
Incidence and preoperative predictors for major complications following radical nephroureterectomy
Introduction
Upper tract urothelial carcinoma (UTUC) is an uncommon genitourinary cancer that accounts for only 5% of all urothelial tumors (1). UTUC is three times more common in men (than women) and primarily affects elderly patients with peak incidence occurring after the 7th decade of life (2,3). Known risk factors for UTUC include smoking, cyclophosphamide use, aristolochic acid exposure, occupational hazards, chronic inflammation, and a history of bladder cancer (3). UTUC is particularly aggressive, with high rates of recurrence and progression, with over 60% of patients presenting with muscle invasion at time of diagnosis (4,5). Tumor stage and grade are the most established and reproducible prognostic factors in patients with UTUC (5,6). Radical nephroureterectomy (RNU) remains the gold standard for management of bulky, invasive, or high grade UTUC with overall 5-year recurrence-free and cancer-specific survival probabilities of 69% and 73%, respectively (6).
Endoscopic ablative techniques are an attractive option in select patients with pathologic low-grade and/or low burden UTUC, or in patients unable to tolerate extirpative surgery. There are, however, no randomized clinical trials comparing endoscopic management with RNU. Admittedly, those patients treated endoscopically have higher rates of ipsilateral upper-tract recurrence as well as bladder cancer (7). Nonetheless, up to 38% of patients of RNU patients develop a complication, and prior retrospective studies have identified a significant reduction in mean GFR, thereby limiting the role of adjuvant chemotherapy for locally advanced disease (8,9). Associated GFR decline further increases the potential for cardiovascular and all-cause mortality.
Many patients undergoing RNU are older and harbor multiple comorbidities which place them at increased risk for postoperative complications. Preoperative nomograms have been constructed to better objectify the risk associated with RNU (9). This prior work has focused on all complications events that a patient may experience. Yet, the association between preoperatively measured patient-specific factors and major complications following RNU (which likely will impact convalescence and recovery) is less clear.
This study reviews a multi-center cohort of RNU patients to identify the incidence of major complications as well as preoperative risk factors for their occurrence. Such information may improve patient counseling as well as present evidence to encourage less invasive treatment options when appropriate and applicable.
Methods
The charts of 1,266 patients with clinically localized, non-metastatic, upper-tract urothelial carcinoma (UTUC) undergoing RNU at 14 academic medical centers between 2002 and 2015 were reviewed. RNU was performed via either an open or minimally invasive approach with regional lymphadenectomy and specific bladder cuff management at the discretion of the operating surgeon. All specimens were confirmed as urothelial carcinoma on pathologic review. Preoperative clinical, demographic, and select patient-specific comorbidities were collected for analysis.
Perioperative complications occurring within 30 days of surgery were graded using the modified Clavien-Dindo classification scale (10). The number, type, and severity of all complications were included. In accordance with standard reporting scales, major complications were classified as Clavien grade ≥ III, while minor complications were Clavien grade ≤ II. Univariate and multivariate logistic regression analysis determined the association between preoperative variables and Clavien III or greater post-RNU complications. A multivariable model included all possible preoperative predictors, including age, race, gender, ECOG performance status, Charlson Comorbidity Index (CCI), American Society of Anesthesiologists (ASA) score, body mass index, individual comorbidities, and receipt of neoadjuvant chemotherapy. Importantly, in this study, we specifically focused on preoperative patient characteristics as opposed to surgical approach or intraoperative events. The rationale was to specifically provide information to practicing urologists regarding preoperative baseline comorbidities which could be ascertained in the office which would impact patient outcomes following RNU. A P value of <0.05 was set as significance.
Results
Table 1 highlights the clinicopathologic characteristics of those patients undergoing RNU. A total of 1,266 patients (707 men and 559 women) with a median age of 70 years and body mass index of 27 kg/m2 were included. Over three-quarters of the cohort was Caucasian, approximately 50% had an ASA score >3, 22% had a CCI score >5, and 17% had an Eastern Cooperative Oncology Group (ECOG) performance status ≥2. Of those patients included, 54.3% had hypertension, 50.1% had baseline chronic kidney disease (CKD) stage III or worse, 37.3% had hyperlipidemia, 20.8% had coronary artery disease, 17.1% had diabetes mellitus, and 14% had baseline pulmonary disease. Only 7.1% of patients received neoadjuvant chemotherapy.
