Updates on sperm retrieval techniques
Introduction
Infertility affects a substantial portion of couples worldwide with multiple studies showing approximately 15% of couples experiencing infertility (1,2). Of these infertile couples, approximately 50% will have a male factor, and 20% will be due solely to male factor (3). In the most severe forms of male factor infertility, the male partner is completely azoospermic, defined as no sperm is found on semen analysis even after centrifugation on two completely collected specimens separated by at least one month. The incidence of azoospermia is estimated to be 1.9% (4) in the general population and 15% of infertile men (5).
With the advent of intracytoplasmic sperm injection (ICSI), it became possible to offer paternity to men who had previously been unable to achieve biological paternity on their own, namely men with non-obstructive azoospermia. It also became possible to offer men with obstructive azoospermia an alternative route to paternity other than microsurgical reconstruction of the reproductive tract. As such, surgical sperm retrieval techniques have allowed the majority of azoospermic men with both obstructive and non-obstructive azoospermia a viable and minimally invasive means towards biological paternity. The goal of all sperm retrieval techniques is to obtain spermatozoa that can be used with assisted reproductive techniques. The determination of which procedure is ideal for each patient is due to a number of factors including cause of azoospermia, availability of a skilled microsurgeon, cost of procedure, operating room availability, timing of the in vitro fertilization (IVF) cycle, number of children desired, yield of sperm needed, and patient desire. While the decision to proceed with surgical sperm retrieval and assisted reproduction is complex, it is clear that microsurgical techniques offer tremendous benefit over non-microsurgical approaches in sperm retrieval. This article examines the current options available for sperm retrieval and for whom they are best suited.
Obstructive azoospermia
Obstructive azoospermia is a condition characterized by normal levels of spermatogenesis but an inability of the sperm to reach the ejaculate due to a blockage. Obstruction of the reproductive tract may be congenital or acquired. Causes of obstructive azoospermia include vasectomy, congenital bilateral absence of the vas deferens, ejaculatory duct obstruction, idiopathic, or iatrogenic obstruction from surgeries such as inguinal hernia repair, radical pelvic surgery, hydrocelectomy, orchidopexy, or failed vasectomy reversal. Vasectomy is the most common cause in the United States, and it is estimated that 175,000 to 354,000 vasectomies are performed each year in United States. While vasectomy reversal is the topic of another review, vasectomized men also have the choice of surgical sperm retrieval coupled with IVF with intracytoplasmic sperm injection (IVF-ICSI) for their female partner. In fact, for nearly all men with obstructive azoospermia, treatment options include either microsurgical reconstruction or surgical sperm retrieval coupled with IVF-ICSI.
In general, an obstructed reproductive system has high levels of sperm production. Epididymal fluid obtained from an obstructed system will have high yields of sperm of up to a million spermatozoa per microliter of fluid. While IVF-ICSI success rates between testicular and epididymal sperm may vary by reproductive center, it is indisputable that extraction of sperm from the epididymis can potentially lead to higher yields of spermatozoa. However, in the obstructed reproductive system, the concept of “inverted motility” applies and means that higher quality sperm are found more proximally in the reproductive tract than distally, where macrophage activity is higher and sperm quality is lower (6). Therefore, the best location for high yields of good quality sperm is the proximal epididymis in the obstructed system. We will now discuss the techniques of sperm retrieval in patients with obstructive azoospermia. A summary table of the relative advantages and disadvantages can be found in Table 1.
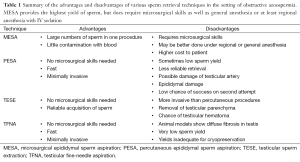
Full table
Percutaneous sperm retrieval techniques
Multiple percutaneous techniques are available to retrieve sperm, including fine needle aspiration of the testis (TFNA), percutaneous epididymal sperm aspiration (PESA), and percutaneous biopsy of the testis (PercBiopsy). Open testicular sperm retrieval is also a viable option (whether single biopsy or multiple biopsy). All of these techniques do not require microsurgical skill, and most can be performed under local anesthesia or with IV sedation.
