Variant histology in bladder cancer: how it should change the management in non-muscle invasive and muscle invasive disease?
Introduction
Urinary bladder cancer (BC) is worldwide the 7th most common cancer in men and the 17th most common cancer in women, respectively (1). About 75% of newly diagnosed BC are noninvasive, while the rest are invasive with the need of more radical treatment.
The incidence of bladder carcinoma in the European Union (EU) is approximately a 100,000 new cases per year, whereas the mortality of this disease approaches up to 30,000 (1-3). BC can be classified as urothelial and non-urothelial types. Non-urothelial BC and variants of urothelial carcinoma (UC) account for up to 10–25% of all BCs (4).
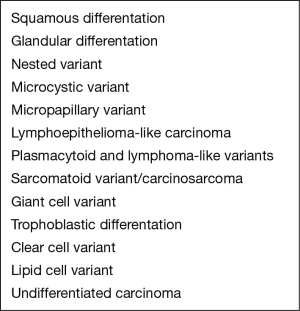
Variant histology includes any bladder malignancy other than pure urothelial cancer, such as UC with aberrant differentiation as well as pure non-UC resulting from metaplasia (5). The recent World Health Organization (WHO) classification of urothelial cancers lists 13 different histologic variants of urothelial cancer (Figure 1) (4).
Non-urothelial BC may be further subclassified as epithelial and non-epithelial non-urothelial BC (6). Approximately 90% of non-urothelial BCs are epithelial, including squamous cell carcinoma (SCC), adenocarcinoma, and small-cell carcinoma (6). Non-epithelial tumors are rare and include sarcoma, carcinosarcoma, paraganglioma, melanoma and lymphoma (6).
As most BC subtypes differ with respect to their cellular origin and thus their genetic background, the exact BC variant should be identified in every individual patient because the prognosis and therapy of choice might differ significantly (7). The observed differences in prognosis for non-urothelial BC relate to an aggressive biological behavior as well as to commonly seen advanced disease stage at the time of diagnosis (8). As in UC, hematuria is the most common symptom in non-UC as well, but some patients may present with bladder irritation symptoms and rarely even mucusuria in adenocarcinoma (9).
The primary treatment for patients with variant histology BC who present with localized disease is surgical. For invasive tumors, radical cystectomy (RC) should be performed including a pelvic lymph node dissection (10). However, little data on the treatment of non-urothelial BCs is currently available, leading to low-level evidence as well as recommendations. Mixed histology is usually not highlighted in clinical trials, such that no clear-cut data or recommendations can be extracted and used for clinical recommendations. As pure non-urothelial tumors are usually not included in phase III trials, routine pre- or postoperative chemotherapy (CTX) or radiotherapy (RTX) are currently not recommended due to a lack of data (7).
The presence of variant histology BC represents high-risk BC even if not muscle-invasive and therefore recommendations generally include early aggressive intervention with RC, especially in those patients with variant histology such as pure SCC, adenocarcinoma and sarcomatoid cancer (7).
In patients with advanced non-urothelial BC or those patients who cannot undergo surgery, including those with metastatic disease, treatment options used are palliative care, RTX or CTX. However, non-UCs of the bladder seem to be associated with an aggressive course and poor outcome with standard chemotherapeutic regimens (11). As there is no data showing a survival or quality-of-life benefit from CTX for non-urothelial BCs, palliative care as an alternative to CTX should be offered and the shortcomings of available treatments should be discussed with the patients (7).
SCC
In North America and Europe SCC accounts for 3% to 5% of BCs; however, in areas with a high prevalence of Schistosoma haematobium infection as in East Africa and the Middle East SCC can be found in up to 75% of BCs (12).
Risk factors for the development of SCC include chronic urinary tract infection, bladder calculi, pelvic radiation therapy, intravesical treatment with Bacillus Calmette-Guérin (BCG), as well as exposure to cyclophosphamide (8). Smoking also seems to be a risk factor as is known for pure UC as well (13).
The optimal treatment for SCC of the bladder remains largely unclear. Up to now, the primary treatment for SCC in localized stages is surgical only as there is limited data regarding efficacy of intravesical therapy in SCC, which suggests inferior performance in SCC with progression rates to MIBC of up to 45% within 2 years and subsequent death in almost all patients with progression (14). The dominating role of surgery is adapted from observational and retrospective data: a retrospective study which included 27 patients with pure SCC of the bladder treated between 1988 and 2003 reported that survival was better among patients who were able to have a cystectomy as compared to CTX and/or RTX, only (15). The 2-year recurrence-free survival (RFS) and 2-year overall survival (OS) rates were 32.8% and 47.6%, respectively, with a median follow-up of 15.3 months in survivors. While there is probably huge selection bias affecting these results, surgery, even in terms of tumor volume reduction seems to be beneficial when possible. A Surveillance, Epidemiology, and End Results (SEER) database analysis of 1,422 patients with pure SCC compared to a total of 107,613 UCs diagnosed between 1988 and 2003 showed that SCC appears to be more aggressive than UC after adjusting for stage and other prognostic factors (16). Among patients who did not undergo RC, a SCC subtype was a strong and independent predictor of poor 2-year survival for all stages compared with UC (16). Furthermore, the 2-year mortality rate in patients with American Joint Committee on Cancer (AJCC) stage III and IV SCC was again worse for SCC than for UC, regardless even of whether RC was performed or not (16). However, in cases in which the tumor was confined to the bladder wall and the bladder was removed as a part of the initial treatment, interestingly SCC histologic features were not associated with increased mortality when compared to UC (16). In patients with SCC who had undergone RC for AJCC stage I (T1N0M0) and II (T2N0M0) disease, the 2-year mortality rate was 11% and 27% compared to UC with a mortality rate of 16% and 23%, respectively, thus underlining the importance of timely diagnosis and aggressive surgical treatment (16).
