Acupuncture assisted local anesthesia for penile surgeries
IntroductionOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
Over the last few decades, several types of regional nerve blockade had been developed for penile surgeries with the patients under local anesthesia (1-5) rather than the well-established general or spinal anesthesia which could not prevent patients from complications on cardiac and central nerve system. Among varied penile surgeries penile implantation may be the most challenging one, either an inconvenient and unpleasant pudendal nerve block, or an adjuvant intravenous injection of sedatives, had been unavoidable (6-12). We will like to overview an innovative combination of acupuncture and several specific topical nerve blocks for varied penile surgeries including the penile implantation on ambulatory basis. This had unexceptionally been sustainable thus far. In method I there are the bilateral proximal dorsal nerve block (13,14), and peripenile infiltration; Whereas in method II specifically adding up with penile crural block (15), cavernous nerve blockade and topical injection of the medial low abdomen for penile implant. We found that these local anesthetic techniques can offer an optimal and viable option.
Acupuncture applicationOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
Since July 1998, acupuncture was routinely used as an adjuvant to local anesthesia, which is beneficial in particularly if the patient became tense during diagnostic work up such as pharmaco-cavernosography, ultrasonography, or experienced discomfort during preoperative preparation. The acupoints of Hegu (LI4), Shou San Li (LI10), Quchi (LI11), and either Waiguan (TE5) or Neiguan (PC6) (Figure 1) were routinely used. The Hegu point is located between the first and second metacarpal bones, at the highest point of prominence when the thumb and the index finger are adducted. The Quchi point is found at the lateral end of the transverse cubital crease, with the elbow flexed at a right angle. The Shou San Li point is positioned three finger’s breadths caudally to the Quchi acupoint. The Waiguan point is positioned two finger’s breadths proximal to the middle point of the volar transverse carpal crease, between the flexor carpi radialis muscle and palmaris longus tendon, with the forearm prone, while the acupoint of Neiguan is projected dorsally.

The innervations of the human penis (16-18)Other Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
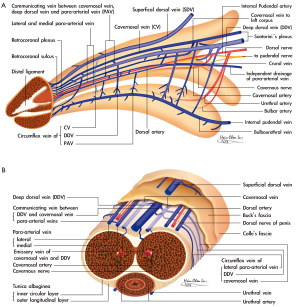
The knowledge of penile anatomy and innervations is pre-requisite for managing those techniques (Figure 2). The human penis is a unique structure composed of multiple fascial layers which surround the three cylinders of erectile sinusoids, the most ideal milieu to apply Pascal’s law in the human body. Thus, it consists of the glans penis, the corpus spongiosum (CS) with the bulb of the urethra, the paired corpora cavernosa (CC) and the bulbospongiosus, as well as the ischiocavernosus muscles. It is the most sensitized organ in the human body owing to its dense nervous distribution. A full review of the nervous pathway and neurophysiology of the human penis is not necessary for the purpose of this article. However, one must always keep in mind the relationship between the cavernous nerve and pudendal nerve along with the penile vascular system to the bony and fibromuscular structures of the penis, in order for the surgeon to be able to reproduce these nervous blockades. At the level of penile hilum where the distal third urethral bulb is met, and the penile crura are formed, the fibers of cavernous nerve are located at around the medial third of each CC. Some of these cavernous fibers enter the CC and CS laterally, abutting with the cavernous and urethral arteries. The remaining fibers travel distally with the dorsal nerve and enter the CC as well as the CS in various sites to innervate the mid and distal penile shaft. Meanwhile, the paired pudendal nerves, with somatomotor as well as somatosensory components, are located one-finger-breadth cranio-posterioly and are regarded as the starting point of the proximal dorsal nerve. The somatic sensory nerves originate at the receptors in the penile skin and glans penis. Subsequently, signals carrying sensory information of pain and temperature ascend via the spinothalamic tract; while vibratory stimuli are carried in the dorsal column; and touch and pressure sensations are transmitted via both pathways to the thalamus. All the transmitting signals of the motor nerve are sent from lateral to medial tracts, and vice versa for the sensory component. Therefore, a lateral blockade of certain nerve always can result an anesthetic effect to its medial innervating proper. It is a rule that the anatomical arrangement of the deep dorsal vein, dorsal artery and dorsal nerve is arrayed from the medial side. Although a thorough understanding of the penile neuroanatomy is indispensable for a well done penile implantation, the recognition of the fibro-muscular skeleton of the human penis is also a prerequisite and clinically meaningful, since through recognition the bony or fibro-muscular landmarks helps to precisely localize any specific nerve.