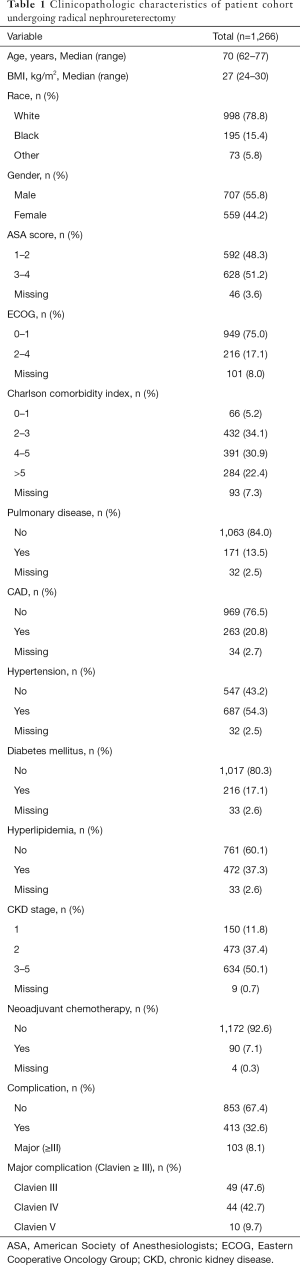
Full table
Four hundred and thirteen patients (32.6%) experienced a complication including 103 (8.1%) patients with a major (Clavien grade III or higher) complication. The specific distribution of major complications included 49 Clavien III (47.6%), 44 Clavien IV (42.7%), and 10 Clavien V (9.7%) adverse events. The distribution of major complications included bleeding/hemorrhage (n=22; 21%), hematologic (n=20; 19%), gastrointestinal (n=19, 18%), infectious (n=19; 18%), cardiovascular (n=16; 16%), and pulmonary (n=7; 7%). Hematologic complications were predominantly venous thrombosis (n=9) or pulmonary embolism (n=7), Gastrointestinal complications included bowel obstruction (n=10), prolonged ileus (n=7), and perforated viscus (n=2).
Table 2 summarizes the univariate model for major complications in patients following RNU. On univariate analysis, patient age (P=0.006), performance status indices [ASA score (P=0.022), ECOG (P<0.001), CCI (P<0.001)], hypertension (P=0.002), diabetes mellitus (P=0.023), and CKD stage (P<0.001) were all associated with major complications. Conversely, major complications were not associated with increased BMI (P=0.251), race (P=0.320), gender (P=0.349), pulmonary disease (P=0.547), coronary artery disease (P=0.536), hyperlipidemia (P=0.176), or receiving neoadjuvant chemotherapy (P=0.609).
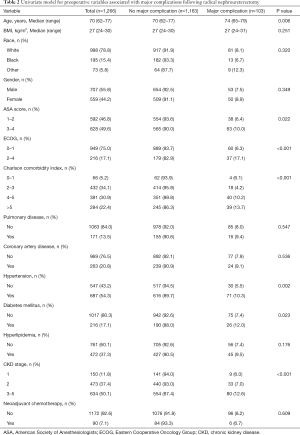
Full table
Table 3 highlights the multivariable model for major complications following RNU. On multivariate analysis, ECOG ≥2 (OR 2.38, 95% CI, 1.46–3.90, P=0.001), CCI >5 (OR 3.45, 95% CI, 1.41–8.33, P=0.007), and CKD stage ≥3 (OR 3.64, P=0.008) were independently associated with major complications. Patient age (P=0.422), ASA score (P=0.180), hypertension (P=0.748), and diabetes mellitus (P=0.594), however, were not.
