Testosterone replacement therapy and the heart: friend, foe or bystander?
Introduction
The relationship between the use of testosterone therapy (TTh) and increased risk of cardiovascular disease (CVD) outcomes is still controversial (1,2). Little is known about whether or not this controversy will soon be clarified (3,4). The main reason is that in the last decade the use TTh has had an unprecedented growth (4). Multiple causes have been suggested to be responsible for this increase (2,4). For instance, the prevalence of testosterone deficiency and hypogonadism (testosterone deficiency plus symptoms) among American men is 24% and 5.6%, respectively (5-7). It is estimated that there are approximately 2.4 million men in the U.S. aged 40 to 69 years with testosterone deficiency (8,9). In addition, a greater concern is that by 2025 approximately 6.5 million American men aged 30 to 80 years will suffer from testosterone deficiency (3). Further, testosterone deficiency is frequently accompanied by a number of symptoms including sexual dysfunction, fatigue, mood disturbance, decline in bone mineral density, and changes in body composition, with increased adipose tissue and decreased muscle mass (3,7,10).
The epidemic of obesity has also played an important role in the increased use of TTh (11). Most epidemiological studies have shown that weight gain (measured by body mass index, waist circumference and percent body fat) reduces the levels of testosterone. Therefore, it is suggested that obesity has the potential to increase the use of TTh through the reduction of testosterone levels (10,12). The concern regarding the interplay between obesity, testosterone deficiency, and TTh is that the rates of obesity are expected to continue increasing (13).
Another significant contributor of the high prevalence of testosterone deficiency and increased use of TTh is the aging of the American male population (14). Testosterone peaks during the teenage years, but starts decreasing among men in their late 30’s (8,15). These factors combine with their sequelae have become a significant public health concern.
Therefore, capitalizing on the increasing prevalence of testosterone deficiency, hypogonadism, the obesity epidemic, and the aging of the American male population, pharmaceutical companies have aggressively strategized direct-to-consumer marketing (3,4,14). Similarly, the establishments of clinics specializing in treating testosterone deficiency have increased by promoting that men who use TTh will become more energetic, alert, mentally sharp, and sexually functional. In fact, “many men have obtained prescriptions not as a medical therapy for male hypogonadism, but as a way to combat fatigue, low sex drive, and weight gain with the goal to regaining the vitality of their youth” (3,4,16). Although it would be expected that the significant increased use of TTh to treat testosterone deficiency would be considered a logical remedy, this treatment has generated one of the most well-known controversies due to a suggested increase risk of CVD among users.
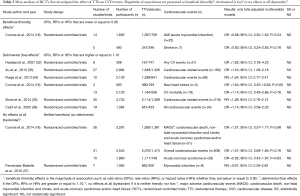
Criteria to define “beneficial (friendly use)”, “detrimental (foe)” and “no effects at all (bystander)” groups
In this review, we critically discuss the previous and emerging literature on the association between TTh and CVD’s from original research studies and meta-analyses of observational studies and of randomized-placebo controlled trials. We separated the body of literature into three groups: “beneficial (friendly use),” “detrimental (foe),” and “no effects at all (bystander)” based on their magnitude of association (overall for the meta-analyses). For instance, studies with “beneficial (friendly use)” effect had a magnitude of association, such as odd ratios (OR’s), rate ratios or relative risk (RR’s), or hazard ratios (HR’s), that is below or equal to 0.90; studies with “detrimental (foe)” effects had OR’s, RR’s or HR’s that are higher or equal to 1.10; or “no effects at all (bystander)” if it is neither “friendly” nor “foe”. These cutoff points were chosen arbitrarily, but magnitudes of association with values that are <90.0 or <1.10 have a very small effect that is difficult to interpret; they are closer to the null and very likely due to chance. In addition, we considered whether these magnitude of associations reached statistically significance (SS) or not (NS). For consistency, we only presented the magnitude of the association of CVD (fatal and nonfatal) events comparing higher to lower levels of testosterone (continuous increment of testosterone or categorical by comparing high to low groups). For those studies that presented their analyses by comparing low to high categorical groups of testosterone, we took the reciprocal of the magnitude of the association to present the comparison of high to low categorical groups. It is possible that one single study can be presented more than once in the tables because they reported several independent analyses using total-, free- and bioavailable-testosterone with different CVD events (i.e., myocardial infarction, stroke, etc.). Furthermore, we only reported those studies that were fully-adjusted in the multivariable modeling. Studies that investigated the interplay between levels of testosterone or use of TTh with all-cause mortality were not included in this review, as most of these studies do not take into account competing risks in their analyses, so the possibility of confounded association increases.