Due to the more favorable diagnosis in bladder-confined SCC without significant differences to UC as well as high local and systemic recurrence rates of up to 50% within a few months after RC, which usually are reasons for subsequent death of disease, neoadjuvant (NAC) therapy regimens should be considered for possible downstaging of tumours as well as prevention of recurrence (15). Data however are sparse regarding that matter. In a small study, 25 patients who had muscle-invasive pure SCC of the bladder received NAC RTX of the bladder and overall, 40% of patients showed downstaging to non-muscle-invasive disease at time of cystectomy with even 24% showing pT0 disease and none of them having recurrence of SCC on subsequent follow-up (17). The median survival of patients with a pelvic recurrence (seven patients) was only 9 months compared to 86.7 months (P=0.03) without recurrence (17). The overall 5-year survival rate for all patients was 50% (17).
NAC RTX can therefore be used in order to attempt downsizing of the tumour to non-muscle-invasive disease, which seems to be connected with significantly lower risk of local recurrence of the cancer and significantly longer median survival (17,18).
The role of RTX is important for patients with SCC as this subtype is resistant to most CTX regimens usually used for advanced and metastatic pure UC (18). So in locally advanced stages with unresectable SCC of the bladder, RTX with or without adjunctive CTX can be used as a treatment attempt. Recommended is the use of CTX regimens, such as the combination of paclitaxel, carboplatin, and gemcitabine, which have demonstrated efficacy in patients with SCC in other locations (17). However, primary RTX with or without CTX is still largely associated with poor results in most series with 5-year OS estimates for locally advanced and metastatic SCC of around 5–18% in larger studies (19,20).
Adenocarcinoma
Primary adenocarcinoma of the bladder is rare and accounts for less than 2% of all BCs in North America and Europe (13). There are different types of adenocarcinomas that have been described, including glandular, colloid, papillary, signet-ring and clear cell (21). Adenocarcinomas can be further categorized as urachal and non-urachal, where urachal adenocarcinomas represent 10% of all primary adenocarcinomas of the bladder (22).
Compared to those with non-urachal tumors, patients with urachal adenocarcinoma are more likely to be younger (median age 56 vs. 69 years) and female (45% vs. 36%) (22). Furthermore, urachal lesions were less likely to be high grade (35% vs. 66%), but more likely to involve distant metastases (30% vs. 15%) (22). Still, patients with urachal adenocarcinoma have a better overall prognosis than those with primary bladder adenocarcinoma, which might be partly due to the fact that urachal adenocarcinoma is often diagnosed in younger patients with less comorbidity (22). In a retrospective study from Tata Memorial Hospital including 48 patients with adenocarcinoma (21 urachal and 27 non-urachal) of the bladder, the 5-year OS was 37% overall, with urachal tumours showing higher OS rates of 45.7% compared to 29.9% for non-urachal tumours, even if not statistically significant probably due to low numbers (23). Moreover, a SEER database study including a total of 151 urachal and 1,374 non-urachal adenocarcinomas of the bladder found that the 5-year OS was still more favorable for patients with urachal adenocarcinoma (48%) than those with non-urachal adenocarcinoma (35%) after adjusting for grade, histologic subtype, stage, age, gender, and surgical management (22). This suggests that intrinsic anatomical and molecular differences between urachal adenocarcinoma and bladder adenocarcinoma might also contribute to the observed different clinical outcome.
Urachal adenocarcinoma
Usually, urachal adenocarcinomas appear in the urachal remnant at the dome of the bladder and often extend into the prevesical space. As most urachal adenocarcinomas produce mucin (90%), mucusuria can be found in a number of patients as well as hematuria and a palpable lower abdominal mass (24). Unfortunately, urachal adenocarcinomas often present primarily with locally advanced disease.
Surgery is the recommended primary treatment for adenocarcinomas of the bladder. Due to the location of the tumor, intraluminal treatment with CTX or resection cannot be performed. Patients with an urachal carcinoma may undergo partial cystectomy rather than RC due to its favorable location at the bladder dome, as long as the tumor can be removed in toto. The resection should, however, always include an en bloc resection of the bladder dome, urachal ligament, and umbilicus (25). As up to 7% of urachal adenocarcinomas involve the umbilicus, the relapse rate is generally higher in patients that do not undergo en-bloc resection (26).