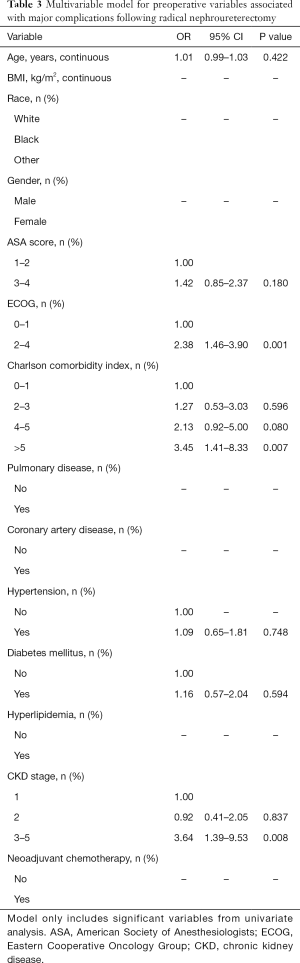
Full table
Discussion
While RNU with excision of ipsilateral bladder cuff is the gold-standard therapy for patients with UTUC and normal contralateral kidney function, there remains a significant risk of perioperative complication due to pre-existing medical comorbidities in this patient population (8,9). In the present study of almost 1,300 patients undergoing RNU at 14 academic medical centers, 413 patients (32.6%) experienced a complication including 103 (8.1%) patients with a Clavien grade III or higher complication. Of these 103 patients with major complications, 49 were Clavien III (47.6%), 44 were Clavien IV (42.7%), and 10 patients suffered Clavien V (9.7%) mortality events. The rate of major complications in this large series is similar to prior studies, but slightly higher than those reported in a systematic review of laparoscopic RNU versus open technique for management of UTUC (4.6% vs. 3.8%, respectively) (11-13). We hypothesize this may be attributable to the inherent case mix bias that is seen at tertiary care academic medical centers.
This study identified several patient-specific factors as independent predictors of perioperative complications. On univariate analysis, patient age (P=0.006), ASA score (P=0.022), ECOG performance status (P<0.001), CCI (P<0.001), hypertension (P=0.002), diabetes mellitus (P=0.023), and CKD stage (P<0.001) were all associated with major complications following RNU. On multivariate analysis, only ECOG ≥2 (OR 2.38, P=0.001), CCI >5 (OR 3.45, P=0.007), and CKD stage ≥3 (OR 3.64, P=0.008) were independently associated with major complications. These findings show concordance from observations noted in prior work. Specifically, a previous multi-institutional study with 427 patients determined ECOG performance status was associated with perioperative mortality and worse overall survival (14). Another multi-institutional study involving 731 patients identified patient age, race, ECOG, CCI, and CKD as independent predictive factors of all complications following RNU, and these patient-specific variables were used to construct a preoperative nomogram to predict complications within 30 days for UTUC (9). The results of the current study involving 1,266 patients from 14 academic medical centers highlights performance status and increased CKD stage as independent predictors of major complications following RNU. Other patient-specific factors, including BMI, ASA score, hypertension, and diabetes mellitus were not associated with major complications.
These observations improve our ability to counsel patients diagnosed with this uncommon malignancy. Indeed, while RNU remains the reference for management of UTUC, urologists must recognize the reality of treatment related morbidity. In that regard, conservative therapies may present a viable (and possibly safer) option in those patients with lower risk disease. Indeed, improved risk stratification and refinements in the ability to deliver adjuvant intracavitary therapies may further enhance the effectiveness of kidney preserving UTUC procedures.
We recognize that our analysis focused on preoperative factors that are associated with major complications. Indeed, we elected not to incorporate operative variables such as surgical approach for several reasons. Firstly, in retrospective studies, surgical approach is inherently impacted by surgeon expertise and case selection bias. Indeed, large series from population based administrative datasets provide conflicting data likely due unmeasured factors (15,16). Secondly, we sought to specifically explore factors that could be measured prior to the operative procedure. These factors would be most beneficial in counseling and expectations prior to a decision of a surgical approach. Finally, if one considers surgical approach, then an array of other operative factors merit inclusion such as lymphadenectomy (and extent) and ipsilateral bladder cuff management. Individually, each surgical nuance presents its own associated benefits and risks. Therefore, analysis did not factor these variables.
Several limitations of this study warrant mention. The retrospective and multicenter design could contribute to variable accuracy and annotation in grading complications and how these complications are managed at each institution. Secondly, these experiences also reflect academic urologic practices and therefore may be subject to referral bias with regards to surgeon expertise as well as patient comorbidity profile. Nonetheless, despite these limitations, this is the largest cohort to date of UTUC patients undergoing radical surgery and the first to report impaired baseline performance status and increasing CKD stage as independent variables in developing major postoperative complications following RNU.