Testicular fine-needle aspiration (TFNA)
Of the percutaneous sperm retrieval techniques, TFNA is the least technically challenging but yields the lowest number of sperm. Local anesthesia is applied to scrotal skin and a spermatic cord block is performed. The surgeon uses his thumb and forefinger to stabilize the testis before inserting the needle along the long axis. Seminiferous tubules must be disrupted in order to obtain sperm in this technique. Therefore, the needle is repeatedly withdrawn slightly and redirected until testicular material is aspirated. A Franzen needle holder can be used to provide negative pressure for the aspiration. However, we do not favor this approach because of the low yield of sperm obtained and the possibility of progressive testicular damage caused by TFNA. Shufaro et al. utilizing a rat model demonstrated progressive and irreversible damage to the testicular architecture, coagulative necrosis, degeneration of seminiferous tubules, destruction of Sertoli cells, and chronic inflammation. The amount of damage positively correlated to the number of punctures performed (7). Notably though, human data on this is lacking.
Percutaneous epididymal sperm aspiration (PESA)
PESA is a procedure that does not require microsurgical skill and can be done under local anesthesia to obtain epididymal sperm for use with assisted reproduction. A butterfly needle is pre-flushed with sperm media and attached to a syringe with a small volume of media. The head of the epididymis is stabilized between the thumb and forefinger and the butterfly needle is inserted along the long axis of the epididymis no more than one third of the way down. The needle is then slowly withdrawn with negative pressure until milky white fluid is seen in the tubing, at which point the tubing is clamped with a hemostat and the system then flushed out into a collection tube. Multiple passages can be performed until adequate sperm yield is attained.
The benefits of PESA includes its high success rate in obtaining sperm, with 84% success rate in obtaining motile sperm or rare motile sperm specimens in one series (8). In addition, PESA is a relatively simple procedure, does not require microsurgical training, and can be done under local anesthesia. However, the negative aspects of the procedure include the concern that the procedure may cause extensive epididymal fibrosis, making future attempts at PESA more difficult and precluding any possibility of microsurgical reconstruction in the future. Pasqualotto et al., in a study of patients who underwent repeat PESA for assisted reproduction, found that only 26% of patients had sperm found on repeat PESA. This is presumably due to epididymal scarring, and may suggest that PESA can be more harmful to the epididymis than its “minimally invasive” nature would suggest (9). Other drawbacks include the blind nature of the procedure, the variable sperm yield, and the difficulty in managing such small samples with butterfly needles and IV tubing. Also, specimens may easily be contaminated with blood given the blind nature of the procedure, which can negatively affect sperm quality. Finally, as the blood supply of the testis runs through the epididymis in this region, there is also the danger of inadvertent damage to the blood supply by the blindly inserted butterfly needle. Overall, while simple and not without its benefits, the variability in the yield of sperm, the likelihood of contamination of the sample with blood, and the danger of damage to the testicular blood supply make PESA a procedure not without significant risk.
Percutaneous testicular needle biopsy (Percbiopsy)
Another option for percutaneous sperm retrieval is needle biopsy of the testis using a 14-gauge biopsy gun with short excursion. It can be performed under local anesthesia with a spermatic cord block. With this method multiple biopsies can be obtained from a single entry site. Percutaneous needle biopsies yield a higher number of sperm than TFNA but fewer and lower quality than microsurgical epididymal sperm aspiration (MESA) (10). Similar to all the percutaneous procedures, this is a blind procedure and the chance of a post-procedure hematoma is not insignificant especially given the larger bore of biopsy guns generally used. Finally, the small testicular tissue samples are difficult to handle and an assistant is often needed to unload the sample and prepare the gun while the surgeon stabilizes the testis to use the same entry site for more biopsies.
Testicular sperm extraction (TESE)
Conventional TESE can also be performed in the setting of obstructive azoospermia. This technique provides several advantages in this setting. Under ideal conditions and in a truly obstructive azoospermic patient we would expect nearly 100% sperm retrieval rate. Microsurgical skills are not needed and this can be performed quickly and conveniently under local anesthesia in the surgeon’s office. In general, we perform these in the office under local anesthesia (spermatic cord block with scrotal skin block). Our technique is to make a small window in the scrotal skin using no-scalpel techniques until we reach the tunica vaginalis. Once this layer is reached we place two holding sutures through the tunica vaginalis using taper needles through the tunica vaginalis and the tunica albuginea. An incision is then made with a scalpel through the tunica vaginalis and the tunica albuginea and a small amount of testicular tissue is harvested. After hemostasis is obtained using bipolar electrocautery, the tunica albuginea, Dartos fascia, and skin are closed with the appropriate sutures. We have found that patients tolerate it exceedingly well and we like the ability to verify hemostasis visually before closing the small window in the scrotum.