High serum total-, free- and bioavailable-testosterone and CVD events in epidemiologic studies (Table 1)

Full table
To understand the controversy of the interplay between use of TTh on CVD events, it is important to first present the current literature on the role of endogenous testosterone in the development of CVD events in population-based studies (Table 1) (17-27). Naturally, testosterone levels among men peaks during the teenage years and decreases in the late 30’s (8,15). Interestingly, the risk of CVDs increases with age. Therefore, epidemiological studies have investigated the relationship between levels of testosterone and etiology of CVD outcomes very closely. We primarily focused on presenting the association of high levels of serum total-, free- and bioavailable testosterone with CVD events (fatal and nonfatal) in prospective cohort studies. We identified 12 prospective studies that used different CVD outcomes (fatal and nonfatal) and different exposures of testosterone, such as total-, free- and bioavailable-testosterone (17-27). These forms of testosterone measurements were reported as continuous increment (low to high) or categorical (highest vs lowest percentile). In terms of validity of the study design, randomized controlled trials (RCT’s) have the highest validity, followed by prospective studies. However, most randomized trials of TTh are not powered to investigate their effect on CVD outcomes (28).
Beneficial (friendly) effect
In the “beneficial (friendly)” effects group, we identified six prospective studies that conducted analyses of high levels of total-, free- and bioavailable-testosterone with different CVD events. For instance, Yeap et al. 2009 (17) reported independent associations of high levels of total- and free-testosterone with the same CVD outcome [incident stroke or transient ischemic attack (TIA)]. With the exception of one study [Hak et al. 2002 (21), n=504], most of these prospective studies included a study population of more than 1,000 participants. Yeap et al. 2014 (20) was the research study with the largest number of number of men included, 3,690. Several studies included in their analyses more than 300 CVD events. For instance, Ohlsson et al. (18) investigated a total of 485 CVD events and Yeap et al. 2009 (17) study was the one with the smallest number of CVD events (n=119). The longest follow-up years was conducted in Shores et al. 2014 that included a median of 9 years (19).
In general, the majority of the multivariable analyses in these studies showed that high levels of total-, free-, or bioavailable-testosterone reduced the risk CVD events. The majority of the magnitude of associations were below 0.71, and lowest one was 0.20 (21). Most of these associations were statistically significant. The only three analyses that did not reach statistical significance had a magnitudes of association of 0.84 (18), 0.90 (19), and 0.85 (20). Although several analyses were conducted with total-, free- and bioavailable-testosterone with different CVD events, we did not find a specific pattern whether one of the forms of testosterone has a greater effect with one of the CVD events.
Detrimental (foe) effects
In the “detrimental (foe)” effects group, we only found four studies (19,23-25). Also, these studies conducted several analyses using high levels of total-, free- and bioavailable-testosterone with different CVD events. The study with the largest number of participants included 1,568 men (23) and the one with the smallest number of participants included 495 (24). Reasonable number of CVD events were included in these studies as well, the study with the highest number of CVD events included 436 (19) and the one with the smallest number 80 (23). The follow-up time for study participant was similar to the one from “beneficial (friend)” effects group with 10 years of follow-up (25). The magnitude associations varied widely in this group. One of the studies reported a 3.61-fold increased risk of ischemic arterial disease (IAD) (24) and the one with lowest magnitude of association reached a value of 1.14 for first ever MI (23). Interestingly, of all the analyses conduced in this group, only one reached statistical significant (24). This is study reported a 3.61-fold increased risk for IAD among men with high levels (Q5 ≥6.85) of total testosterone compared to second quartile (Q2 3.94–4.88), however, this study has one of the smallest number of CVD events included in the analysis (n=146).
