
High grade renal trauma management: a survey of practice patterns and the perceived need for a prospective management trial
Introduction
The kidney is the most commonly injured genitourinary organ in trauma (1). Conservative management of renal trauma, including angioembolization is now widely accepted and has an overall success of 80–90% (2,3); however, data from the National Trauma Databank (NTDB) suggests that as high as 1/3 of high grade renal trauma patients are managed with nephrectomy (4). There is a low level of evidence underlying renal trauma management guidelines and management remains variable and controversial, especially in high grade renal injury (5-10). While some argue it is necessary to perform nephrectomy for management of severe renal injury, others believe that conservative management with angioembolization can be successful even for unstable patients (2,11). Our recent multi-institutional study supported by American Association for the Surgery of Trauma (AAST) demonstrated that nephrectomy remains the most common renal trauma bleeding intervention at 13% while angioembolization was only used in 6% of cases (12).
Prior studies have sought to understand variation in trauma management practice patterns (13,14). Nearly a decade ago, Yeung et al. (15) surveyed both trauma surgeons from the AAST and urologists managing renal trauma and found significant variation in the workup and management of renal trauma. More specifically, for bleeding control they found differences in the use of imaging characteristics such as vascular contrast extravasation triggering angioembolization. In addition renal trauma management and outcomes have been demonstrated to vary by trauma level designation, with level 1 trauma centers more likely to perform conservative management, including angioembolization (5,16). These studies highlight a need for more standardized, evidence based renal trauma management guidelines.
To date, there have been no cohort prospective trials performed to inform renal trauma management. Imperative to prospective research development is an understanding of the practice patterns, as well as the needs and interest of key ‘stakeholders’. The purpose of this study was to evaluate the current practice patterns of clinicians managing high grade renal trauma, their access to interventional radiology (IR), and to assess stakeholder interest in a prospective multi-institutional trial utilizing a protocol designed to minimize nephrectomy.
Methods
Institutional Review Board approval was granted from the University of Utah (IRB_00036782). An electronic survey was developed in Research Electronic Data Capture program (REDCap) aimed to assess multiple factors surrounding the management of renal trauma. Prior to survey dissemination a panel of expert trauma surgeons and urologists involved in renal trauma management reviewed and provided a critique of the survey. Their feedback was then used to modify the questions in order to improve question clarity, focus, and to eliminate redundancy.
The final survey was comprised of 29 questions including yes/no, multiple choice, and fill in the blank questions. Three categories were included in the survey: (I) demographics: including age, location of practice, years in practice, physician type, fellowship training, trauma center designation of primary practice, location of practice, and society membership [AAST or Society of Genitourinary Reconstructive Surgeons (GURS)]; (II) IR access and utilization; and (III) renal trauma management for high grade renal injuries. High grade renal injuries were defined as AAST grades III–V as utilized in numerous prior studies due to increased risk of clinically significant hemorrhage as compared to grades I–II (7,12,17-19).
IR access was assessed by asking whether there was a readily available practitioner, such as a radiologist, vascular surgeon, or trauma surgeon, to perform angiography and angioembolization. IR access was also assessed by classifying the location of services as: in the operating suite or in a separate area, and whether practitioners have difficulty arranging IR procedures. Further, participants were asked if IR was ever used for renal trauma and how often in the prior 12 months.
Renal trauma management was assessed in several ways. Participants were asked about how they had managed renal trauma cases in the last 12 months and the number of injuries that had managed. If they had performed nephrectomy they were asked about the circumstances that led to the nephrectomy. Participants were also asked about their comfort with renal repair, such as renorrhaphy or partial nephrectomy. Attitudes about renal preservation were also assessed by asking for reasons patients would or would not benefit, in the short and long-term, from renal preservation.
Management was also evaluated with three clinical scenarios designed to identify surgeon practice patterns for high grade renal injury (Figure 1). Clinical scenario 1 assesses the surgeon’s willingness to use a damage control and packing strategy with further imaging versus immediate exploration in a patient with suspected renal injury discovered during laparotomy. In clinical scenario 2, the surgeon’s feelings about employing angioembolization rather than retroperitoneal exploration is assessed with a patient who has been explored and had initial imaging suggesting vascular contrast extravasation from the kidney. Finally, clinical scenario 3 assesses the preferred management (operative, observation, or angioembolization) of a patient with otherwise non-operative blunt injuries who has a high-grade renal injury with signs of the potential for needing interventions for bleeding from the kidney. These 3 clinical scenarios were intended to overall judge the willingness of trauma surgeons to utilize conservative non-operative management of renal injury with different situations that mimic real life trauma scenarios.