Microsurgical epididymal sperm aspiration (MESA)
MESA is a microsurgical procedure in which individual epididymal tubules are isolated and micropunctured, either with a pulled glass pipette or an ophthalmic ultrasharp microknife. It is the preferred approach to harvest sperm in patients with obstructive azoospermia. Of all surgical sperm retrieval techniques, it yields the highest number of sperm, far greater than any percutaneous procedure (10). With yields ranging from 15-99 million sperm, MESA provides a sufficient quantity for effective cryopreservation into multiple aliquots with high yields of motile sperm (10,11). In addition, with direct microsurgical visualization of the epididymis and its puncture sites, it allows minimal contamination of samples with blood (which is toxic to sperm) and reduces the risk of other damage to epididymis and the blood supply to the testis.
MESA allows the surgeon to sample multiple sites or different epididymal tubules for selection of the site with the best quality sperm. The ideal initial target is an amber dilated epididymal tubule located about halfway up the obstructed reproductive segment. A small portion of the sample from each puncture is analyzed for sperm motility and, ideally, a test freeze should be done on an aliquot of the sample. If good quality sperm are not found at that site, or there is poor quality on test-freeze, successive micropuncture can be performed more proximally toward the caput until adequate sperm quality is obtained. In the extreme case in which multiple consecutive specimens contain suboptimal sperm, the tunica of the epididymis may be reflected off the testis itself to expose the efferent ducts to collect additional samples (12), or a TESE can be performed.
The technique of actual specimen collection is variable, and none of these techniques have been evaluated in a head-to-head prospective manner. Some microsurgeons use a pulled glass micropipette to micropuncture an epididymal tubule and aspirate the fluid directly. Another technique involves puncturing the tubule and allowing the epididymal fluid to pool. Hematocrit pipettes (dependent on capillary action) are then used to collect the pools of epididymal fluid. If hematocrit pipettes are not available, a 1 mL syringe containing sperm buffer attached to a 24-gauge angiocatheter may also be used instead. Again, bloody areas should and can be avoided. One of the main advantages of MESA is the ability to get clean, blood-free samples with high sperm concentration. Although samples collected generally range from 10-20 microliters, the total numbers of sperm harvested range from 15-99 million (10,11). MESA does require the use of general anesthesia or at least regional anesthesia with IV sedation as well as a trained microsurgeon.
Nonobstructive azoospermia
Before the advent of IVF-ICSI, men with non-obstructive azoospermia only had the options of using donor sperm or adoption, with no feasible route to biological paternity. However, the advent of ICSI allowed the use of exceedingly low numbers of testicular sperm to allow biological paternity for up to 15% of infertile men (5). With the discovery that the testis can have a heterogeneous pattern of sperm production, it became possible to find and remove small pockets of sperm producing testicular tissue for use with assisted reproduction and to spare the remaining testicular tissue. Methods currently employed for sperm retrieval in this setting include TFNA, TESE, and microdissection testicular sperm extraction (mTESE). With the introduction of mTESE, optical magnification has allowed selective seminiferous tubule removal resulting in higher sperm retrieval rates with less testicular tissue removal (9.4 vs. 720 mg) when compared to conventional or multi-biopsy TESE (13).
Fine needle aspiration
TFNA is the same procedure as performed for obstructive azoospermia (see earlier in review). TFNA in this setting may be performed after a biopsy for sperm retrieval or as a method of “mapping” the areas of spermatogenesis in the testis prior to sperm retrieval (14). The effectiveness of TFNA to extract spermatozoa in patients with nonobstructive azoospermia, however, has been shown in multiple controlled series to be less than that of open testicular biopsies (15). Hence, we do not recommend TFNA for use as a primary or solitary technique of retrieval.
