Hypogonadism and testosterone replacement therapy in end-stage renal disease (ESRD) and transplant patients
Introduction
Low testosterone is a common finding in end-stage renal disease (ESRD) and renal transplant patients. Over half of male renal failure patients demonstrate low or low-normal levels of testosterone (1,2)—a much higher percentage than the 6–9% of men affected in the general population. The etiology is likely multifactorial and the term “uremic hypogonadism” has been coined to describe the hormonal state associated with kidney disease.
The clinical implications of low testosterone are varied and include associations with mood, anemia, muscle mass and strength, bone mass, and sexual function. Therapeutic options are controversial and include optimal management of kidney function, pharmacologic options, and testosterone replacement. The use of testosterone supplementation in particular has dramatically increased in the past few years. In the UK, the number of prescriptions for testosterone replacement increased nearly 90% from 2001–2010. Many of these prescriptions were for the newer, more costly, formulations resulting in a nearly 300-fold increase in healthcare costs (3).
Recently, testosterone replacement has been linked with increased cardiovascular risk—though this claim is controversial and has been disputed due to discrepancies in statistical analyses (4). Despite this widespread use of testosterone, data is lacking concerning the overall health risks, benefits, and effectiveness. The data on use of testosterone in ESRD patients is even more limited. Low testosterone levels have been correlated with higher all-cause and cardiovascular-related mortality in dialysis patients (5) and low levels at the time of transplantation are associated with patient and graft loss (6). There is a dearth of information on the effect of testosterone therapy in ESRD and transplant patients.
Etiology of hypogonadism in ESRD patients
Hypogonadism in ESRD patients is likely multifactorial. Many patients have comorbidities that can contribute to hypogonadism including diabetes, vascular disease, atherosclerosis, older age, and obesity. In addition to these pre-existing conditions, ESRD patients are in a chronically inflamed state; with documented elevated levels of inflammatory biomarkers (7). These factors are likely interrelated and ultimately culminate in changes to the hypothalamic-pituitary-gonadal axis. Though the process is complex and incompletely understood, there are several known disruptions including reduction of gonatotropin-releasing hormone (GNrH) and reduced amplitude of the resultant luteinizing hormone (LH) secretory burst (8). LH levels are elevated in chronic kidney disease (CKD) patients due to reduced testosterone feedback, and testicular failure contributes to reduced testosterone levels. Follicle-stimulating hormone (FSH) levels are also generally elevated. In addition, prolactin levels in CKD patients are elevated and resistant to suppression and can lead to suppression of the normal pulsatile release of GnRH (Table 1).
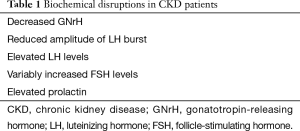
Full table
Clinical presentation of hypogonadism
Hypogonadism can affect multiple systems with sexual dysfunction perhaps being most obvious presentation and includes low libido, difficulties with orgasm, low overall sexual satisfaction, and erectile dysfunction (Table 2). The majority of men with ESRD report some form of sexual dysfunction with some studies reporting >80% of ESRD patients affected. Several studies have reported significantly lower quality of life scores on validated questionnaires (9,10) and have shown diminished quality of both physical and mental aspects of life.
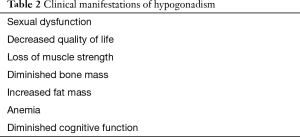
Full table
The association between testosterone deficiency and anemia in CKD patients has recently been studied and testosterone levels were found to be negatively associated with hemoglobin levels in uni- and multivariate models (11). CKD patients were 5 times more likely to be anemic if they had low testosterone levels. There was an inverse association between testosterone levels and erythropoiesis-stimulating agents (ESAs) as well, making testosterone a possible target for patients who are hyporesponsive to ESAs.
Many of these presentations however are nonspecific and can be found frequently in older patients with multiple comorbidities such as those on dialysis. It can be difficult to differentiate the etiology of these manifestations. Care should be taken to ensure adequate nutrition, physical activity, strength building, and correction of anemia in all patients prior to attributing clinical presentation to hypogonadism alone. Laboratory evaluation is critical to help discern the etiology.