A retrospective analysis of 66 cases seen at the Mayo Clinic between 1951 and 2004 showed that early and complete extended partial cystectomy, including umbilectomy, is critical for the survival of patients with urachal adenocarcinoma (25). Associated with poor outcome were positive surgical margins [hazard ratio (HR), 4.7 (95% CI, 2.2–9.8)], high tumor grade [HR, 3.6 (95% CI, 1.7–7.7)], positive local lymph nodes [HR, 5.1 (95% CI, 2.2–11.5)], metastases at diagnosis [HR, 3.3 (95% CI, 1.6–6.8)], advanced tumor stage [HR, 4.8 (95% CI, 2.0–11.3)], need for primary radiation therapy before surgery [HR, 2.9 (95% CI, 1.1–7.7)], and failure to perform umbilectomy [HR, 3.0 (95% CI, 1.3–6.8)] (all P<0.05). No survival benefit was noted for extended lymphadenectomy or adjuvant therapy (CTX, RTX, or both) (25).
Currently, there is no evidence of efficacy for any particular CTX agent or regimen neither NAC or adjuvant and RTX seems to be ineffective (26). Further, no effective treatment was yet identified for patients with metastatic urachal adenocarcinoma due to its highly aggressive behaviour. However, the combination of 5-fluorouracil, leucovorin, gemcitabine, and cisplatin seems to be promising in this disease. At the moment a phase-II trial with this regimen is ongoing (M.D. Anderson Cancer Center) (27). In a retrospective study including 42 patients with urachal carcinoma, 26 patients developed metastatic disease and 20 received CTX, showing median OS from commencement of CTX to be 20 months (26). Of the 9 patients receiving 5-fluorouracil and cisplatin containing regimens, three showed a significant response (26). In addition, modified FOLFOX-based CTX has been used for metastatic urachal cancer. For example, in a retrospective study with five patients receiving mFOLFOX6 (oxaliplatin, leucovorin, 5-FU), two of five patients showed an objective response and the median survival time was 42 months (range, 18–46 months) (28). However, data on the effectiveness of this regimen in urachal cancer is currently still limited to a few case reports.
Non-urachal adenocarcinoma
Non-urachal adenocarcinomas are often papillary or flat lesions infiltrating in the bladder and a diffusely thickened bladder wall with stranding in the surrounding fat is frequently found on imaging; typical manifestations of metastases, if present, are the peritoneum, local lymph nodes, and the lungs (29). The 5-year survival rates are low (11–61%) depending on tumour stage, size and grade (30). However, in early, localized stages with well differentiated tumours, a transurethral resection (TUR-BT) or partial cystectomy is a possible treatment option. There is currently no study available on the effect of intravesical immuno- or CTX. However, a case report of three patients with stage 1 adenocarcinoma of the bladder treated with BCG showed good clinical response with disease free survival of 58 months (23).
For patients with invasive non-urachal adenocarcinomas RC with pelvic lymphadenectomy analog to UC is recommended (19). The role for NAC or adjuvant CTX as well as RTX in locally advanced or even metastatic adenocarcinoma of the bladder is not clear.
A prospective trial of ifosfamide, paclitaxel and cisplatin in 20 men with advanced non-urothelial BC, 11 of which with adenocarcinoma, showed an overall response rate of 35% (95% CI, 15–59%) and a median survival of 24.8 months (95% CI, 10.2–32.3 months) (11). Further, an available retrospective series of 21 patients, including 14 with adenocarcinoma, reported a comparable response rate of 36% to first-line cisplatin-containing regimens, but report a shorter median survival of only 13 months (95% CI, 6.8–19.2 months) from the day of first-line CTX (31). This difference in survival might be due to the mixed patient population in the latter study and the potential selection bias in patients chosen to be included in a prospective study regarding overall performance status as well as disease burden. Unfortunately, there is no data on the effectiveness of taxanes and gemcitabine in this patient population. The average survival in patients with locally advanced, unresectable disease without CTX was less than 1 year (31).
Small cell carcinoma
Small cell carcinoma of the bladder (SCBC) is a rare and aggressive type of bladder carcinoma, and there is evidence that both varieties of histology, SCBC and UC, originate from the same cells in the urothelium (32). SCBC shows similar characteristics as small cell carcinomas of the lung including the capacity of ectopic hormone production, which can lead to clinically significant hypercalcemia or hypophosphatemia (33). About 0.5% of all bladder malignancies are estimated to present as SCBC (34). It is noteworthy that any amount of small cell histology should lead to the classification of SCBC, as this type of histology determines the prognosis of the patient (4). Untreated, SCBC has, like the pulmonary counterpart a very poor prognosis with an OS of less than 18 months over all stages (33,35). Even with multimodal treatment regimens, survival for disease limited to the bladder, limited to the pelvis or metastatic is reported to be as low as 36%, 24% and 0% at 2 years (36). When compared to UC, SCBC tends to present with higher rates of advanced stage (pT3/4, 84% vs. 46%) and lymph node involvement (37% vs. 20%) (37). Despite these differences, when the 68 patients with SCBC included in this study of Kaushik et al. were matched (1:2) to patients with UC according to TNM-stage, no statistically significant difference was seen in 5-year cancer-specific survival (CSS, 30% vs. 38%) and 5-year OS (27% vs. 29%) between SCBC and UC patients (37). On the contrary, Geynisman and colleagues, using data out of the National Cancer Data Base including a total of 960 advanced SCBC and 27,796 UC patients, found that, while survival of patients with M1 disease did not differ between SCBC and UC, patients with N+M0 disease did live shorter when they had SCBC (median OS 13.0 vs. 17.3 months) (38).