Conclusions
Major complications occur in 8% of patients undergoing RNU. Impaired preoperative performance status (as determined by ECOG or CCI) and baseline CKD are associated with major postoperative adverse events. These easily measurable indices warrant consideration prior to proceeding with RNU.
Acknowledgments
Funding: The study was supported by The Keith and Lynda Harring Fund for Urologic Research at Penn State Health.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (John J. Knoedler and Jay D. Raman) for the series “Upper-Tract Urothelial Carcinoma: Current State and Future Directions” published in Translational Andrology and Urology. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau.2020.01.22). The series “Upper-Tract Urothelial Carcinoma: Current State and Future Directions” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Penn State College of Medicine Institutional Review Board and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Raman JD, Messer J, Sielatycki JA, et al. Incidence and survival of patients with carcinoma of the ureter and renal pelvis in the USA, 1973-2005. BJU Int 2011;107:1059-64. [Crossref] [PubMed]
- Shariat SF, Favaretto RL, Gupta A, et al. Gender differences in radical nephroureterectomy for upper tract urothelial carcinoma. World J Urol 2011;29:481-6. [Crossref] [PubMed]
- Rouprêt M, Babjuk M, Comperat E, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2017 Update. Eur Urol 2018;73:111-22. [Crossref] [PubMed]
- Margulis V, Shariat SF, Matin SF, et al. Outcomes of Radical Nephroureterectomy: A Series From the Upper Tract Urothelial Carcinoma Collaboration. Cancer 2009;115:1224-33. [Crossref] [PubMed]
- Lughezzani G, Burger M, Margulis V, et al. Prognostic Factors in Upper Urinary Tract Urothelial Carcinoma: A Comprehensive Review of the Current Literature. Eur Urol 2012;62:100-14. [Crossref] [PubMed]
- Leow JJ, Orsola A, Chang SL, et al. A contemporary review of management and prognostic factors of upper tract urothelial carcinoma. Cancer Treat Rev 2015;41:310-9. [Crossref] [PubMed]
- Yakoubi R, Colin P, Seisen T, et al. Radical nephroureterectomy versus endoscopic procedures for the treatment of localised upper tract urothelial carcinoma: a meta-analysis and a systematic review of current evidence from comparative studies. Eur J Surg Oncol 2014;40:1629-34. [Crossref] [PubMed]
- Raman JD, Lin YK, Kaag M, et al. High rates of advanced disease, complications, and decline of renal function after radical nephroureterectomy. Urol Oncol 2014;32:47.e9-14. [Crossref] [PubMed]
- Raman JD, Lin YK, Shariat SF, et al. Preoperative nomogram to predict the likelihood of complications after radical nephroureterectomy. BJU Int 2017;119:268-75. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Lin YK, Deliere A, Lehman K, et al. Critical analysis of 30 day complications following radical nephroureterectomy for upper tract urothelial carcinoma. Can J Urol 2014;21:7369-73. [PubMed]
- Rajput MZ, Kamat AM, Clavell-Hernandez J, et al. Perioperative outcomes of laparoscopic radical nephroureterectomy and regional lymphadenectomy in patients with upper urinary tract urothelial carcinoma after neoadjuvant chemotherapy. Urology 2011;78:61-7. [Crossref] [PubMed]
- Ni S, Tao W, Chen Q, et al. Laparoscopic Versus Open Nephroureterectomy for the Treatment of Upper Urinary Tract Urothelial Carcinoma: A Systematic Review and Cumulative Analysis of Comparative Studies. Eur Urol 2012;61:1142-53. [Crossref] [PubMed]
- Martinez-Salamanca JI, Shariat SF, Rodriguez JC, et al. Prognostic role of ECOG performance status in patients with urothelial carcinoma of the upper urinary tract: an international study. BJU Int 2012;109:1155-61. [Crossref] [PubMed]
- Hanske J, Sanchez J, Schmid M, et al. A comparison of 30-day perioperative outcomes in open versus minimally invasive nephroureterectomy for upper tract urothelial carcinoma: analysis of 896 patients from the American College of Surgeons – National Surgical Quality Improvement Program Database. J Endourol 2015;29:1052-58. [Crossref] [PubMed]
- Nazzani S, Bazinet A, Preisser F, et al. Comparison of perioperative outcomes between open and minimally invasive nephroureterectomy: a population based analysis. Int J Urol 2019;26:487-92. [Crossref] [PubMed]