In addition to these three categories of questions, participants were asked about thresholds for bleeding interventions. Finally, participants were asked about perceived value in a prospective trial designed to evaluate a protocol that would decrease nephrectomy after renal trauma. Participants were also asked if they would participate in such a theoretical trial.
The survey was distributed by the AAST and GURS via email distribution to members of the societies between April and May, 2018. As an incentive to participate, an Apple iPad was provided to a randomly selected participant after closure of the survey in July, 2018. Descriptive statistics were utilized to analyze frequencies of different participant responses. Chi square was used to compare different characteristics between level one trauma centers and other trauma designations using SPSS 21©.
Results
Demographics
A total of 253 practitioners responded with an average age of 48.4±10.4 years. The majority trauma/acute care surgeons (TS/ACS) 63.2%, followed by urologists, 34.4%, and 2.4% “other” practitioners (including non-operative critical care practitioners). Most practiced at level 1 trauma centers 80.6% in 39 US states and 28 non-US countries (Table 1). The states with the highest number of participants included Texas (8.7%), California (7.5%), and Florida (5.1%). The overall response rates were 11.1% (150/1,353) for AAST and 28.9% (87/301) for GURS members. Sixty-two percent of responders were in practice >10 years. The majority of respondents completed a fellowship: 63.7% ACS/TS and 25.7% a GURS fellowship.
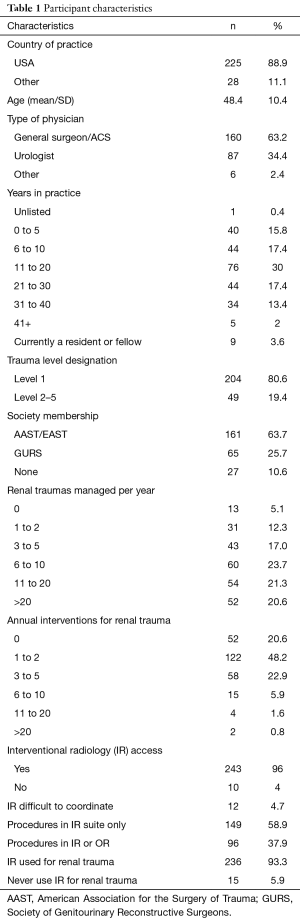
Full table
Renal trauma management
Sixty-five percent of respondents had managed greater than 5 renal traumas in the previous 12 months. Ninety-five percent found value in renal preservation in acute and long-term recovery despite having renal damage. Most respondents reported utilizing IR (73.9%) and having comfort in performing either simple (41.5%) or complex (45.1%) renorrhaphy/partial nephrectomy. Renal packing (20.6%) and renorrhaphy/partial nephrectomy (24.1%) were reported less commonly.
Practitioners who reported being comfortable with renal repair were more likely to have done so in the acute setting (27.3% of those comfortable vs. 2.9% of those not comfortable, P=0.001). Approximately half the respondents (50.6%) reported needing to perform a nephrectomy for renal injury management in the last year. The most common reasons to perform nephrectomy were “patient exsanguinating within 4 hours of arrival” (31.6%), and “patient with other injuries requiring operative intervention, and the kidney bleeding as well” (31.2%) (Table 2).

Full table
IR
A total of 96.1% had access to IR. Of those with IR access, most IR procedures were performed in the IR suite (61.3%). Overall, few reported difficulties obtaining IR services. In fact, most participants (73.9%) had used angioembolization as a management strategy in the last year (Table 3).
Full table
The three clinical scenarios (Figure 1) revealed that most participants favored non-operative management or angioembolization when feasible rather than retroperitoneal exploration. Seventy percent of respondents, in scenario 1, favored packing the abdomen and obtaining imaging when there was a suspected renal injury rather than retroperitoneal exploration when patients were otherwise stable in the OR after immediate exploration. In clinical scenario 2, the majority of surgeons (83%) favored angiographic management of a high-grade renal injury with evidence of vascular contrast extravasation on imaging or observation rather than attempt at renal repair during a laparotomy for other injuries. Similarly, in clinical scenario 3, 75% of respondents favored non-operative management of a renal injury even with a large hematoma, deep lacerations, and some segmental infarction, in a patient that did not otherwise require laparotomy.