No effects at all (bystander)
In this group, we only identified four prospective studies (20,23,26,27). However, several independent analyses were conducted. The sample size in the study with the largest number of participants included 3,620 (20). It is important to note that although several analyses were conducted in these studies most of them included very small numbers of CVD such as <100 (Vikan et al. 2009, n=80; and Haring et al. 2013, n=56 and n=92). The number of follow-up of years is very similar to the other studies in Table 1. Yet, none of these studies included in this group reached statistical significance. Conducting different analyses using total-, free-, or bioavailable did not make a different in the values of the magnitude of associations. It is possible that the lack of statistical significance can be driven by the small numbers of CVD events, but also most of the values for the magnitude of associations are small and close to the null. Because there are other well-established risk factors for CVD events (e.g., smoking, diabetes, hypertension, diet, etc.), it is very unlikely that TTh plays a role in the development of those CVD outcomes. Therefore, in this body of literature TTh may be a bystander.
Meta-analyses of observational studies investigating the association between serum total-, free- and bioavailable-testosterone and CVD events in epidemiological studies (Table 2)

Full table
We conducted similar review of the literature with the meta-analyses of epidemiological studies, and we separated this literature three groups of “beneficial (friendly use)”, “detrimental (foe)” and “no effects at all (bystander)” groups using the overall value of magnitude of association. Three meta-analyses of epidemiological studies were found (29-31). However, the inclusion of different study designs was included. For instance, Corona et al. 2011 included only cross-sectional studies (n=54 studies), while Araujo et al. 2011 included a combination of both prospective and cross-sectional (n=7 studies). The third meta-analyses study only included prospective studies (n=18 studies). It is important note that the overall magnitude of associations of the total-, free-, and bioavailable-testosterone with different CVD events in the three meta-analyses were all “beneficial (friendly) effects”. These meta-analyses either included a large number of participants or large number of CVD events. The largest meta-analyses of epidemiological studies conducted as of to date is from Corona et al. 2011 that reported a statistical significant inverse association between total testosterone and CVD events (HR =0.53; 95% CI, 0.44–0.60) in 54 studies. Similarly, Ruige et al., 2011 reported a reduced risk of CVD events among men with higher levels of total testosterone (HR =0.89; 95% CI, 0.83–0.96), while no significant association were reported in Araujo et al. meta-analyses. Although cross-sectional studies do not have the same validity compared to prospective studies and randomized trials they are hypothesis driven and in the findings reported by Corona et al. in the 54 studies were similar in magnitude and direction compared to the 18 prospective used in Ruige et al. 2011.
Meta-analyses of randomized placebo-controlled trials investigating the effect of TTh on CVD events (Table 3)
Full table
In Table 3, only meta-analyses of randomized placebo-controlled trials were presented (16,32-37). Again, the overall value of magnitude of association was used to divide the three groups of “beneficial (friendly)”, “detrimental (foe)” and “not effects all (bystander)”. We identified a total of seven meta-analyses of RCT’s. The largest meta-analyses, Borst et al. 2014, included a total of 35 RCT’s followed by Corona et al. 2014 that included 31 trials. As previously mentioned, RCT’s have the highest validity compared to prospective studies; however, they are not powered with number of CVD events. For instance, in the two largest meta-analyses of randomized placebo controlled trials, the number of CVD events were 218 in Borst et al. 2014, and 209 in Corona et al. 2014. In the prospective studies shown in Table 1, the study with the largest number of CVD events included 485 (18). However, the difference in number of CVD events included meta-analyses of epidemiological studies compared to meta-analyses of RCT’s is much wider. The meta-analyses of only prospective studies included a total of 4,598 CVD events compared to the largest meta-analyses of RCT’s that included only 218 CVD events. On the other hand, the number of men taking TTh and included in the placebo group is robust. The two largest meta-analyses of RCT’s included more than 2,000 who used TTh and more than 1,400 men in the placebo controlled groups. It is noteworthy to mention that among all meta-analyses of RCT’s presented in Table 3, only one reported statistical significance in the effect of TTh on CVD events (33).