Diagnosis
The diagnosis of hypogonadism is two-pronged and includes the laboratory detection of a low testosterone level and well as the corresponding signs and symptoms. It is important to be familiar with the laboratory assay being used at a particular institution as well as the reference ranges in order to appropriately interpret results. Total serum testosterone is generally the first test that is ordered and can be measured by antibody-based assay or mass spectrometry. The antibody-based assay is widely used but has been shown, at low testosterone levels, to have high inter-technique variability and poor agreement when compared with results from mass spectrometry. Moal et al. compared five immunoassay techniques with mass spectrometry and found none of them to be reliable methods of determining low serum testosterone levels (12). These considerations should be kept in mind when evaluating a laboratory value.
Samples for testing should be drawn in the morning; at the time of peak testosterone levels. It is generally recommended that at least two levels are drawn for diagnosis. Total serum testosterone is usually sufficient, with the normal ranges varying between different laboratories. Because of this variability, there is no strict cutoff for the diagnosis of hypogonadism however typical guidelines suggest a total testosterone <350 ng/dL or free testosterone <80 ng/dL in the presence of symptoms. Therefore, each evaluation should take multiple factors into consideration including reference ranges, methods, and presence of clinical signs/symptoms.
Testosterone replacement
Once the diagnosis of hypogonadism is made in an ESRD patient, a treatment plan must be determined. The combinations of low testosterone levels and signs/symptoms consistent with hypogonadism lead to the consideration of testosterone replacement therapy. The risks and benefits of testosterone replacement have been extensively studied in the general population. It is well known that testosterone replacement leads to improvement of muscle mass and strength (13) and bone density (14,15). Improvements in energy, positive feelings, and friendliness along with decreased negative feelings including anger and irritability have been previously shown (16). Improvements in sexual function have likewise been demonstrated (16). The data for CKD or ESRD patients, however, is scant.
In 1982, Barton et al. published the effects of intramuscular testosterone replacement in six hypogonadal ESRD patients over a 6-month period. Testosterone levels markedly increased while FSH and LH levels significantly decreased (17) during the study time period. In a double blind study, van Coevorden et al. administered oral testosterone or placebo to 19 ESRD patients on dialysis. Levels of testosterone increased with falls in LH and FSH in the patients receiving testosterone; while no changes were observed in the patients receiving placebo (18). These findings suggest an improvement in biochemical levels of hormones in response to androgen replacement in ESRD patients.
Lawrence et al. evaluated the effect of testosterone replacement on sexual function in hypogonadal ESRD men on dialysis. 27 patients were administered intramuscular testosterone and while all demonstrated biochemical resolution of hypogonadism, only 3 (11.1%) experienced restoration of libido as well as fullness and duration of penile erections. Unfortunately, 2 of these 3 responders lost their response within 18 months. None of these responders had renal disease of diabetic etiology. Nineteen subjects experienced partial responses while five subjects had no response. This study also offered vacuum tumescence therapy to the 26 ESRD patients whose sexual dysfunction did not respond to testosterone. Nineteen of these patients experienced full correction of their erectile dysfunction. Four subjects noted mild fluid retention, a known side effect of testosterone therapy (19). Cangüven et al. evaluated the effect of testosterone gel treatment on nine men on dialysis with erectile dysfunction and hypogonadism. Treatment with gel significantly increased serum T levels and significantly decreased levels of FSH and LH. They found significantly improved scores on the International Index of Erectile Function (IEFF), improved intercourse satisfaction, orgasmic function, sexual desire, and overall sexual satisfaction. In addition, there was a significant increase in the frequency of intercourse. All subjects were able to complete the 6-month study without significant adverse effects (20). Chatterjee et al. studied 12 patients with hypogonadism and erectile dysfunction—4 were on hemodialysis and 8 were post-renal transplant. All patients received intramuscular monthly injections of testosterone and oral sildenafil once or twice weekly for 1 year. All 12 patients were able to participate in sexual intercourse and reported improvement in IEFF score. Post-treatment hormone levels were not reported (21). As mentioned, sexual dysfunction in the CKD population is likely multifactorial, and the combination of sildenafil and testosterone replacement targets multiple likely coexistent etiologies.
The ability of renal transplantation to improve aspects of sexual dysfunction is controversial and studies are notable for small sample sizes. Shamsa et al. prospectively evaluated 15 ESRD patients who underwent living donor transplantation and found that mean testosterone level decreased significantly after transplantation (22). IIEF scores improved in 11/15 cases but worsened in 2 cases. A study by Barroso et al. compared men on dialysis and after renal transplant and found no difference in the prevalence of erectile dysfunction. They did, however find significant difference in ability to achieve orgasm, libido, and overall sexual satisfaction (23). Other studies have also found no difference in erectile dysfunction after renal transplantation (24,25). This lack of significant improvement may be attributed to comorbidities, effect of medications, and persistent disturbed physiology.