The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)Other Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
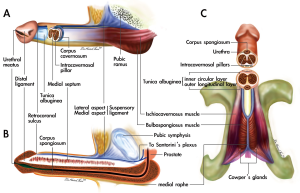
The traditional anatomical description of human penis has been well established. However, it may not be detailed enough to deliver a precise fibrous landmark which is essential for adequate nerve blockade during outpatient penile surgeries. Recent studies have reported more knowledge about the penile tunical anatomy, which will benefit the surgeon in recognizing the detailed fibrous landmarks within the penis. This includes the tunica albuginea (19), the exact position and relationship between the skeletal muscle and smooth muscles (20), the upper border as well as the lower margin of the symphysis pubis and the ischial tuberosity. The tunica albuginea is consistently described as a single layer with uniform thickness and strength circumferentially. Recent studies, however, support a revised model of the tunica albuginea of the CC as a bi-layered structure with a 360° complete inner circular layer and a 300° incomplete outer longitudinal coat. Furthermore its thickness as well as strength can vary much depending of its specific position. The outer longitudinal layer is absent between the 5 and 7 o’clock positions, where two triangular ligamentous structures form. These structures, termed the ventral thickening (VT), are a continuation of the anterior fibers of the left and right bulbospongiosus muscles, respectively. A weak border is positioned ventrally between two VTs where the CS and CC lean each other, and a hazardous prosthesis extrusion might be implicated from this region (21). On the dorsal aspect, between the 1 and 11 o’clock positions, is the region called the dorsal thickening, a radiating aspect of the bilateral ischiocavernosus muscles. It is then converged distally and arranged centrally to form a distal ligament (DL) which is located immediately above the 12 o’clock position of the navicular fossa of the distal urethra and acts as a trunk of the glans penis. Without this strong ligament, the glans would be too weak to bear the buckling pressure generated during coitus. A surgeon should be able to feel five pre-requisite fibrous or bony landmarks of the penis prior to surgery. First of all, the distal tip of the distal ligament can be clearly perceived if one puts the finger palm of one’s index finger, for example, over the glanular tip. Secondly, the borders of the CS formed by bilateral VTs can be felt when one put her/his finger palm over the penoscrotal junction of patient. This is more easily palpable if the patient is asked to make an anal constriction. Thirdly, one is able to tell whether the patient’s penile hilum is fibrotic or not by feeling that the underlying suspensory ligament is free of resistance when one uses a gentle pushing force along the pubic angle or from the lateral aspect when the penile shaft is pulled away from the body axis. When the hilum is less fibrotic, it is easier to introduce the injection needle, thus allowing for more precise proximal dorsal nerve block. In the fourth place, one has to be sure of the exact discrimination between the border of the upper border as well as the lower margin of the symphysis pubis. And last of all, the ability to palpate the ischial tuberosity.