Beneficial (friendly) effect
In this group, only one meta-analyses reported beneficial effects (Corona et al. 2014) (16). This meta-analyses conducted two independent analyses looking at the effect of TTh on CVD outcomes, acute myocardial infarction (n=22) in 14 randomized trials and stroke (n=7) in five randomized trials. However, none of the protective effects reached a statistical significance, [OR =0.68; 95% CI, 0.30–1.52 (P=0.34)] and [OR =0.82; 95% CI, 0.24–2.83 (P=0.76)].
Detrimental (foe) effects
We identified six meta-analyses in this group (16,32-36). In fact, this is where we found most of the independent analyses conducted between TTh and CVD events. In addition, the only significant inverse association between TTh and CVD events was observed under this group; there was a statistically significant 54% increased risk of cardiovascular related events after comparing use of TTh with placebo (OR =1.54; 95%CI, 1.09–2.18). Again, although the magnitude of association of 1.54 is high and statistically significant, one must be cautious with the interpretation of this finding due to the small number of CVD events (n=180).
No effect at all (bystander)
Two meta-analyses were identified in this group (16,37). Corona et al. 2014 included 26 trials, whereas Fernández-Balsells et al. analyzed seven trials. In Corona et al. 2014 meta-analyses more in-depth analyses were conducted by using different CVD outcomes, but not one of them reached statistical significance. Since the effects of these analyses are small and so close to the null, they may be due to chance. Two of the CVD outcomes analyses in Corona et al. included 51 (major cardiovascular events) and 29 (acute coronary syndrome) events. As previously discussed, the magnitudes of these effects are so small and close to the null that may be due to due to chance. In addition, many other well-established factors related to CVD events that were not taken into account in these meta-analyses (e.g., diet) may be playing a significant role. Therefore, any interpretation derived from this body of literature should be made with caution.
Meta-analyses of retrospective cohort studies investigating the association between use of TTh and CDV events (Table 4)

Full table
After reviewing the body of literature using meta-analyses of prospective studies and RCT’s, we also found one meta-analyses of retrospective cohort studies (39). The importance to address this is meta-analysis of retrospective cohort studies is that two studies that received significant media attention by reporting an increased risk of CVD events among men who used TTh are considered retrospective cohort studies (40,41). Although the validity of retrospective studies is higher compared to that of other epidemiological studies such as cross-sectional studies, the RCT validity is not compared to the one of RCT’s and prospective studies. In general, retrospective studies were not designed to investigate the etiology of one specific outcome. Most of these studies capitalized from large databases that were not necessarily created with the intention to investigate the development of a specific outcome (e.g., cardiovascular or cancer) after following-up a group of people that were randomized into an intervention or control groups.
This meta-analyses of five retrospective studies reported a magnitude of association of OR =1.00, 95% CI, 0.79–1.25 (P=0.97). This value of magnitude of association falls within the group of “no effect at all (bystander)”. Thus, based from this body of literature of retrospective studies it is difficult to conclude that the use of TTh increased the risk of CVD events.
Conclusions
The body of literature that investigated the association of high levels of testosterone with CVD events in original prospective studies and meta-analyses of cross-sectional and prospective studies seems to be more consistent in demonstrating that higher levels of endogenous testosterone reduce the risk of CVD events. In addition, after we separated the body of literature into the three groups of “beneficial (friendly)”, “detrimental (foe)” and “no effects at all (bystander)” based on their magnitude of associations and statistical significance, a clearer picture emerged. We found more studies and analyses reporting a beneficial effect on reducing the risk of a CVD event than in the other two groups (foe or bystander). On the other hand, the body of literature using meta-analyses of RCT’s for the association between use of TTh and CVD events did not provide a clear picture after we divided it into the beneficial, detrimental or no effect all groups. Only one of meta-analyses of RCT’s found a statistical significant increased risk of CVD among men using TTh. However, due to the small number of CVD events included in the meta-analyses of RCT’s, the effect of TTh on CVD events remains inconclusive. In addition, it is even more difficult to derive a conclusion based on single retrospective studies or meta-analyses of retrospective cohort studies. The latter included five retrospective cohort studies and the overall magnitude of association was null.