Testicular sperm extraction (TESE)
Conventional TESE involves the removal of testicular tissue and can be done with or without optical magnification. Either a single site or multiple sites can be sampled and the number of samples (and volume of tissue) removed is highly variable among reproductive urologists. Certainly, conventional TESE is a blind technique in terms of choosing a site for sperm extraction, though attempts have been done to try and localize areas of spermatogenesis prior to TESE (16-18). Multiple-site, multiple-sample TESE may result in the removal of a large testicular volume with uncertain sperm retrieval. Another underlying and considerable shortcoming of this approach is the risk of interrupting testicular blood supply. The subtunical vessels are distributed over the testis surface before penetrating into testicular parenchyma and it is difficult to avoid these vessels without an operating microscope. Given the risk of bleeding, contamination of samples with blood, and the larger amount of tissue removed, our preference is ideally to proceed with a route that provides a higher chance of sperm retrieval with the fewest number of procedures.
Microdissection testicular sperm extraction (mTESE)
The risk of testicular injury in conjunction with low spermatozoa collection led to the development of the mTESE (13). It involves the use of an operating microscope to help identify seminiferous tubules that are more likely to harbor spermatogenesis. The testis with larger volume or more advanced spermatogenic pattern seen on biopsy (if prior biopsy was performed) is usually initially chosen. Using magnification, the subtunical and intra-testicular vessels can be visualized and preserved. A wide incision is made into the tunica albuginea in an avascular region, and the testicular parenchyma is exposed during this initial wide exposure. The surgeon then proceeds to microsurgically develop dissection lanes along testicular lobules to separate and directly examine each seminiferous tubule for likelihood of sperm production (Figure 1). The underlying principle is that those tubules that are more likely to harbor spermatogenesis are filled with germ cells and are more likely to be larger in diameter and opaque in color. Those tubules that are sclerotic or Sertoli-cell only will have a smaller diameter and be more attenuated on visual examination. Only those tubules more likely to harbor sperm production are removed using microsurgical technique and evaluated intra-operatively by an embryologist. Only when adequate yields of sperm are found is the microdissection completed and the testis closed.

Studies have shown mTESE allows for greater chance of retrieving sperm, higher sperm yields, and lower removal of testicular tissue compared to conventional TESE (13,19,20). Fewer acute and chronic changes to the testis have been seen by ultrasound and hormonal evaluation after mTESE when compared to conventional multi-biopsy TESE (21). But even with the mTESE, the surgeon should always be aware that a higher number of biopsies are counterbalanced by the increased risk of damaging testicular vasculature.
A number of areas in mTESE merit further discussion and special considerations, and are as follows.
Tissue processing
Once testicular tissue samples are obtained by mTESE, they are dispersed in 300-500 microliters of sperm transport media. Sterile scissors are used to mince tubules to achieve mechanical disruption. Further dispersal is performed by passing the suspension of testicular tissue through a 24-G angiocatheter to further disperse the tubules, which results in higher sperm yield (22). Even if sperm are not initially seen in the operating room, tissue digestion and extensive tissue search may yield sperm in 7% of cases in the largest series of mTESE cases reported (23).
Role of testicular biopsy
Given that diagnostic testicular biopsy result does not preclude sperm retrieval nor ensure it, in our practice, a diagnostic testicular biopsy is not required prior to attempts at sperm retrieval. Even with Sertoli cell-only pattern on histology, the chance of sperm retrieval is still approximately 25-40% (24-27). If that number is not low enough for the couple to preclude proceeding with IVF, then we believe that diagnostic biopsy is unnecessary and only inserts another procedure that may have potential for morbidity.
Predictors of sperm retrieval in mTESE
Clearly, one of the biggest gaps in our knowledge of non-obstructive azoospermia is finding predictors of spermatogenesis that can be used to guide patients regarding the decision to proceed with sperm retrieval. The ideal test would be non-invasive, easy to perform, be able to accurately predict and/or preclude sperm retrieval, be cost-effective, and be widely available. While the perfect test does not yet exist, there have been multiple attempts at correlating a number of tests with sperm retrieval rates.
For mTESE, the most advanced stage seen on biopsy (not the predominant one) as well as history of previous successful TESE, are currently the only known predictors of successful sperm retrieval (25,27-30). On the other hand, the etiology of nonobstructive azoospermia, testicular volume, serum FSH levels, operative length, body mass index, baseline testosterone level, and response to medical therapy for hypogonadism thus far have shown little to no impact on the chance of sperm retrieval (24,28,31-35). In fact, attempts at creation of multi-variable models have also only had modest success in predicting sperm retrieval outcomes (36). Therefore, likely only new technologies [including advanced cellular imaging (18), gene expression patterns in testicular biopsies (37), and other novel biomarkers of spermatogenesis] may enable us to better predict those who will benefit from sperm retrieval.