Proximal dorsal nerve block and peripenile infiltration (Figure 4)Other Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
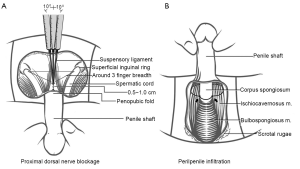
For making proximal dorsal nerve block (Figure 4A), a 23-gauge, 1.25' (3.18-cm) disposable needle connected to a 10-mL syringe, was used to inject the local anesthetic of a 0.8% lidocaine solution prepared in an aseptic bowl prefilled with 1.0 mL of a 1:200,000 epinephrine solution. With the bevel parallel to the longitudinal body axis, the needle is introduced in-between the suspensory ligaments along the pubic angle while the penile shaft is pulled a little caudally away from the body axis by the surgeon’s left hand. Then the injection is made in three directions in order to cover the proximal dorsal nerves bilaterally. An aspiration of the syringe is made before any attempt of injection in order to avoid inadvertent entry into the vessels. Under a finger guide, the needle is withdrawn back just sufficiently to free it from being entrapped in the penile hilum. The needle is then shifted laterally and advanced to the lateral margin of penile crus; then an injection is slowly delivered while the needle is withdrawn until the subcutaneous space is encountered. The needle is advanced caudally and further infiltration is made till the median raphe after ensuring no inadvertent entry into a vessel. This step results in negligible pain of the needle puncture for peripenile infiltration. The contralateral side is anesthetized in a similar fashion. For performing peripenile infiltration (Figure 4B), two underlying rigid borders are felt by palpation while pushing downward from the penoscrotal junction. A right-handed surgeon requires the patient’s glans penis to be held upward by an assistants’ left hand with the palm of the index finger and thumb pinch the 3 and 9 o’clock positions respectively at the retrocoronal sulcus. Then a precise puncture is made at the intersection of the medial raphe and the penoscrotal junction. Subsequently, a meticulous injection of the VT is made bilaterally from its medial margin. The peripenile infiltration is performed in a semi-circumferential manner unilaterally, and then the infiltration of the contralateral side is made in a similar fashion to complete the circle in the ventral aspect. Thus, topical infiltration to the junction between the CS and the CC is mandatory in order to avoid an incomplete block of the sensitive CS. Care should be taken not to puncture the paper-thin tunica albuginea of the CS. A gauge compression of the bleeding point for several minutes is sufficient to stop the bleeders if the spongiosa body is incidentally entered. The scrotal infiltration may be extended caudally if a water reservoir is intended to implant in the scrotal pouch. Finger guided manipulation is very helpful in the entire procedure.
Penile crural and cavernous nerve block (Figure 5)Other Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
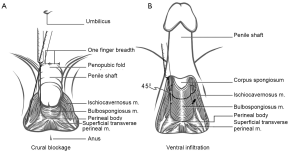
For doing penile crural block (Figure 5A), the penile shaft is put in a pendulous position while the patient is in a comfortable supine position. A 23G ×1.5' (3.81-cm)-long disposable needle is punctured into the skin at the intersection of the penopubic fold, one finger-breadth laterally. Under finger guidance, the needle is pushed downward vertically along the pubic angle until the medial third penile crus is targeted. It is then withdrawn a little upward before the local anesthetic solution is delivered in case of inadvertent puncture into the corpus. A bloody aspiration denotes that the CC is entered. An experienced hand can feel whether an inadvertent puncture through the tunica has been made since the tunica can act as a barrier in providing an intermediate resistance. An injection of 2 to 3 mL solution is sufficient to block the neurofibers of the cavernous nerve. Under finger guidance, the needle is withdrawn sufficiently to free it from being entrapped in the penile hilum. The needle is then advanced to the lateral margin down to the ischial tuberosity. A slow and even delivery of the local anesthetic solution is made while the needle is withdrawn superficially until the subcutaneous space is met. In order to fulfill a cavernous nerve blockage (Figure 5B), a 23-gauge, 1.5-cm disposable needle is recommended for this purpose. The penile shaft is stretched upward while the penoscrotal junction is identified. The needle is targeted at a 45° angle oblique to the coronal plane at the junction of the CS and the penile crus. It is advanced to about 2 cm in order to block the cavernous nerve. Thus there are two opportunities to perform the cavernous nerve blockade, dorsally and ventrally. An additional topical anesthetic injection is required if implantation of a three-piece prosthesis is performed.
Clinical applicationOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
From July 1998 to July 2013, total of 1,481 males had undergone this anesthesia on an ambulatory basis without exception thus far. In order to provide a comprehensive overlook Table 1 summaries the demography of 1,481 males. Overall no patient cannot abide the outpatient rule. In method I there were 1,353 men in whom 993 men of penile venous stripping surgeries, 336 cases of penile corporoplasty, 8 males of urethroplasty, 7 patients of vaso-vasostomy, 6 men of penile arterial reconstruction and 3 males of penectomy. In method II there were 125 cases of penile implant with varied models but type of three pieces. This included 48 AMS 600, 13 AMS 650, 6 Ambicor, 2 Dynaflex, 15 Duraphase, 33 Acuform, and 8 Spectra. A further topical injection of the medial low abdominal region made it possible for implanting a three-piece model of AMS 700 CX in 3 males.