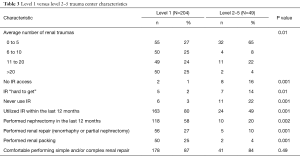
When comparing trauma center designation, level 1 versus other levels, we found a higher volume of renal traumas and significantly greater access to and utilization of IR in level 1 centers (Table 2). Further, renal repair was more likely to be performed at level one center. There was no significant difference in comfort level with simple or complex renal repairs between the different trauma center designations.
There was a wide range in the threshold that surgeons felt were appropriate for bleeding risk and interventions to prevent bleeding (Figure 2). Most commonly participants would wait until clinical bleeding was evident (32%). Most respondents believed there was some (42.3%, 107/253) or a lot (40.3%, 102/253) of value in a prospective trial to develop an acute renal trauma management protocol and would be interested in participating, 78.3% (198/253) (Figure 2).

Discussion
Our findings demonstrate that clinicians managing renal trauma value renal preservation, report high IR access and utilization rates, and have confidence in their ability to perform renal repair. However, the survey results also show that nephrectomy is still performed routinely, and in only 32% of patients due to exsanguination, demonstrating that there may be patients where nephrectomy could be avoided. The responses to common clinical scenarios showed that surgeons favored non-operative managements of renal trauma, often utilizing further imaging or angioembolization rather than renal exploration. Finally, respondents felt there would be value in a multi-institutional prospective study evaluating a renal trauma management protocol.
Non-operative management, including angioembolization, is now the accepted approach for the majority of patients presenting with high grade renal trauma (2,3,7,20-22). The shift to conservative management of renal trauma is reflected in our survey results in which 95% of respondents reported value in renal preservation in the acute trauma setting and many favored non-operative management of renal injuries, even if already performing an exploratory laparotomy for other injuries (Figure 1). This rate of reported conservative management was in keeping with the overall high IR access rate. More than 90% of respondents had access to IR, and greater than 70% reported utilization of this intervention in the last year for renal bleeding management. These rates are similar to a recent survey study by Glass et al. (23) which found a in a cohort of 413 urologists and interventional radiologists, all practitioners responding from level 1 and 2 trauma centers had access to IR and 60% reported utilizing angioembolization in the preceding year.
Despite the survey results showing that respondents valued renal preservation, had IR access, and felt competent to perform renal repair, half the respondents reported the need to perform a nephrectomy in the preceding 12 months. This is in keeping with our recent multi-institutional AAST study which revealed nephrectomy was the most common bleeding intervention for high grade trauma at 13% while angioembolization was performed in only 6% (12). The reason for this discrepancy may be ‘recall bias’ in the survey responses, resulting in discrepancy between a practitioner’s perceptions of management and actual practice. The most common reasons for nephrectomy was “exsanguination within the first 4 hours of arrival” (31.6%) and for “exploratory laparotomy for other injuries with concurrent renal bleeding” (31.2%). In many cases, nephrectomy may be life-saving. However, in other cases, such as those with non-renal injuries and concurrent renal bleeding, there may be opportunities for conservative management. Conservative management could consist of angioembolization, damage control packing, and delayed renal repair after resuscitation.
Although overall IR access was excellent, it was not generally available in the respondents’ OR (Table 1). Prior studies have demonstrated successful management of renal injury with angioembolization in both stable and unstable patients (2,11), further, most patients with high grade renal injury undergoing exploratory laparotomy undergo nephrectomy (4,12). It is therefore possible that initially unstable patients taken to the OR emergently may be better served by damage control maneuvers, such as packing the retroperitoneum and angioembolization; this is a strategy that might avoid retroperitoneal exploration and nephrectomy. Besides the use of angioembolization, renal repair could also prevent nephrectomy. Interestingly, despite most respondents (87%) reporting comfort with simple or complex renal repair, only 24% performed renal repair, in the prior 12 months. This may be due to a lack of clinical scenarios that would warrant repair, or perhaps indicate that renal repair is not something practitioners feel comfortable with in acute renal trauma management. This overall data reflects a need for education on opportunities to increase angiographic intervention and renal repair thereby decreasing nephrectomy when possible.
