 40 having potential transmission through sexual contact (3,4). Many infections are asymptomatic and cleared by the host immune system. The oncogenic viral types (HPV 16 and 18) and wart-causing viral types (HPV 6 and 11) are the targets for the quadrivalent vaccine (Gardasil®, Merck & Company, Whitehouse Station, New Jersey, USA). A bivalent vaccine for HPV 16 and 18 has been marketed for female vaccine programs (Cervarix®, GSK, Research Triangle Park, North Carolina, USA), but has not been as widely marketed. In the European market, viral types 16 and 18 account for more than 70% of cervical cancers (5). The cancers caused by these viruses can have devastating consequences including high morbidity and mortality. Unfortunately, the incidence of all of these primary cancer cases appears to be increasing (6). Approximately 40-50% of all penile tumors are caused by HPV infection with HPV 16, 18, and 6 identified as the predominant viral types in 30.8%, 6.6%, and 6.7% respectively. As noted by Backes, prophylactic vaccines targeting carcinogenic types HPV 16 and 18 could potentially reduce approximately one-third of incident squamous cell carcinomas of the penis (7,8). For genital warts in both males and females, HPV 6 and HPV 11 are the most common causative viral types. Despite wide adoption of Pap testing, almost 70% of cervical cancers are also associated with HPV 16 and 18 viral types. Male oropharyngeal cancers are highly associated with HPV 16 (9). Anal cancers are also highly associated with HPV 16 and 18 viral types. Two effective vaccines for the oncogenic HPV viral serotypes have been available for almost a decade after the initial administrative approval in June 2006. In 2011, the CDC extended the indications for universal use in male patients from ages 9-26 with additional regimens for catch-up dosing depending on age (10). In the USA, state-mandated immunization programs have increased the numbers of children vaccinated; however, there are states that do not mandate universal vaccination of school-age children for HPV. Only Virginia and the District of Columbia require HPV vaccination to attend school. Many other states [12] have adopted education programs and another 8 provide funding for vaccination. The remaining 29 states do not have specific mandates regarding the vaccine, but many eligible dependent children are able to obtain the vaccines through linkage with Medicaid or other state insurance programs (11). Despite these programs that include financial coverage of the vaccine, only about 37.6% of female patients and 13.9% of male patients who start the vaccine series actually complete the three prescribed doses within the 6-month time interval of administration as detailed from surveillance data from 2007-2013 (12). For females, the risk of cervical cancer and the potential for prevention of this devastating disease served as the impetus for widespread adoption of the vaccine. The increase in male genital lesions, penile cancer, as well as oropharyngeal and anogenital cancers helped extend the indications for this vaccine to both sexes up to the age of 26. There also documented benefits to male patients regarding a decrease in sexually-transmitted lesions from female sexual partners who have been vaccinated. Hariri has summarized the early evidence of population impact of HPV vaccines with moderate reductions in HPV associated pathology in the vaccinated groups (13). Specifically, Markowitz details a nationally representative survey that documents a 50% decrease in viral prevalence from the pre-vaccine years [2003-2006] to the post-vaccine era [2007-2010] (14). Many other studies detail the significant decline in the diagnosis of genital warts during this time frame as well. Preliminary data from Australia show that herd immunity may be an added benefit from the vaccine program (15). The ideal time to begin the vaccine series in both sexes is before the age of commencing sexual contact. In theory, this vaccination may help prevent the spread of genital warts in both sexes in addition to the cancer prevention rationale listed above. For some parents, this presents an ethical dilemma. The disease prevention benefits are easier to justify. For others, the vaccine is seen as a potential gateway to encouraging sexual contact at earlier ages or promoting higher risk sexual practices and, consequently, forms the basis of an argument to discourage the administration of the vaccine. For female patients, the argument that the vaccine will prevent cervical cancer appears far more persuasive than the counterargument of promoting earlier sexual activity and higher risk sexual practices. The most frequent parental reasons for not vaccinating teenage girls were summarized in the review by Darden et al. and stated the top reasons were that the girls with either not sexually active or a lack of knowledge about the vaccine (16). For parents of male patients, there also seems to be a relatively high rate of acceptance (by both parents and physicians) regarding the vaccine for male teenagers, but with less emphasis than females (17).
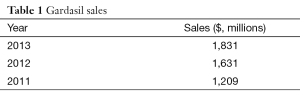
There is ongoing, active scientific inquiry and clinical trials to extend the vaccine to include activity against more of the oncogenic viral subtypes for cancers invading the oropharyngeal and anogenital regions. Merck has a 9-valent vaccine (V503) including 5 additional cancer-causing subtypes to increase activity against these types of cancer (18). Sales for the Gardasil vaccine have increased over the past 3 years (Table 1) (19). This measure serves as a surrogate for total vaccine doses produced by the pharmaceutical company. Numbers of patients actually vaccinated (either with a single initiation dose or complete series) are difficult to extrapolate. The current data regarding estimated HPV vaccination coverage among adolescent boys and girls aged 13-17 details an increase in completed vaccine series from 5.9% in 2007 to 37.6% in 2013 for girls and 1.3% to 13.9% in boys from 2011 to 2013 (20).