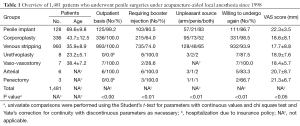
Full table
There were rare to encounter either early significant complications or late complication but one diabetic man who experienced a prosthesis extrusion resulting from 48 hours sitting for playing Mahjong. Two patients were complicated by postoperative self-limited infection which was not associated with local anesthesia. There was no statistical difference in scoring using a visual analog scale (VAS) among patients who underwent different models of prosthesis implantation, except for those who received the AMS 700 CX, in which a higher VAS score was characteristic.
DiscussionOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
Acupuncture analgesia was reported to involve endogenous opioid peptide via somatosympathetic reflex (22-26). Subsequently it has boomed up a lot of interesting studies (27-31). It seems meaningful to enhance those specific nerve blocks in penile surgeries in our long time clinical practice of acupuncture which is not difficult to handle (32,33). Similarly reproducibility of these nerve blocks is not challenging if one adopts the advanced penile anatomy although a learning curve of these techniques exists of course, and requires practice. A thorough recognition and understanding of the bony as well as fibromuscular landmarks of the penis is indispensable to the achievement of adequate anesthetic effect of local penile anesthesia. The surface markings of the pelvic region and the inguinal region have been previously described in anatomical texts, which were exclusively derived from human cadavers. In the surgeon’s clinical practice, however, an attempt to directly apply that anatomical knowledge may not be practical until a proper recognition of these markings is given. Furthermore, finger-guided manipulation by the assistant’s index finger is helpful for confirming the exact position of the injection throughout the anesthetic procedure. This can be done because the tissue is palpable due to the paucity of adipose tissue, the layered nature of the tissue, and the tuck tunica albuginea that provides a bony-like barrier which can be palpated. Particularly during the crural block, the exact location can be definitely confirmed if the ischiocavernosus muscle is contracted. Precise puncture and injection of the local anesthesia not only minimizes the pain, but also saves the consumption of the local anesthetic agent.
Local anesthesia by pudendal nerve block has been advocated in previous studies (6). In our clinical experience, however, pudendal nerve block has not been very effective and may have the following disadvantages. They include the long time of manipulation needed for anesthesia, the difficulty to completely disinfect the perineum region, the requirement for patient’s position change if a booster injection is needed, the susceptibility to puncture of a vessel, and possible postoperatively perineal pain. Similarly, a local anesthetic was proposed to be retained in the distal CC which was bandaged by a rubber at the penile base (9); however we caution against this kind of application since puncture through the tunica can be extraordinarily hazardous if an implant is in situ, and a booster injection would be necessary when the patient registers pain intraoperatively. Meanwhile, particularly in a geriatric impotent male patient, excessive venous drainage of the sinusoidal blood with local anesthetic may result in harmful insult to patients. The feasibility of a crural block is a frequently encountered concern in obese patients, in whom the injection needle might not be sufficiently long enough. We have also observed that the elasticity of the penopubic skin and its underlying tissue can readily compromise the thickness of the entire tissue layer. Initially we use a 23G ×3.5' (8.89-cm)-long disposable needle and found that it was, by no means, easy to be handled because a longer needle is likely to be feebler and, in turn, not be able to sufficiently sustain against buckling force; furthermore, difficulty to localize an already tortured needle sometimes occur. In most patients, an injection needle of 1.25' (3.18-cm) is sufficiently long for this purpose, if the skin is properly anesthetized. Moreover, during injection at the junction between the CS and CC, it is advisable for the needle to be targeted at a 45-degree angle oblique to the coronal plane, and be injected deeper in order to block the cavernous nerve. There is, therefore, one more opportunity for the cavernous nerve blockade with this manipulation. The pain evoked by the dilatation of the CC can thus be avoided.