Testosterone treatment for the correction of anemia in dialysis patients has been previously studied. In a 6-month prospective trial, Gaughan et al. studied nineteen anemic dialysis patients randomized into two groups. One group received thrice weekly recombinant erythropoietin for 26 weeks while the second group received equal doses of recombinant erythropoietin in addition to 100 mg intramuscular nandrolone decanoate weekly. At the completion of the study, both groups improved mean hematocrit but the group that received nandrolone decanoate in addition to the recombinant erythropoietin had a statistically greater increase (8.2%±4.4% vs. 3.5%±2.8%; P=0.012) (26). Teruel et al. prospectively studied the effect of testosterone treatment alone on anemic male dialysis patients. Twenty-five patients received 200 mg intramuscular nandrolone decanoate weekly for 6 months. They found an increase in both serum erythropoietin and hemoglobin (basal value: 8±0.9 g/dL; at 1 month postandrogen: 9.2±1.3 g/dL, P<0.001; at 6 months: 10.7±1.8 g/dL, P<0.001) (27).
To our knowledge, the effect of testosterone replacement on bone density and muscle mass and strength in CKD patients has not been studied. It has been shown that dialysis patients with the lowest testosterone levels score lower on tests of strength—but this is an association and a multitude of other factors may play a causal role. It is possible that testosterone replacement could have anabolic effects in this population but more studies are needed in this area. Total testosterone has been shown to correlate inversely with sRANKL levels in dialysis and may play a role in bone homeostasis in dialysis patients but more data remains to be seen.
The goal of testosterone replacement is to treat the signs and symptoms of testosterone deficiency. Once a treatment regimen is started, it is important to continue to monitor testosterone levels as well as monitor for improvement in the clinical presentation. Serum testosterone monitoring should be tailored to the type of replacement the individual is receiving. If injections are being given, levels should be measured halfway between injections. With testosterone gels, levels can be measured at any time. And with testosterone patches, levels should be measured 12 hours after application. If adequate levels (total testosterone between 400 and 900 ng/dL) are maintained without improvement in signs/symptoms, the treatment plan should be reconsidered.
Conclusions
Men with ESRD and those who have received a renal transplant are often plagued with hypogonadism. The etiology is likely multifactorial and the diagnosis is established by detection of a low testosterone level and associated clinical signs and symptoms. Testosterone replacement therapy has surged in the general population and has been shown in small studies to improve the hormonal parameters of ESRD patients. The effects of androgen replacement on sexual dysfunction in ESRD or transplant are controversial but studies suggest variable improvement. Further studies are needed to better elucidate the effects of therapy as well as to determine the effects on other clinical signs/symptoms including anemia, muscle mass, strength, bone density, and psychology in this special population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gungor O, Kircelli F, Carrero JJ, et al. Endogenous testosterone and mortality in male hemodialysis patients: is it the result of aging? Clin J Am Soc Nephrol 2010;5:2018-23. [Crossref] [PubMed]
- Albaaj F, Sivalingham M, Haynes P, et al. Prevalence of hypogonadism in male patients with renal failure. Postgrad Med J 2006;82:693-6. [Crossref] [PubMed]
- Gan EH, Pattman S, H S, Pearce S, et al. A UK epidemic of testosterone prescribing, 2001-2010. Clin Endocrinol (Oxf) 2013;79:564-70. [Crossref] [PubMed]
- Hackett G. Testosterone replacement therapy and cardiovascular events. BMJ 2014;349:g7230. [Crossref] [PubMed]
- Carrero JJ, Qureshi AR, Parini P, et al. Low serum testosterone increases mortality risk among male dialysis patients. J Am Soc Nephrol 2009;20:613-20. [Crossref] [PubMed]
- Shoskes DA, Kerr H, Askar M, et al. Low testosterone at time of transplantation is independently associated with poor patient and graft survival in male renal transplant recipients. J Urol 2014;192:1168-71. [Crossref] [PubMed]