TUR-BT is routinely used for initial diagnosis of SCBC, however, there is no data on treatment efficacy of TUR-BT alone or in combination with intravesical therapy in these patients, who also rarely present with non-invasive disease, where such an approach could be considered. Further, due to the aggressive behavior of SCBC, early, upfront RC should be considered in patients with true non-invasive disease (pTa), whereas multimodal therapy regimens should be used in invasive disease stages (≥ pT1).
RTX and CTX as a local and systemic adjunct to surgical resection via TUR-BT were investigated in two studies with a total of 28 patients (39,40). Complete remission rates after RTX to the pelvis and CTX with multiple regimens including MVAC, EP, VAC and others were reported to be as high as 73% and 88% on subsequent TUR-BT, but despite high rates of local tumor control, 3-year metastasis-free survival and OS were only 27% and 24% in one study, while median OS was 32.5 months in the other (39,40). This discrepancy between good local tumor control and high rate of metastases and subsequent death underline the aggressiveness of this variant and warrants for aggressive surgical treatment in combination with systemic therapies in these patients.
As indicated above, systemic CTX is an integral part of the treatment of patients with SCBC. In studies where patients were deemed unfit for or did not receive CTX, the survival results were very poor despite surgical treatment and presence of localized disease, with median survival times of only 3–5 months, while patients receiving local treatment and CTX lived between 15–33 months (38,41,42). As all these reports are retrospective, significant selection bias has to be kept in mind when interpreting these results.
Due to the known importance of systemic CTX in SCBC, multiple studies investigated the value of NAC before RC. In a retrospective analysis including 125 patients with non-metastatic SCBC (clinical stage ≤ T4aN0M0) 95 were found to be surgical candidates (43). Patients receiving NAC with different regimens (n=48) were downstaged to non-muscle invasive disease in 62% vs. only 9% in patients with RC alone, showing the efficacy of CTX in this disease (43). Survival was also markedly improved (median OS was 159.9 vs. 18.3 months respectively) (43). Further, after showing similarly favorable results in 46 patients, of whom 21 received NAC and reached 5-year OS of 73%, Siefker-Radtke and colleagues performed a prospective phase II trial, treating 30 patients (18 non-metastatic and 12 metastatic) with alternating doublet therapy containing ifosfamide and doxorubicin as well as etoposide and cisplatin (44,45). In non-metastatic patients, downstaging to non-muscle invasive disease was seen in 78% of patients receiving NAC before RC, which was associated with a median OS of 58 months (45). In patients with metastatic disease, the objective response rate to this regimen was 67% and median OS was 13.3 months (45). Systemic CTX in the postoperative setting also seems to have some efficacy as 5-year OS was found to be 43% after RC plus AC vs. only 20% for patients receiving RC alone (37).
Overall, in patients with non-invasive SCBC (pTa), early upfront cystectomy without previous CTX can be an option, however, SCBC rarely presents in a non-invasive stage. Therefore, due to the above presented limited survival results with extirpative therapy alone, the treatment for SCBC should be multimodal whenever possible and should contain RC as well as systemic CTX with or without RTX.
Sarcomatoid carcinoma
Purely sarcomatoid differentiated carcinomas of the bladder (SBC) are only described in small case series due to its rare appearance (around 0.3% in all bladder malignancies), which precludes robust suggestions regarding its treatment as compared to standard UC (46). However, the true incidence of SBC is likely to be underestimated, likely due to the previously limited awareness of this variant and limitations in immunohistochemical staining technique. More commonly than pure SBC, sarcomatoid features are found in parts of UC (in up to 6%), but also for these patients, the mere presence of sarcomatoid features seems to be an adverse pathological event (47). The aggressiveness might be a result of either anaplastic changes or dedifferentiation related to a process of losing cell adhesion molecules (48). Almost all of SBC are poorly differentiated or undifferentiated and the majority of patients with SBC presented with at least muscle-invasive disease and many with stage IV carcinoma. In comparison to UC, SBC presents with higher rates of advanced stage (T3-4 34% vs. 28%) and metastatic disease (N+/M+ >20% vs. 10%) and harbors worse prognosis even after stratification for pathologic criteria (49).
There are no studies reporting direct outcomes of TUR-BT alone with or without intravesical therapy due to the rarity of the disease, but most experts agree to skip bladder preservative approaches to prevent delay to definite extirpative therapy. Further, results from the SEER database advocate RC over partial cystectomy as 2-year survival was 14% in patients undergoing bladder sparing as compared to 52% in patients treated with RC underline these recommendations (50,51). This is in line with other available reports, where median survival was 14 months with 54% of patients alive at 1 year after cancer-directed surgery (TUR-BT, partial or RC) (50).
Due to the high rate of recurrence and cancer-specific death after surgical therapy, multimodal approaches with perioperative CTX and RTX have been advocated, however, data are scarce as well. Descriptive analyses of SBC patients receiving TUR-BT with and without RTX, as well as additional RC and CTX in some patients showed survival times of 1 to 73 months (mean 9.8 months), but do not allow for interpretation of treatment specific outcomes (52). A case series from MDACC reported on their experience with NAC for SCB. In patients receiving NAC before RC, a pT0 rate of 45% at time of cystectomy was achieved as compared to 12% after TUR-BT and RC alone, however, due to small sample size this did not translate into a survival benefit (53).