Still patients should be counseled that a somewhat painful injection of the local anesthetic agent should be expected. In reality, however, a quick puncture through the skin accompanied by slow injection of the anesthetic is usually acceptable (34). Local anesthesia for penile implant of a one-piece or two-piece device has been recommended and well accepted as an option for anesthesia. However, pure local anesthesia for a three-piece device requires more precise placement of the local anesthesia. It is too early to draw any conclusions about 3-piece implants, since we have only performed three cases of this prosthesis implant under local anesthesia. Regardless of the type of implantation used, the penile micro-architecture must be well understood in order for the surgeon to master the injection technique, otherwise arbitrary application of the local anesthetic agent not only wastes the drug but can also result in ineffective anesthesia. Effective local anesthesia of the penis appears to result in lesser complications in our experience. The local anesthetic techniques of crural block, cavernous nerve block, and proximal dorsal nerve block, although challenging, have proven to be reproducible in our experience. We expect these techniques to have great potential, because of the convenience and advantages for the patients.
Acupuncture assisted Local anesthesia on an outpatient basis for penile surgeries appears to be highly promising. The local anesthetic methods of proximal dorsal nerve block, peripenile infiltration, penile crural block, cavernous nerve blockage, and a topical injection on an as needed basis have been proven to be reliable, simple, and safe with fewer complications in our study. Local anesthesia offers the advantages of less anesthetic adverse effects, less morbidity, more protection of patient’s privacy, and a more-rapid return to daily activity with minimal complications (35).
AcknowledgementsOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
We would like to thank Benedict S. A. Murrell for his English editing, along with Ms Hsiu-Chen Lu, Nicola Chen their preparations of illustration and photos for this manuscript.
FootnoteOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
Conflicts of Interest: The authors have no conflicts of interest to declare.
ReferencesOther Section
- Introduction
- Acupuncture application
- The innervations of the human penis (16-18)
- The fibro-muscular and 3-Dimensional anatomy of the human penis (Figure 3)
- Proximal dorsal nerve block and peripenile infiltration (Figure 4)
- Penile crural and cavernous nerve block (Figure 5)
- Clinical application
- Discussion
- Acknowledgements
- Footnote
- References
- Kirya C, Werthmann MW Jr. Neonatal circumcision and penile dorsal nerve block--a painless procedure. J Pediatr 1978;92:998-1000. [PubMed]
- Brown TC, Weidner NJ, Bouwmeester J. Dorsal nerve of penis block--anatomical and radiological studies. Anaesth Intensive Care 1989;17:34-8. [PubMed]
- Dunn RL, Harris DL. Technique for continuous dorsal penile nerve anaesthesia following penile surgery. Br J Surg 1997;84:220-1. [PubMed]
- Ghanem H, Fouad G. Penile prosthesis surgery under local penile block anaesthesia via the infrapubic space. Int J Androl 2000;23:357-9. [PubMed]
- Das A, Soroush M, Maurer P, et al. Multicomponent penile prosthesis implantation under regional anesthesia. Tech Urol 1999;5:92-4. [PubMed]
- Dos Reis JM, Glina S, Da Silva MF, et al. Penile prosthesis surgery with the patient under local regional anesthesia. J Urol 1993;150:1179-81. [PubMed]
- Kaufman JJ. Penile prosthetic surgery under local anesthesia. J Urol 1982;128:1190-1. [PubMed]
- Benson RC Jr, Barrett DM, Patterson DE. The Jonas prosthesis--technical considerations and results. J Urol 1983;130:920-2. [PubMed]
- Light JK, Scott FB. Implantation of the inflatable penile prosthesis using local anesthesia. In: Kaye KW. eds. Outpatient Urologic Surgery. Philadelphia: Lea & Febiger, 1985:261-8.