In conclusion, after scrutinizing the literature that investigated the association of high levels of testosterone and use of TTh with CVD, we can confirm that we need a study or number of studies with adequate power and clinical and epidemiological data to provide a definitive conclusion on this controversy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kloner RA, Carson C 3rd, Dobs A, et al. Testosterone and Cardiovascular Disease. J Am Coll Cardiol 2016;67:545-57. [Crossref] [PubMed]
- Morgentaler A. Controversies and Advances With Testosterone Therapy: A 40-Year Perspective. Urology 2016;89:27-32. [Crossref] [PubMed]
- Malik RD, Lapin B, Wang CE, et al. Are we testing appropriately for low testosterone?: Characterization of tested men and compliance with current guidelines. J Sex Med 2015;12:66-75. [Crossref] [PubMed]
- Khera M. Controversies in testosterone supplementation therapy. Asian J Androl 2015;17:175-6. [Crossref] [PubMed]
- Baillargeon J, Urban RJ, Ottenbacher KJ, et al. Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Intern Med 2013;173:1465-6. [Crossref] [PubMed]
- Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2006;91:1995-2010. [Crossref] [PubMed]
- Araujo AB, Esche GR, Kupelian V, et al. Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab 2007;92:4241-7. [Crossref] [PubMed]
- Harman SM, Metter EJ, Tobin JD, et al. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab 2001;86:724-31. [Crossref] [PubMed]
- Bhattacharya RK, Khera M, Blick G, et al. Testosterone replacement therapy among elderly males: the Testim Registry in the US (TRiUS). Clin Interv Aging 2012;7:321-30. [Crossref] [PubMed]
- Rohrmann S, Shiels MS, Lopez DS, et al. Body fatness and sex steroid hormone concentrations in US men: results from NHANES III. Cancer Causes Control 2011;22:1141-51. [Crossref] [PubMed]
- Corona G, Giagulli VA, Maseroli E, et al. Testosterone supplementation and body composition: results from a meta-analysis of observational studies. J Endocrinol Invest 2016;39:967-81. [Crossref] [PubMed]
- Corona G, Giagulli VA, Maseroli E, et al. THERAPY OF ENDOCRINE DISEASE: Testosterone supplementation and body composition: results from a meta-analysis study. Eur J Endocrinol 2016;174:R99-116. [Crossref] [PubMed]
- Verma S, Hussain ME. Obesity and diabetes: An update. Diabetes Metab Syndr 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Snyder PJ, Bhasin S, Cunningham GR, et al. Effects of Testosterone Treatment in Older Men. N Engl J Med 2016;374:611-24. [Crossref] [PubMed]
- Khera M, Broderick GA, Carson CC 3rd, et al. Adult-Onset Hypogonadism. Mayo Clin Proc 2016;91:908-26. [Crossref] [PubMed]
- Corona G, Maseroli E, Rastrelli G, et al. Cardiovascular risk associated with testosterone-boosting medications: a systematic review and meta-analysis. Expert Opin Drug Saf 2014;13:1327-51. [Crossref] [PubMed]
- Yeap BB, Hyde Z, Almeida OP, et al. Lower testosterone levels predict incident stroke and transient ischemic attack in older men. J Clin Endocrinol Metab 2009;94:2353-9. [Crossref] [PubMed]
- Ohlsson C, Barrett-Connor E, Bhasin S, et al. High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. The MrOS (Osteoporotic Fractures in Men) study in Sweden. J Am Coll Cardiol 2011;58:1674-81. [Crossref] [PubMed]
- Shores MM, Biggs ML, Arnold AM, et al. Testosterone, dihydrotestosterone, and incident cardiovascular disease and mortality in the cardiovascular health study. J Clin Endocrinol Metab 2014;99:2061-8. [Crossref] [PubMed]
- Yeap BB, Alfonso H, Chubb SA, et al. In older men, higher plasma testosterone or dihydrotestosterone is an independent predictor for reduced incidence of stroke but not myocardial infarction. J Clin Endocrinol Metab 2014;99:4565-73. [Crossref] [PubMed]