Up to this date, no larger trial investigated the influence of different treatment options in patients with SBC, therefore the true value of CTX per se, different CTX regimens, RTX and surgery as well combinations of those cannot be fully estimated.
Plasmacytoid carcinoma
Plasmacytoid variant of histology in bladder cancer (PBC) is, even more than SBC, a very rare type of BC, which is easily missed in histologic workup (47). There are no larger trials available; investigations are currently limited to case reports, small case series with usually less than 20 patients and one report on advanced stage PBC with a total of 30 cases (54-58). Compared to conventional UC and micropapillary bladder carcinoma (MPBC), patients with PBC seem to have a worse outcome when treated with current standard treatments (mainly RC with adjuvant cisplatin-based CTX), with a median OS of 27.4 months compared to 62.2 and 64.2 months for conventional UC and MPBC, respectively (59). Also, there seems to be an alternate way of systemic spread, as spread alongside the ureters into the retroperitoneum, into the peritoneal cavity as well as other uncommon distant sites is reported (60).
There are no distinct reports to draw conclusions about the value of TUR-BT with or without adjunct intravesical therapy or early cystectomy due to the rarity of the disease. In one larger series comparing 30 PBCs to 278 UCs, PBC was significantly more likely to present in more advanced stages (pT3-4 73% vs. 40%) and with lymph node involvement (70% vs. 25%) (58). Median OS and CSS were 19 and 22 months, respectively for PBC, whereas these endpoints were not reached in the UC comparator patients at 68 months (58). Due to these results, early RC should be recommended whenever possible. Regarding CTX or RTX, there are not more than case reports of multimodal treatment regimens available, precluding strong recommendations regarding specific therapeutic regimens. Commonly described CTX agents are gemcitabine and cisplatin (55,59). However, one has to keep in mind that case reports are usually likely to be biased towards unexpectedly favorable disease courses.
Micropapillary carcinoma
MPBC is a variant form of infiltrating UC with an incidence from 0.6% up to 1% (61,62). Early case series often reported advanced stage at time of diagnosis and poor prognosis (5-year OS 25% overall) (61). Conversely, the currently largest case series of 100 patients with MPBC actually reported a higher proportion of non-muscle invasive disease (44%) and generally better clinical outcomes (5-year OS 51%). However, most patients with non-muscle invasive disease were pT1 indicating beginning tumor invasion (63).
Available data indicate that especially in the group of patients with pT1 or carcinoma in situ (CIS) the decision towards early RC seems to be beneficial. In case series including about 40 patients each with pT1 or CIS on initial TUR-BT, the 5-year cancer-specific mortality rate was lower when immediate RC was performed (17%) as compared to more conservative treatment with TUR-BT +/‒ BCG and possible deferred RC within 3 months (25%) (64,65). Further, most of the specimens of patients who underwent deferred RC showed advanced disease after intravesical therapy with BCG suggesting no beneficial effect in this histological subtype (64,65). Recently Jackson et al. aimed to identify patients who might be managed without immediate RC distinguished all non-muscle invasive MPBC tumors (n=40) into superficial (pTa) and invasive carcinomas (pT1) (66). Unsurprisingly, the authors reported that superficial MPBC is associated with higher survival rates (median OS 63 vs. 47 months), and concluded, that those might therefore be managed more conservatively with TUR-BT and possible deferred RC in selected patients (66). Still there is evidence that intravesical therapy is less effective in variants as compared to UC, with progression rates of up to 70% after 8 months, therefore advocating generously for early RC in all non-muscle invasive MPBC (14,63).
There are few reports regarding the effect of NAC in MPBC. In a study including 44 patients with MPBC and clinical stage ≥ cT2 of which 29 underwent NAC (21 gemcitabine and cisplatin, 2 gemcitabine, cisplatin and sunitinib, 2 gemcitabine and carboplatin, 2 paclitaxel, gemcitabine and cisplatin, 1 methotrexate, vinblastine, doxorubicine and cisplatin), downstaging to pT0/CIS only occurred in 45% of the patients receiving NAC vs. only 13% of the patients with immediate RC (67). Further, downstaging to pT1 occurred in another 10%. Downstaging to pT0/CIS was also associated with lower rates of MPBC recurrence (21% vs. 79%) and improved OS (92% vs. 25%) after 2 years (67). Ghoneim and colleagues report the possibility of significant residual disease after platin-based NAC associated with poor outcomes in a relevant proportion of patients treated with NAC, underlining the heterogeneity of possible responses in MPBC (65). Further, one group even reports worse survival results for patients receiving NAC as compared to patients undergoing immediate RC (5-year OS 32% vs. 71%). However, this possibly represents selection bias as in this non-randomized study, patients with adverse criteria at diagnosis were probably more likely to receive NAC (63).
The role of platin-based AC was retrospectively analyzed in 31 cases of MPBC compared to 235 patients with conventional UC showing 5-year CSS of 24% (MPBC) vs. 47% (UC), suggesting lower susceptibility of MPBC to platinum as conventional UC (68). Despite the limited data, the higher rates of recurrence allow to question the efficacy and role of AC in MPBC with the currently routinely used regimens.