- Scott FB. Outpatient implantation of penile prostheses under local anesthesia. Urol Clin North Am 1987;14:177-85. [PubMed]
- Leach GE. Local anesthesia for urologic procedures. Urology 1996;48:284-8. [PubMed]
- Stav A, Gur L, Gorelik U, et al. Modification of the penile block. World J Urol 1995;13:251-3. [PubMed]
- Hsu GL, Chen SH, Weng SS. Out-patient surgery for the correction of penile curvature. Br J Urol 1997;79:36-9. [PubMed]
- Hsu GL, Hsieh CH, Wen HS, et al. Outpatient surgery for penile venous patch with the patient under local anesthesia. J Androl 2003;24:35-9. [PubMed]
- Hsu GL, Hsieh CH, Wen HS, et al. Outpatient penile implantation with the patient under a novel method of crural block. Int J Androl 2004;27:147-51. [PubMed]
- Breza J, Aboseif SR, Orvis BR, et al. Detailed anatomy of penile neurovascular structures: surgical significance. J Urol 1989;141:437-43. [PubMed]
- Salmons S. Muscle: muscles and fasciae of the trunk. In: Bannister LH, Berry MM, Collins P, et al. eds. 38th ed. Gray’s Anatomy. London: Churchill Livingstone, 1995;809-34.
- Lue TF. Male sexual dysfuction. In: Tanagho EA, McA ninch JW. eds. Smith’s General Urology. McGraw-Hill, 2000:788-9.
- Hsu GL, Brock G, Martinez-pinerio L, et al. The three-dimensional structure of the human tunica albuginea: anatomical and ultrastructural level. Int J Impot Res 1992;4:117-29.
- Hsu GL, Hsieh CH, Wen HS, et al. Anatomy of the human penis: the relationship of the architecture between skeletal and smooth muscles. J Androl 2004;25:426-31. [PubMed]
- Hsu GL, Brock G, Martínez-Piñeiro L, et al. Anatomy and strength of the tunica albuginea: its relevance to penile prosthesis extrusion. J Urol 1994;151:1205-8. [PubMed]
- He LF. Involvement of endogenous opioid peptides in acupuncture analgesia. Pain 1987;31:99-121. [PubMed]
- Huang CS, Tsai YF. Somatosympathetic reflex and acupuncture-related analgesia. Chin J Physiol 2009;52:345-57. [PubMed]
- Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol 2008;85:355-75. [PubMed]
- Wang SM, Kain ZN, White P. Acupuncture analgesia: I. The scientific basis. Anesth Analg 2008;106:602-10. [PubMed]
- Wang SM, Kain ZN, White PF. Acupuncture analgesia: II. Clinical considerations. Anesth Analg 2008;106:611-21. table of contents. [PubMed]
- Zheng Z, Feng SJ. Acupuncture analgesia for temporal summation of experimental pain: a randomised controlled study. Eur J Pain 2010;14:725-31. [PubMed]
- Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain 2011;152:755-64. [PubMed]
- Nir RR, Granovsky Y, Yarnitsky D, et al. A psychophysical study of endogenous analgesia: the role of the conditioning pain in the induction and magnitude of conditioned pain modulation. Eur J Pain 2011;15:491-7. [PubMed]
- Moont R, Pud D, Sprecher E, et al. ‘Pain inhibits pain’ mechanisms: Is pain modulation simply due to distraction? Pain 2010;150:113-20. [PubMed]
- Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol 2010;23:611-5. [PubMed]
- Hsu GL. Peyronie’s disease. In: Kim YC, Tan HM. eds. APSIR BOOK on Erectile Dysfunction, 1st. ed. Malaysia: Pacific Cosmos Sdn Bhd., 1999:200-12.
- Hsu GL, Hsieh CH, Chen HS, et al. The advancement of pure local anesthesia for penile surgeries: can an outpatient basis be sustainable? J Androl 2007;28:200-5. [PubMed]
- Serour F, Mandelberg A, Mori J. Slow injection of local anaesthetic will decrease pain during dorsal penile nerve block. Acta Anaesthesiol Scand 1998;42:926-8. [PubMed]
- Hsu GL, Molodysky E, Liu SP, et al. A combination of penile venous stripping, tunical surgery and varicocelectomy for patients with erectile dysfunction, penile dysmorphology and varicocele under acupuncture-aided local anesthesia on ambulatory basis. Surgery 2013;S12:008.