Prior studies have demonstrated differences in renal trauma outcomes and IR access and utilization between level 1 trauma centers versus other trauma center designations (5,24). This was echoed in the present study as we found level 1 trauma centers demonstrated higher rates of reported IR access and utilization, and increased numbers of renal sparing surgical interventions, including renorrhaphy, and partial nephrectomy. Using the NTDB, Hotaling et al. revealed higher rates of angiographic procedures and improved renal trauma outcomes for patients undergoing observation, minimally invasive, or open renal surgery at level 1 trauma centers compared to lower level centers (5). These discrepancies in renal trauma management and outcomes by center designation reflect a need for increased education, protocol development/dissemination, and early transfer to level 1 trauma centers.
Most respondents reported they thought there would be value in a prospective trial designed to evaluate a protocol designed to reduce nephrectomy rates (Figure 2). Further, almost 80% of the cohort reported an interest in participating in a prospective renal trauma management trial. Further, the need for a prospective trial is demonstrated by the variation in reported threshold for bleeding intervention based on a proposed nomogram (Figure 2). The highest response rate (32%), indicated that interventions should be not be done unless continued bleeding or hemodynamic instability occurred; however, there was a wide variation in responses for a threshold for intervention for predicted renal bleeding. Similar studies have revealed variation in triggers of angioembolization. Yeung et al. found trauma surgeons were more likely to use hematoma location and vascular contrast extravasation as a trigger for selective angioembolization than urologists (98% vs. 52%, P<0.0001) (15). Glass et al. similarly showed differences in angioembolization use with urologists more likely to utilize for grade V renal injuries (81% vs. 56%, P=0.03), and interventional radiologists more likely to utilize for low grade injuries (33% vs. 3%, P=0.002) and penetrating injuries (83% vs. 58%, P=0.02). The findings of this and similar studies further confirm the need for a multi-institutional prospective trial to evaluate thresholds for intervention for renal hemorrhage and generally renal trauma management.
As with any survey data, there were limitations to this study. Despite offering incentives, the response rate was only 11% for AAST and 30% for GURS members. Although this is a comparable response rate for similar studies (14,15), low response rates inherently introduce selection/response bias into findings. Further, we mostly evaluated members of two, well-established trauma societies, practitioners who are theoretically best informed on the most current trauma management protocols. Therefore, we likely missed respondents that would potentially benefit most from a prospective trial, such as those covering trauma patients at lower level trauma centers. While we attempted to design an easy to interpret survey with the assistance of field experts, it is not possible to list every potential management choice. Despite these limitations, most respondents were experienced trauma surgeons practicing at mostly level 1 trauma centers. This suggests that our survey data is an accurate reflection of key stakeholder attitudes towards renal trauma management and interest in a prospective study.
Conclusions
We found the majority of practitioners managing high grade renal trauma value renal preservation, have access to IR, and are comfortable with renorrhaphy. However, there was variability in reported thresholds for performing angioembolization, low renal repair rates, and half of respondents reported a need to perform a nephrectomy for acute renal trauma management within the last year, only 30% due to exsanguination. There is great interest and need for a prospective trial to standardize care and promote renal sparing acute trauma management. Efforts should be directed towards trial development.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval was granted from the University of Utah (IRB_00036782). The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Terrier JE, Paparel P, Gadegbeku B, et al. Genitourinary injuries after traffic accidents: Analysis of a registry of 162,690 victims. J Trauma Acute Care Surg 2017;82:1087-93. [Crossref] [PubMed]