Conclusions
The management of variant histology BC is challenging; especially the diagnosis and the choice of adequate therapy are difficult due to a lack of profound data on these settings. Recommendations for therapy are mostly based on retrospective case series as well as extrapolation of data from pure urothelial BC. Especially the sensitivity of variant histology BC to multimodal therapy, including CTX, radiation and intravesical agents, remains unknown. Moreover, variant histology BC often presents in an advanced stage of disease, which further complicates treatment decisions in the face of limited date. For most non-metastatic non-UC of the bladder early radical surgery is strongly recommended in a localized disease setting, in certain variants (SCBC) even in combination with multimodal approaches. For advanced disease stages, radical surgical approaches embedded in further systemic therapy are advocated whenever possible. In this regard multi-institutional, international, prospective collaborative efforts are needed to clarify the distinct prognosis of these patients and to determine optimal therapy regimens.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Burger M, Catto JW, Dalbagni G, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol 2013;63:234-41. [Crossref] [PubMed]
- Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013;49:1374-403. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [Crossref] [PubMed]
- Chalasani V, Chin JL, Izawa JI. Histologic variants of urothelial bladder cancer and nonurothelial histology in bladder cancer. Can Urol Assoc J 2009;3:S193-8. [Crossref] [PubMed]
- Bertz S, Hartmann A, Knüchel-Clarke R, et al. Specific types of bladder cancer. Pathologe 2016;37:40-51. [Crossref] [PubMed]
- Helpap B. Nonepithelial neoplasms of the urinary bladder. Virchows Arch 2001;439:497-503. [Crossref] [PubMed]
- Willis D, Kamat AM. Nonurothelial bladder cancer and rare variant histologies. Hematol Oncol Clin North Am 2015;29:237-52. viii. [Crossref] [PubMed]
- Dahm P, Gschwend JE. Malignant non-urothelial neoplasms of the urinary bladder: a review. Eur Urol 2003;44:672-81. [Crossref] [PubMed]
- Grignon DJ, Ro JY, Ayala AG, et al. Primary adenocarcinoma of the urinary bladder. A clinicopathologic analysis of 72 cases. Cancer 1991;67:2165-72. [Crossref] [PubMed]
- Crozier J, Papa N, Sengupta S, et al. Changing practice of pelvic lymph node dissection in management of primary bladder cancer. Minerva Urol Nefrol 2016;68:106-11. [PubMed]
- Galsky MD, Iasonos A, Mironov S, et al. Prospective trial of ifosfamide, paclitaxel, and cisplatin in patients with advanced non-transitional cell carcinoma of the urothelial tract. Urology 2007;69:255-9. [Crossref] [PubMed]
- Mostafa MH, Sheweita SA, O'Connor PJ. Relationship between schistosomiasis and bladder cancer. Clin Microbiol Rev 1999;12:97-111. [PubMed]
- Kantor AF, Hartge P, Hoover RN, et al. Epidemiological characteristics of squamous cell carcinoma and adenocarcinoma of the bladder. Cancer Res 1988;48:3853-5. [PubMed]
- Gofrit ON, Yutkin V, Shapiro A, et al. The response of variant histology bladder cancer to intravesical immunotherapy compared to conventional cancer. Front Oncol 2016;6:43. [Crossref] [PubMed]
- Kassouf W, Spiess PE, Siefker-Radtke A, et al. Outcome and patterns of recurrence of nonbilharzial pure squamous cell carcinoma of the bladder: a contemporary review of The University of Texas M D Anderson Cancer Center experience. Cancer 2007;110:764-9. [Crossref] [PubMed]
- Scosyrev E, Yao J, Messing E. Urothelial carcinoma versus squamous cell carcinoma of bladder: is survival different with stage adjustment? Urology 2009;73:822-7. [Crossref] [PubMed]
- Hussain M, Vaishampayan U, Du W, et al. Combination paclitaxel, carboplatin, and gemcitabine is an active treatment for advanced urothelial cancer. J Clin Oncol 2001;19:2527-33. [PubMed]
- Serretta V, Pomara G, Piazza F, et al. Pure squamous cell carcinoma of the bladder in western countries. Report on 19 consecutive cases. Eur Urol 2000;37:85-9. [Crossref] [PubMed]
- Anderström C, Johansson SL, von Schultz L. Primary adenocarcinoma of the urinary bladder. A clinicopathologic and prognostic study. Cancer 1983;52:1273-80. [Crossref] [PubMed]
- Johnson DE, Schoenwald MB, Ayala AG, et al. Squamous cell carcinoma of the bladder. J Urol 1976;115:542-4. [PubMed]
- Fiter L, Gimeno F, Martin L, et al. Signet-ring cell adenocarcinoma of bladder. Urology 1993;41:30-3. [Crossref] [PubMed]
- Wright JL, Porter MP, Li CI, et al. Differences in survival among patients with urachal and nonurachal adenocarcinomas of the bladder. Cancer 2006;107:721-8. [Crossref] [PubMed]
- Krabbe LM, Svatek RS, Shariat SF, et al. Bladder cancer risk: Use of the PLCO and NLST to identify a suitable screening cohort. Urol Oncol 2015;33:65.e19-25. [Crossref] [PubMed]
- Sheldon CA, Clayman RV, Gonzalez R, et al. Malignant urachal lesions. J Urol 1984;131:1-8. [PubMed]
- Ashley RA, Inman BA, Sebo TJ, et al. Urachal carcinoma: clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer 2006;107:712-20. [Crossref] [PubMed]