- Stenvinkel P. Inflammation in end-stage renal disease: the hidden enemy. Nephrology (Carlton) 2006;11:36-41. [Crossref] [PubMed]
- Holley JL. The hypothalamic-pituitary axis in men and women with chronic kidney disease. Adv Chronic Kidney Dis 2004;11:337-41. [Crossref] [PubMed]
- Rosas SE, Joffe M, Franklin E, et al. Association of decreased quality of life and erectile dysfunction in hemodialysis patients. Kidney Int 2003;64:232-8. [Crossref] [PubMed]
- Türk S, Guney I, Altintepe L, et al. Quality of life in male hemodialysis patients. Role of erectile dysfunction. Nephron Clin Pract 2004;96:c21-7. [Crossref] [PubMed]
- Carrero JJ, Bárány P, Yilmaz MI, et al. Testosterone deficiency is a cause of anaemia and reduced responsiveness to erythropoiesis-stimulating agents in men with chronic kidney disease. Nephrol Dial Transplant 2012;27:709-15. [Crossref] [PubMed]
- Moal V, Mathieu E, Reynier P, et al. Low serum testosterone assayed by liquid chromatography-tandem mass spectrometry. Comparison with five immunoassay techniques. Clin Chim Acta 2007;386:12-9. [Crossref] [PubMed]
- Bhasin S, Storer TW, Berman N, et al. Testosterone replacement increases fat-free mass and muscle size in hypogonadal men. J Clin Endocrinol Metab 1997;82:407-13. [PubMed]
- Wang YJ, Zhan JK, Huang W, et al. Effects of low-dose testosterone undecanoate treatment on bone mineral density and bone turnover markers in elderly male osteoporosis with low serum testosterone. Int J Endocrinol 2013;2013:570413.
- Bouloux PM, Legros JJ, Elbers JM, et al. Effects of oral testosterone undecanoate therapy on bone mineral density and body composition in 322 aging men with symptomatic testosterone deficiency: a 1-year, randomized, placebo-controlled, dose-ranging study. Aging Male 2013;16:38-47. [Crossref] [PubMed]
- Wang C, Alexander G, Berman N, et al. Testosterone replacement therapy improves mood in hypogonadal men--a clinical research center study. J Clin Endocrinol Metab 1996;81:3578-83. [PubMed]
- Barton CH, Mirahmadi MK, Vaziri ND. Effects of long-term testosterone administration on pituitary-testicular axis in end-stage renal failure. Nephron 1982;31:61-4. [Crossref] [PubMed]
- van Coevorden A, Stolear JC, Dhaene M, et al. Effect of chronic oral testosterone undecanoate administration on the pituitary-testicular axes of hemodialyzed male patients. Clin Nephrol 1986;26:48-54. [PubMed]
- Lawrence IG, Price DE, Howlett TA, et al. Correcting impotence in the male dialysis patient: experience with testosterone replacement and vacuum tumescence therapy. Am J Kidney Dis 1998;31:313-9. [Crossref] [PubMed]
- Cangüven O, Aykose G, Albayrak S, et al. Efficacy of testosterone gel in the treatment of erectile dysfunction in hypogonadal hemodialysis patients: a pilot study. Int J Impot Res 2010;22:140-5. [Crossref] [PubMed]
- Chatterjee R, Wood S, McGarrigle HH, et al. A novel therapy with testosterone and sildenafil for erectile dysfunction in patients on renal dialysis or after renal transplantation. J Fam Plann Reprod Health Care 2004;30:88-90. [Crossref] [PubMed]
- Shamsa A, Motavalli SM, Aghdam B. Erectile function in end-stage renal disease before and after renal transplantation. Transplant Proc 2005;37:3087-9. [Crossref] [PubMed]
- Barroso LV, Miranda EP, Cruz NI, et al. Analysis of sexual function in kidney transplanted men. Transplant Proc 2008;40:3489-91. [Crossref] [PubMed]
- Al Khallaf HH. Analysis of sexual functions in male nondiabetic hemodialysis patients and renal transplant recipients. Transpl Int 2010;23:176-81. [Crossref] [PubMed]
- Mirone V, Longo N, Fusco F, et al. Renal transplantation does not improve erectile function in hemodialysed patients. Eur Urol 2009;56:1047-53. [Crossref] [PubMed]
- Gaughan WJ, Liss KA, Dunn SR, et al. A 6-month study of low-dose recombinant human erythropoietin alone and in combination with androgens for the treatment of anemia in chronic hemodialysis patients. Am J Kidney Dis 1997;30:495-500. [Crossref] [PubMed]
- Teruel JL, Marcén R, Navarro JF, et al. Evolution of serum erythropoietin after androgen administration to hemodialysis patients: a prospective study. Nephron 1995;70:282-6. [Crossref] [PubMed]