- Hak AE, Witteman JC, de Jong FH, et al. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab 2002;87:3632-9. [Crossref] [PubMed]
- Khaw KT, Dowsett M, Folkerd E, et al. Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) Prospective Population Study. Circulation 2007;116:2694-701. [Crossref] [PubMed]
- Vikan T, Schirmer H, Njølstad I, et al. Endogenous sex hormones and the prospective association with cardiovascular disease and mortality in men: the Tromsø Study. Eur J Endocrinol 2009;161:435-42. [Crossref] [PubMed]
- Soisson V, Brailly-Tabard S, Helmer C, et al. A J-shaped association between plasma testosterone and risk of ischemic arterial event in elderly men: the French 3C cohort study. Maturitas 2013;75:282-8. [Crossref] [PubMed]
- Shores MM, Arnold AM, Biggs ML, et al. Testosterone and dihydrotestosterone and incident ischaemic stroke in men in the Cardiovascular Health Study. Clin Endocrinol (Oxf) 2014;81:746-53. [Crossref] [PubMed]
- Smith GD, Ben-Shlomo Y, Beswick A, et al. Cortisol, testosterone, and coronary heart disease: prospective evidence from the Caerphilly study. Circulation 2005;112:332-40. [Crossref] [PubMed]
- Haring R, Teng Z, Xanthakis V, et al. Association of sex steroids, gonadotrophins, and their trajectories with clinical cardiovascular disease and all-cause mortality in elderly men from the Framingham Heart Study. Clin Endocrinol (Oxf) 2013;78:629-34. [Crossref] [PubMed]
- Cunningham GR, Stephens-Shields AJ, Rosen RC, et al. Testosterone Treatment and Sexual Function in Older Men With Low Testosterone Levels. J Clin Endocrinol Metab 2016;101:3096-104. [Crossref] [PubMed]
- Corona G, Rastrelli G, Monami M, et al. Hypogonadism as a risk factor for cardiovascular mortality in men: a meta-analytic study. Eur J Endocrinol 2011;165:687-701. [Crossref] [PubMed]
- Araujo AB, Dixon JM, Suarez EA, et al. Clinical review: Endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab 2011;96:3007-19. [Crossref] [PubMed]
- Ruige JB, Mahmoud AM, De Bacquer D, et al. Endogenous testosterone and cardiovascular disease in healthy men: a meta-analysis. Heart 2011;97:870-5. [Crossref] [PubMed]
- Haddad RM, Kennedy CC, Caples SM, et al. Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc 2007;82:29-39. [Crossref] [PubMed]
- Xu L, Freeman G, Cowling BJ, et al. Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med 2013;11:108. [Crossref] [PubMed]
- Ruige JB, Ouwens DM, Kaufman JM. Beneficial and adverse effects of testosterone on the cardiovascular system in men. J Clin Endocrinol Metab 2013;98:4300-10. [Crossref] [PubMed]
- Borst SE, Shuster JJ, Zou B, et al. Cardiovascular risks and elevation of serum DHT vary by route of testosterone administration: a systematic review and meta-analysis. BMC Med 2014;12:211. [Crossref] [PubMed]
- Calof OM, Singh AB, Lee ML, et al. Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci 2005;60:1451-7. [Crossref] [PubMed]
- Fernández-Balsells MM, Murad MH, Lane M, et al. Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab 2010;95:2560-75. [Crossref] [PubMed]
- Corona G G, Rastrelli G, Maseroli E, et al. Testosterone Replacement Therapy and Cardiovascular Risk: A Review. World J Mens Health 2015;33:130-42. [Crossref] [PubMed]
- Corona G, Maggi M. Testosterone supplementation and cardiovascular risk. Trends Cardiovasc Med 2015;25:258-60. [Crossref] [PubMed]
- Finkle WD, Greenland S, Ridgeway GK, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One 2014;9:e85805. [Crossref] [PubMed]
- Vigen R, O'Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 2013;310:1829-36. [Crossref] [PubMed]