- Siefker-Radtke AO, Gee J, Shen Y, et al. Multimodality management of urachal carcinoma: the M. D. Anderson Cancer Center experience. J Urol 2003;169:1295-8. [Crossref] [PubMed]
- Siefker-Radtke A. Urachal carcinoma: surgical and chemotherapeutic options. Expert Rev Anticancer Ther 2006;6:1715-21. [Crossref] [PubMed]
- Yanagihara Y, Tanji N, Miura N, et al. Modified FOLFOX6 chemotherapy in patients with metastatic urachal cancer. Chemotherapy 2013;59:402-6. [Crossref] [PubMed]
- Hughes MJ, Fisher C, Sohaib SA. Imaging features of primary nonurachal adenocarcinoma of the bladder. AJR Am J Roentgenol 2004;183:1397-401. [Crossref] [PubMed]
- Dandekar NP, Dalal AV, Tongaonkar HB, et al. Adenocarcinoma of bladder. Eur J Surg Oncol 1997;23:157-60. [Crossref] [PubMed]
- Hong JY, Choi MK, Uhm JE, et al. Palliative chemotherapy for non-transitional cell carcinomas of the urothelial tract. Med Oncol 2009;26:186-92. [Crossref] [PubMed]
- Cheng L, Jones TD, McCarthy RP, et al. Molecular genetic evidence for a common clonal origin of urinary bladder small cell carcinoma and coexisting urothelial carcinoma. Am J Pathol 2005;166:1533-9. [Crossref] [PubMed]
- Oesterling JE, Brendler CB, Burgers JK, et al. Advanced small cell carcinoma of the bladder. Successful treatment with combined radical cystoprostatectomy and adjuvant methotrexate, vinblastine, doxorubicin, and cisplatin chemotherapy. Cancer 1990;65:1928-36. [Crossref] [PubMed]
- Blomjous CE, Vos W, De Voogt HJ, et al. Small cell carcinoma of the urinary bladder. A clinicopathologic, morphometric, immunohistochemical, and ultrastructural study of 18 cases. Cancer 1989;64:1347-57. [Crossref] [PubMed]
- Fahed E, Hansel DE, Raghavan D, et al. Small cell bladder cancer: biology and management. Semin Oncol 2012;39:615-8. [Crossref] [PubMed]
- Pasquier D, Barney B, Sundar S, et al. Small cell carcinoma of the urinary bladder: a retrospective, multicenter rare cancer network study of 107 patients. Int J Radiat Oncol Biol Phys 2015;92:904-10. [Crossref] [PubMed]
- Kaushik D, Frank I, Boorjian SA, et al. Long-term results of radical cystectomy and role of adjuvant chemotherapy for small cell carcinoma of the bladder. Int J Urol 2015;22:549-54. [Crossref] [PubMed]
- Geynisman DM, Handorf E, Wong YN, et al. Advanced small cell carcinoma of the bladder: clinical characteristics, treatment patterns and outcomes in 960 patients and comparison with urothelial carcinoma. Cancer Med 2016;5:192-9. [Crossref] [PubMed]
- Bex A, de Vries R, Pos F, et al. Long-term survival after sequential chemoradiation for limited disease small cell carcinoma of the bladder. World J Urol 2009;27:101-6. [Crossref] [PubMed]
- Bryant CM, Dang LH, Stechmiller BK, et al. Treatment of small cell carcinoma of the bladder with chemotherapy and radiation after transurethral resection of a bladder tumor. Am J Clin Oncol 2016;39:69-75. [Crossref] [PubMed]
- Bex A, Nieuwenhuijzen JA, Kerst M, et al. Small cell carcinoma of bladder: a single-center prospective study of 25 cases treated in analogy to small cell lung cancer. Urology 2005;65:295-9. [Crossref] [PubMed]
- Mukesh M, Cook N, Hollingdale AE, et al. Small cell carcinoma of the urinary bladder: a 15-year retrospective review of treatment and survival in the Anglian Cancer Network. BJU Int 2009;103:747-52. [Crossref] [PubMed]
- Lynch SP, Shen Y, Kamat A, et al. Neoadjuvant chemotherapy in small cell urothelial cancer improves pathologic downstaging and long-term outcomes: results from a retrospective study at the MD Anderson Cancer Center. Eur Urol 2013;64:307-13. [Crossref] [PubMed]
- Siefker-Radtke AO, Dinney CP, Abrahams NA, et al. Evidence supporting preoperative chemotherapy for small cell carcinoma of the bladder: a retrospective review of the M. D. Anderson cancer experience. J Urol 2004;172:481-4. [Crossref] [PubMed]
- Siefker-Radtke AO, Kamat AM, Grossman HB, et al. Phase II clinical trial of neoadjuvant alternating doublet chemotherapy with ifosfamide/doxorubicin and etoposide/cisplatin in small-cell urothelial cancer. J Clin Oncol 2009;27:2592-7. [Crossref] [PubMed]
- Torenbeek R, Blomjous CE, de Bruin PC, et al. Sarcomatoid carcinoma of the urinary bladder. Clinicopathologic analysis of 18 cases with immunohistochemical and electron microscopic findings. Am J Surg Pathol 1994;18:241-9. [Crossref] [PubMed]
- Shah RB, Montgomery JS, Montie JE, et al. Variant (divergent) histologic differentiation in urothelial carcinoma is under-recognized in community practice: impact of mandatory central pathology review at a large referral hospital. Urol Oncol 2013;31:1650-5. [Crossref] [PubMed]
- Ikegami H, Iwasaki H, Ohjimi Y, et al. Sarcomatoid carcinoma of the urinary bladder: a clinicopathologic and immunohistochemical analysis of 14 patients. Hum Pathol 2000;31:332-40. [Crossref] [PubMed]
- Wright JL, Black PC, Brown GA, et al. Differences in survival among patients with sarcomatoid carcinoma, carcinosarcoma and urothelial carcinoma of the bladder. J Urol 2007;178:2302-6; discussion 2307. [Crossref] [PubMed]
- Wang J, Wang FW, Lagrange CA, et al. Clinical features of sarcomatoid carcinoma (carcinosarcoma) of the urinary bladder: analysis of 221 cases. Sarcoma 2010;2010.