Conclusions
Advances in assisted reproductive technology and specifically IVF-ICSI have revolutionized our ability to offer biological paternity to men with azoospermia. While microsurgical reproductive tract reconstruction was once the only treatment option for these men, modern sperm retrieval techniques have allowed for the ability to retrieve sperm for assisted reproduction with minimal morbidity and maximal sperm yield. The procedure of choice depends on the etiology of the azoospermia, but in both obstructive and non-obstructive azoospermia, microsurgical techniques offer tremendous advantages and should be the technique of choice when available. While currently few clinical predictors can predict the chance of finding sperm in non-obstructive azoospermia, we await advances in technology that will allow us to more accurately predict who will benefit from surgical sperm retrieval in non-obstructive azoospermia.
Acknowledgements
We would like to thank Vanessa Dudley for her assistance with the artwork used in this article.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gunnell DJ, Ewings P. Infertility prevalence, needs assessment and purchasing. J Public Health Med 1994;16:29-35. [PubMed]
- Philippov OS, Radionchenko AA, Bolotova VP, et al. Estimation of the prevalence and causes of infertility in western Siberia. Bull World Health Organ 1998;76:183-7. [PubMed]
- Thonneau P, Marchand S, Tallec A, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod 1991;6:811-6. [PubMed]
- Willott GM. Frequency of azoospermia. Forensic Sci Int 1982;20:9-10. [PubMed]
- Jarow JP, Espeland MA, Lipshultz LI. Evaluation of the azoospermic patient. J Urol 1989;142:62-5. [PubMed]
- Mooney JK Jr, Horan AH, Lattimer JK. Motility of spermatozoa in the human epididymis. J Urol 1972;108:443-5. [PubMed]
- Shufaro Y, Prus D, Laufer N, et al. Impact of repeated testicular fine needle aspirations (TEFNA) and testicular sperm extraction (TESE) on the microscopic morphology of the testis: an animal model. Hum Reprod 2002;17:1795-9. [PubMed]
- Yafi FA, Zini A. Percutaneous epididymal sperm aspiration for men with obstructive azoospermia: predictors of successful sperm retrieval. Urology 2013;82:341-4. [PubMed]
- Pasqualotto FF, Rossi-Ferragut LM, Rocha CC, et al. The efficacy of repeat percutaneous epididymal sperm aspiration procedures. J Urol 2003;169:1779-81. [PubMed]
- Sheynkin YR, Ye Z, Menendez S, et al. Controlled comparison of percutaneous and microsurgical sperm retrieval in men with obstructive azoospermia. Hum Reprod 1998;13:3086-9. [PubMed]
- Janzen N, Goldstein M, Schlegel PN, et al. Use of electively cryopreserved microsurgically aspirated epididymal sperm with IVF and intracytoplasmic sperm injection for obstructive azoospermia. Fertil Steril 2000;74:696-701. [PubMed]
- Zenke U, Jalalian L, Shen S, et al. The difficult MESA: findings from tubuli recti sperm aspiration. J Assist Reprod Genet 2004;21:31-5. [PubMed]
- Schlegel PN. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod 1999;14:131-5. [PubMed]
- Turek PJ, Cha I, Ljung BM. Systematic fine-needle aspiration of the testis: correlation to biopsy and results of organ “mapping” for mature sperm in azoospermic men. Urology 1997;49:743-8. [PubMed]
- Friedler S, Raziel A, Strassburger D, et al. Testicular sperm retrieval by percutaneous fine needle sperm aspiration compared with testicular sperm extraction by open biopsy in men with non-obstructive azoospermia. Hum Reprod 1997;12:1488-93. [PubMed]
- Turek PJ, Givens CR, Schriock ED, et al. Testis sperm extraction and intracytoplasmic sperm injection guided by prior fine-needle aspiration mapping in patients with nonobstructive azoospermia. Fertil Steril 1999;71:552-7. [PubMed]
- Tunç L, Alkibay T, Küpeli B, et al. Power Doppler ultrasound mapping in nonobstructive azoospermic patients prior to testicular sperm extraction. Arch Androl 2005;51:277-83. [PubMed]