Full table
The Advisory Committee on Immunization Practices (ACIP), in concert with other professional associations, recommends the administration schedule of vaccines (21). Despite the annual recommendations, there is no national governing body to implement these recommendations. In the US, school vaccination requirements are generally decided by each state legislature. The CDC maintains federal Vaccines for Children (VFC) in all 50 states and provides vaccine and some state Medicaid programs also cover underinsured and uninsured children. Many states appear to endorse the administration of the vaccine, but neither mandate universal compliance nor provide adequate funding for the vaccine administration (22).
Despite these objections, the public health benefits of the vaccine and cost effectiveness have been validated in multiple studies. For female patients, the cervical cancer prevention with vaccine administration remains superior to cervical cancer screening programs employing Papanicolaou smears alone. In a systematic review of 29 studies by Seto and colleagues estimated that the addition of boys to the vaccination programs generally exceeds traditional cost-effectiveness thresholds ($50,000 per QALY). They concluded that studies consistently show that the HPV vaccines can have a substantial impact on the epidemiology of HPV disease (23). Only longer observation of trends over time will validate these conclusions.
Cons of HPV vaccine administration
The benefits of vaccine administration for HPV prevention have been summarized in the preceding section, but what are the risks and downsides to widespread adoption of the vaccination program? The CDC published a summary document of adverse events reported in JAMA for vaccine administration from time of approval in June 2006 to December 2008. The study also included patterns in adverse events reported to the Vaccine Adverse Event Reporting System (VAERS) and was the first nationwide published HPV post licensure study. (The findings were similar to safety reviews of other vaccines recommended for a similar age group [9-26] and compared to such vaccines as meningitis and Tdap). Overall, the vaccine continues to be safe and effective and concluded that benefits continue to outweigh its risks. The main findings are summarized below as compiled from the reports with updated data to the July 2014 report (24).
- More than 67 million doses were administered nationally since the HPV vaccine was licensed in June 2006 until March 2014. There were 25,176 reports to VAERS of adverse events.
- About 92.4% of the adverse events were not serious. Adverse events are considered serious if it is life threatening, or results in death, permanent disability, abnormal conditions at birth, hospitalization or prolonged administration.
- The most common events reported (for both male and female patients) were:
- Syncope (or fainting)-common after needle injections, especially in pre-teens and teens;
- Local reactions at the site of immunization (pain and redness);
- Dizziness;
- Nausea;
- Headache.
- In the first report, there were 12,424 reports of adverse events 772 (6% of all reports) described serious adverse events including 32 reports of death. The most recent report from June 2006-June 2013 reported 85 deaths after the vaccine. Upon further screening of the reported deaths, there were no common patterns to the deaths that would suggest that they were caused by the vaccine. Some of the deaths were attributable to diabetes, viral illness, illicit drug use, and heart failure.
- There were two reports of unusual neurological illness that were variants of Amyotrophic Lateral Sclerosis (ALS) that resulted in the deaths of two young females. This finding is being evaluated by several highly regarded academic centers.
- There was increased reporting of syncope and pulmonary emboli compared to other vaccines given to females of the same age. Of the people who had blood clots, 90% had a known risk factor for blood clots, such as taking oral contraceptives. The VAERS reports cannot prove the vaccine caused the adverse event in women with these risk factors.
A follow-up report authored by Bednarczyk et al. reviewed the trends in HPV vaccination from the National Immunization Survey-Teen, 2008-2011 and concluded that minority and below-poverty adolescents consistently had higher series initiation than white and above-poverty adolescents. For the uptake of at least one dose of the vaccine, rates increased from 37.2% of adolescent females ages 13-17 to 53% in 2011 with an average annual increase of 5.2%. Federally funded programs covering Medicaid beneficiaries most likely account for the increased coverage of the minority and below-poverty adolescents (25). Parental resistance to vaccination appears to be increasing with 44% of parents in 2010 said they did not intend to vaccinate their children (26). The resistance to vaccination appears to be related to the education of both healthcare providers and parents regarding the side effects of the vaccination and the ethical issues relating to human sexuality. The top five reasons for parents not vaccinating adolescents with the HPV vaccine are lack of knowledge, not needed or necessary, safety concerns/side effects, not recommended, and not sexually active (27). Clearly, there is room for more education and counseling to improve the acceptance of the vaccine series.