- Malla M, Wang JF, Trepeta R, et al. Sarcomatoid carcinoma of the urinary bladder. Clin Genitourin Cancer 2016;14:366-72. [Crossref] [PubMed]
- Lopez-Beltran A, Pacelli A, Rothenberg HJ, et al. Carcinosarcoma and sarcomatoid carcinoma of the bladder: clinicopathological study of 41 cases. J Urol 1998;159:1497-503. [Crossref] [PubMed]
- Black PC, Brown GA, Dinney CP. The impact of variant histology on the outcome of bladder cancer treated with curative intent. Urol Oncol 2009;27:3-7. [Crossref] [PubMed]
- Nigwekar P, Tamboli P, Amin MB, et al. Plasmacytoid urothelial carcinoma: detailed analysis of morphology with clinicopathologic correlation in 17 cases. Am J Surg Pathol 2009;33:417-24. [Crossref] [PubMed]
- Fritsche HM, Burger M, Denzinger S, et al. Plasmacytoid urothelial carcinoma of the bladder: histological and clinical features of 5 cases. J Urol 2008;180:1923-7. [Crossref] [PubMed]
- Mai KT, Park PC, Yazdi HM, et al. Plasmacytoid urothelial carcinoma of the urinary bladder report of seven new cases. Eur Urol 2006;50:1111-4. [Crossref] [PubMed]
- Lopez-Beltran A, Requena MJ, Montironi R, et al. Plasmacytoid urothelial carcinoma of the bladder. Hum Pathol 2009;40:1023-8. [Crossref] [PubMed]
- Kaimakliotis HZ, Monn MF, Cary KC, et al. Plasmacytoid variant urothelial bladder cancer: is it time to update the treatment paradigm? Urol Oncol 2014;32:833-8. [Crossref] [PubMed]
- Keck B, Wach S, Stoehr R, et al. Plasmacytoid variant of bladder cancer defines patients with poor prognosis if treated with cystectomy and adjuvant cisplatin-based chemotherapy. BMC Cancer 2013;13:71. [Crossref] [PubMed]
- Ricardo-Gonzalez RR, Nguyen M, Gokden N, et al. Plasmacytoid carcinoma of the bladder: a urothelial carcinoma variant with a predilection for intraperitoneal spread. J Urol 2012;187:852-5. [Crossref] [PubMed]
- Johansson SL, Borghede G, Holmäng S. Micropapillary bladder carcinoma: a clinicopathological study of 20 cases. J Urol 1999;161:1798-802. [Crossref] [PubMed]
- Alvarado-Cabrero I, Sierra-Santiesteban FI, Mantilla-Morales A, et al. Micropapillary carcinoma of the urothelial tract. A clinicopathologic study of 38 cases. Ann Diagn Pathol 2005;9:1-5. [Crossref] [PubMed]
- Kamat AM, Dinney CP, Gee JR, et al. Micropapillary bladder cancer: a review of the University of Texas M. D. Anderson Cancer Center experience with 100 consecutive patients. Cancer 2007;110:62-7. [Crossref] [PubMed]
- Spaliviero M, Dalbagni G, Bochner BH, et al. Clinical outcome of patients with T1 micropapillary urothelial carcinoma of the bladder. J Urol 2014;192:702-7. [Crossref] [PubMed]
- Ghoneim IA, Miocinovic R, Stephenson AJ, et al. Neoadjuvant systemic therapy or early cystectomy? Single-center analysis of outcomes after therapy for patients with clinically localized micropapillary urothelial carcinoma of the bladder. Urology 2011;77:867-70. [Crossref] [PubMed]
- Jackson BL, Mohammed A, Mayer N, et al. Is Immediate radical cystectomy necessary for all patients with non-muscle-invasive micropapillary bladder cancer? Urol Int 2016;96:32-8. [Crossref] [PubMed]
- Meeks JJ, Taylor JM, Matsushita K, et al. Pathological response to neoadjuvant chemotherapy for muscle-invasive micropapillary bladder cancer. BJU Int 2013;111:E325-30. [Crossref] [PubMed]
- Masson-Lecomte A, Xylinas E, Bouquot M, et al. Oncological outcomes of advanced muscle-invasive bladder cancer with a micropapillary variant after radical cystectomy and adjuvant platinum-based chemotherapy. World J Urol 2015;33:1087-93. [Crossref] [PubMed]