- Ramasamy R, Sterling J, Fisher ES, et al. Identification of spermatogenesis with multiphoton microscopy: an evaluation in a rodent model. J Urol 2011;186:2487-92. [PubMed]
- Amer M, Ateyah A, Hany R, et al. Prospective comparative study between microsurgical and conventional testicular sperm extraction in non-obstructive azoospermia: follow-up by serial ultrasound examinations. Hum Reprod 2000;15:653-6. [PubMed]
- Tsujimura A, Matsumiya K, Miyagawa Y, et al. Conventional multiple or microdissection testicular sperm extraction: a comparative study. Hum Reprod 2002;17:2924-9. [PubMed]
- Ramasamy R, Yagan N, Schlegel PN. Structural and functional changes to the testis after conventional versus microdissection testicular sperm extraction. Urology 2005;65:1190-4. [PubMed]
- Ostad M, Liotta D, Ye Z, et al. Testicular sperm extraction for nonobstructive azoospermia: results of a multibiopsy approach with optimized tissue dispersion. Urology 1998;52:692-6. [PubMed]
- Ramasamy R, Reifsnyder JE, Bryson C, et al. Role of tissue digestion and extensive sperm search after microdissection testicular sperm extraction. Fertil Steril 2011;96:299-302. [PubMed]
- Ramasamy R, Schlegel PN. Microdissection testicular sperm extraction: effect of prior biopsy on success of sperm retrieval. J Urol 2007;177:1447-9. [PubMed]
- Abdel Raheem A, Garaffa G, Rushwan N, et al. Testicular histopathology as a predictor of a positive sperm retrieval in men with non-obstructive azoospermia. BJU Int 2013;111:492-9. [PubMed]
- Okada H, Dobashi M, Yamazaki T, et al. Conventional versus microdissection testicular sperm extraction for nonobstructive azoospermia. J Urol 2002;168:1063-7. [PubMed]
- Haimov-Kochman R, Lossos F, Nefesh I, et al. The value of repeat testicular sperm retrieval in azoospermic men. Fertil Steril 2009;91:1401-3. [PubMed]
- Su LM, Palermo GD, Goldstein M, et al. Testicular sperm extraction with intracytoplasmic sperm injection for nonobstructive azoospermia: testicular histology can predict success of sperm retrieval. J Urol 1999;161:112-6. [PubMed]
- Ramasamy R, Ricci JA, Leung RA, et al. Successful repeat microdissection testicular sperm extraction in men with nonobstructive azoospermia. J Urol 2011;185:1027-31. [PubMed]
- Seo JT, Ko WJ. Predictive factors of successful testicular sperm recovery in non-obstructive azoospermia patients. Int J Androl 2001;24:306-10. [PubMed]
- Ramasamy R, Lin K, Gosden LV, et al. High serum FSH levels in men with nonobstructive azoospermia does not affect success of microdissection testicular sperm extraction. Fertil Steril 2009;92:590-3. [PubMed]
- Ramasamy R, Fisher ES, Ricci JA, et al. Duration of microdissection testicular sperm extraction procedures: relationship to sperm retrieval success. J Urol 2011;185:1394-7. [PubMed]
- Reifsnyder JE, Ramasamy R, Husseini J, et al. Role of optimizing testosterone before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J Urol 2012;188:532-6. [PubMed]
- Bryson CF, Ramasamy R, Sheehan M, et al. Severe testicular atrophy does not affect the success of microdissection testicular sperm extraction. J Urol 2014;191:175-8. [PubMed]
- Ramasamy R, Bryson C, Reifsnyder JE, et al. Overweight men with nonobstructive azoospermia have worse pregnancy outcomes after microdissection testicular sperm extraction. Fertil Steril 2013;99:372-6. [PubMed]
- Ramasamy R, Reifsnyder JE, Husseini J, et al. Localization of sperm during microdissection testicular sperm extraction in men with nonobstructive azoospermia. J Urol 2013;189:643-6. [PubMed]
- Ando M, Yamaguchi K, Chiba K, et al. Expression of VASA mRNA in testis as a significant predictor of sperm recovery by microdissection testicular sperm extraction in patient with nonobstructive azoospermia. J Androl 2012;33:711-6. [PubMed]