Ethical and practical considerations
From the epidemiological perspective, widespread adoption of universal vaccination against HPV has strong supporting evidence. Worldwide, HPV infection is responsible for half a million cases of cancer and more than 250,000 deaths every year (28,29). The highest incidence of the virus is occurs in developing countries that do not have resources to promote prevention or insure adequate treatment of the disease. The current worldwide scope of vaccination is greater than 120,000,000 people worldwide being vaccinated since the introduction of the vaccines in 2006. The relatively minor side effects of the vaccine seem to be worth the almost 100% effectiveness in preventing pre-cancerous lesions caused by the HPV oncogenic viral subtypes (HPV-6, 11, 16, and 18). To date, none of the deaths that occurred after vaccine administration have been directly linked to the vaccine. In June 2013, Japan became the only country to cease the active promotion of the vaccine for patients until more studies related to the incidence of side effects could be completed (30).
Navarro-Illano and colleagues published a thought-provoking summary debate regarding the ethical considerations of universal vaccination against HPV in 2014 since the country of Spain was considering the adoption of an HPV vaccine program (31). Several ethical issues are highlighted in their analysis including whether to vaccinate people who have opted to abstain from sex and whether obtaining the vaccine increases the early onset of sexual relations (32). In the first instance, absolute sexual abstinence is a very difficult parameter to measure especially in the early age group that has been targeted for the initial vaccination series. From a more scientific perspective, the antibody titer generated at the younger age appears to be highest between the ages of 9-14. Aside from the physical process of vaccination, the more important issues influencing the success of these programs are the educational components that counsel patients and parents regarding the initiation of sexual activity as well as the awareness of the serious health consequences of HPV infection (33). These programs are not successful in isolation and need the educational component to help decrease other higher risk sexual behaviors. Parents and physicians need to remain actively involved in the education process and continue to advocate for the children. Similarly, the parents ultimately retain the right to decide whether or not to vaccinate their children.
The ethical arguments also extend to the manufacturers of the HPV vaccines. The research costs for bringing a successful product to market are usually quite high. Successful programs require a balance such that commercial products are safe and effective and that continued research occurs to perpetuate the cycle of new viable products. Only continued time and monitoring will document the success of these programs worldwide. The practical aspects of recommending HPV vaccine to parents and patients are probably more important than the ethical issues with any type of vaccination program. As summarized by Holman, physicians and parents cite different barriers to the vaccine. Physicians cite financial concerns and parental attitudes and concerns, while most parents need more information about the vaccine before they will consent to administration (34). As with most other interventions, the parents look to the clinician for the ultimate recommendation to vaccinate.
Conclusions
The goal of this article has been to review the benefits and risks of HPV vaccination in teenagers and pre-teenagers as well as a brief review of some of the more important ethical and practical issues that influence the widespread adoption of the vaccine. The overwhelming evidence favors administration of the vaccine to prevent the precancerous and malignant disease conditions caused by HPV infection. The risks of the vaccine are within the range of complications noted with other vaccination programs that have been maintained for decades. Only time will document whether inclusion of both males and females will induce additional herd immunity that ultimately protects a wider proportion of the population or not. Pediatric urologists and pediatricians remain on the “front lines” in informing patients and parents regarding the benefits of HPV vaccination and need to keep informed about the benefits of the vaccine. With better education, practicing urologists can help increase the numbers of children who complete the HPV vaccine and work to decrease the disease burden of HPV-related diseases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Anic GM, Giuliano AR. Genital HPV infection and related lesions in men. Prev Med 2011;53 Suppl 1:S36-41. [PubMed]
- Smith JS, Gilbert PA, Melendy A, et al. Age-specific prevalence of human papillomavirus infection in males: a global review. J Adolesc Health 2011;48:540-52. [PubMed]