- van der Wilden GM, Velmahos GC, Joseph DK, et al. Successful nonoperative management of the most severe blunt renal injuries: a multicenter study of the research consortium of New England Centers for Trauma. JAMA Surg 2013;148:924-31. [Crossref] [PubMed]
- Santucci RA, Fisher MB. The literature increasingly supports expectant (conservative) management of renal trauma--a systematic review. J Trauma 2005;59:493-503. [Crossref] [PubMed]
- Wessells H, Suh D, Porter JR, et al. Renal injury and operative management in the United States: results of a population-based study. J Trauma 2003;54:423-30. [Crossref] [PubMed]
- Hotaling JM, Wang J, Sorensen MD, et al. A national study of trauma level designation and renal trauma outcomes. J Urol 2012;187:536-41. [Crossref] [PubMed]
- McClung CD, Hotaling JM, Wang J, et al. Contemporary trends in the immediate surgical management of renal trauma using a national database. J Trauma Acute Care Surg 2013;75:602-6. [Crossref] [PubMed]
- McCombie SP, Thyer I, Corcoran NM, et al. The conservative management of renal trauma: a literature review and practical clinical guideline from Australia and New Zealand. BJU Int 2014;114 Suppl 1:13-21. [Crossref] [PubMed]
- Bryk DJ, Zhao LC. Guideline of guidelines: a review of urological trauma guidelines. BJU Int 2016;117:226-34. [Crossref] [PubMed]
- Groen J, Pannek J, Castro Diaz D, et al. Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur Urol 2016;69:324-33. [Crossref] [PubMed]
- Morey AF, Brandes S, Dugi DD 3rd, et al. Urotrauma: AUA guideline. J Urol 2014;192:327-35. [Crossref] [PubMed]
- Lanchon C, Fiard G, Arnoux V, et al. High Grade Blunt Renal Trauma: Predictors of Surgery and Long-Term Outcomes of Conservative Management. A Prospective Single Center Study. J Urol 2016;195:106-11. [Crossref] [PubMed]
- Keihani S, Xu Y, Presson AP, et al. Contemporary management of high-grade renal trauma: Results from the American Association for the Surgery of Trauma Genitourinary Trauma study. J Trauma Acute Care Surg 2018;84:418-25. [Crossref] [PubMed]
- Dennis BM, Medvecz AJ, Gunter OL, et al. Survey of trauma surgeon practice of emergency department thoracotomy. Am J Surg 2016;212:440-5. [Crossref] [PubMed]
- Zarzaur BL, Kozar RA, Fabian TC, et al. A survey of American Association for the Surgery of Trauma member practices in the management of blunt splenic injury. J Trauma 2011;70:1026-31. [Crossref] [PubMed]
- Yeung LL, Brandes SB. Contemporary management of renal trauma: differences between urologists and trauma surgeons. J Trauma Acute Care Surg 2012;72:68-75; discussion 77. [Crossref] [PubMed]
- Cudnik MT, Newgard CD, Sayre MR, et al. Level I versus Level II trauma centers: an outcomes-based assessment. J Trauma 2009;66:1321-6. [Crossref] [PubMed]
- Keihani S, Rogers DM, Putbrese BE, et al. A nomogram predicting the need for bleeding interventions after high-grade renal trauma: Results from the American Association for the Surgery of Trauma Multi-institutional Genito-Urinary Trauma Study (MiGUTS). J Trauma Acute Care Surg 2019;86:774-82. [Crossref] [PubMed]
- McGuire J, Bultitude MF, Davis P, et al. Predictors of outcome for blunt high grade renal injury treated with conservative intent. J Urol 2011;185:187-91. [Crossref] [PubMed]
- Myers JB, Brant WO, Broghammer JA. High-grade renal injuries: radiographic findings correlated with intervention for renal hemorrhage. Urol Clin North Am 2013;40:335-41. [Crossref] [PubMed]
- Robert M, Drianno N, Muir G, et al. Management of major blunt renal lacerations: surgical or nonoperative approach? Eur Urol 1996;30:335-9. [Crossref] [PubMed]
- Moudouni SM, Patard JJ, Manunta A, et al. A conservative approach to major blunt renal lacerations with urinary extravasation and devitalized renal segments. BJU Int 2001;87:290-4. [Crossref] [PubMed]
- Chow SJ, Thompson KJ, Hartman JF, et al. A 10-year review of blunt renal artery injuries at an urban level I trauma centre. Injury 2009;40:844-50. [Crossref] [PubMed]
- Glass AS, Appa AA, Kenfield SA, et al. Selective angioembolization for traumatic renal injuries: a survey on clinician practice. World J Urol 2014;32:821-7. [Crossref] [PubMed]
- Gor RA, Styskel BA, Li T, et al. Unexpected High Rates of Angiography and Angioembolization for Isolated Low-grade Renal Trauma: Results From a Large, Statewide, Trauma Database. Urology 2016;97:92-7. [Crossref] [PubMed]