- Low GM, Attiga YS, Garg G, et al. Can male vaccination reduce the burden of human papillomavirus-related disease in the United States? Viral Immunol 2012;25:174-86. [PubMed]
- Gravitt PE. The known unknowns of HPV natural history. J Clin Invest 2011;121:4593-9. [PubMed]
- Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 2003;348:518-27. [PubMed]
- Moscicki AB, Palefsky JM. Human papillomavirus in men: an update. J Low Genit Tract Dis 2011;15:231-4. [PubMed]
- Miralles-Guri C, Bruni L, Cubilla AL, et al. Human papillomavirus prevalence and type distribution in penile carcinoma. J Clin Pathol 2009;62:870-8. [PubMed]
- Backes DM, Kurman RJ, Pimenta JM, et al. Systematic review of human papillomavirus prevalence in invasive penile cancer. Cancer Causes Control 2009;20:449-57. [PubMed]
- van Monsjou HS, van Velthuysen ML, van den Brekel MW, et al. Human papillomavirus status in young patients with head and neck squamous cell carcinoma. Int J Cancer 2012;130:1806-12. [PubMed]
- Recommendations on the Use of Quadrivalent Human Papillomavirus Vaccine in Males — Advisory Committee on Immunization Practices (ACIP), 2011. Morbidity and Mortality Weekly Report 2011;60:1705-8. (MMWR). [PubMed]
- The HPV Vaccine: Access and Use in the U.S. Available online: http://kaiserfamilyfoundation.files.wordpress.com/2014/03/7602-04-the-hpv-vaccine-access-and-use-in-the-u-s.pdf
- Centers for Disease Control and Prevention (CDC). National, state, and local area vaccination coverage among adolescents aged 13-17 years--United States, 2008. MMWR Morb Mortal Wkly Rep 2009;58:997-1001. [PubMed]
- Hariri S, Markowitz LE, Dunne EF, et al. Population impact of HPV vaccines: summary of early evidence. J Adolesc Health 2013;53:679-82. [PubMed]
- Markowitz LE, Hariri S, Lin C, et al. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003-2010. J Infect Dis 2013;208:385-93. [PubMed]
- Moscicki AB, Palefsky JM. Human papillomavirus in men: an update. J Low Genit Tract Dis 2011;15:231-4. [PubMed]
- Darden PM, Thompson DM, Roberts JR, et al. Reasons for not vaccinating adolescents: National Immunization Survey of Teens, 2008-2010. Pediatrics 2013;131:645-51. [PubMed]
- Liddon N, Hood J, Wynn BA, et al. Acceptability of human papillomavirus vaccine for males: a review of the literature. J Adolesc Health 2010;46:113-23. [PubMed]
- Merck & Company, 2013 Annual Report, page 9. Accessed online: merck.com/investor, 17 July 2014.
- Merck & Company, 2013 Annual Report, page 42. Accessed online: merck.com/investor, 17 July 2014.
- Stokley S, Jeyarajah J, Yankey D, et al. Human Papillomavirus Vaccination Coverage Among Adolescents, 2007–2013, and Postlicensure Vaccine Safety Monitoring, 2006–2014 — United States. Morbidity and Mortality Weekly Report 2014;63:620-4. (MMWR). [PubMed]
- Centers for Disease Control and Prevention (CDC). Recommended childhood immunization schedule--United States, January-June 1996. MMWR Morb Mortal Wkly Rep 1996;44:940-3. [PubMed]
- National Council of State Legislatures, chapter on HPV Vaccine. Available online: http://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx. [accessed 2014 May 14].
- Seto K, Marra F, Raymakers A, et al. The cost effectiveness of human papillomavirus vaccines: a systematic review. Drugs 2012;72:715-43. [PubMed]
- Human Papillomavirus (HPV) Vaccine. Available online: https: www.cdc.gov/vaccinesafety/Vaccines/HPV/jama.html. [accessed 17 July 2014].
- Bednarczyk RA, Curran EA, Orenstein WA, et al. Health disparities in human papillomavirus vaccine coverage: trends analysis from the National Immunization Survey-Teen, 2008-2011. Clin Infect Dis 2014;58:238-41. [PubMed]
- Fiks AG, Grundmeier RW, Mayne S, et al. Effectiveness of decision support for families, clinicians, or both on HPV vaccine receipt. Pediatrics 2013;131:1114-24. [PubMed]
- Holman DM, Benard V, Roland KB, et al. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014;168:76-82. [PubMed]
- Ferlay J, Bray F, Pisani P, et al. GLOBOCAN 2002. Cancer incidence, mortality and prevalence worldwide IARC CancerBase No. 5 [Internet]. Version 2.0. Lyon: IARC Press. 2004. Available online: http://www-dep.iarc.fr/
- GLOBOCAN 2012, Cancer Incidence, Mortality, and Prevalence Worldwide in 2012, International Agency for Research on Cancer, World Health Organization. Accessed at globocan.iarc.fr/Pages/summary_table_site_sel.aspx. iarc.fr on 17 July 2014. Incidence of cervical cancer noted to be 527,624 cases reported worldwide.
- Merck & Company, 2013 Annual Report, page. 48. Accessed online: merck.com/investor, 17 July 2014.
- Navarro-Illana P, Aznar J, Díez-Domingo J. Ethical considerations of universal vaccination against human papilloma virus. BMC Med Ethics 2014;15:29. [PubMed]
- Charo RA. Politics, parents, and prophylaxis--mandating HPV vaccination in the United States. N Engl J Med 2007;356:1905-8. [PubMed]
- Allison MA, Dunne EF, Markowitz LE, et al. HPV vaccination of boys in primary care practices. Acad Pediatr 2013;13:466-74. [PubMed]
- Holman DM, Benard V, Roland KB, et al. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014;168:76-82. [PubMed]


