
Comparison of effectiveness and postoperative complications of different surgical methods in the treatment of benign prostatic hyperplasia: a systematic review and meta-analysis based on randomized controlled trials
Introduction
In men, lower urinary tract symptoms (LUTS) caused by benign prostatic hyperplasia (BPH) are prevalent urinary diseases. It is estimated that the quality of life (QoL) of about 1 in every 3 men over 50 years old is affected by LUTS caused by BPH (1,2). Even BPH with moderate and severe symptoms can even affect the mental state of patients (3,4). Although drug treatment, such as finasteride and dutasteride, can control clinical symptoms to a certain extent, surgical treatment is still the most effective way to treat BPH. Among the surgical options, transurethral prostatectomy (TURP), which involves removing the hyperplastic prostate piece by piece through a unilateral electrode, has been the most widely used in the clinic since 1970. The long-term effectiveness of this procedure in improving a series of clinical indicators of BPH [such as maximum urinary flow rate (Qmax), international prostate symptom score (IPSS), QoL score, and so on] has been explored in many observational studies and randomized controlled trials (RCTs) (5-8). However, complications such as massive hemorrhage or TURP syndrome are also common (9). A study showed that TURP was associated with incidence rate and even mortality of complications (10). Since entering the new century, studies have explored the effectiveness and safety of new surgical methods for the treatment of BPH, such as the use of bilateral electrodes or various laser systems (holmium laser, potassium titanium phosphate laser, thulium laser, diode laser, and so on), prostatic artery embolization (PAE), plasmakinetic resection of the prostate (PKRP), transurethral GreenLightTM laser photovaporization of the prostate (GLL PVP), and so on. These new procedures are safer than traditional TURP procedures, with less risk of surgical bleeding, transprostatectomy syndrome, and decreased hemoglobin levels. Overall, all procedures can be divided into four categories: resection, vaporization, enucleation, and arterial embolization. Resection is the process of cutting out the enlarged prostate tissue piece by piece. Vaporization is the process of using electrodes such as lasers or plasma to vaporize prostate tissue to high temperatures. Enucleation is the process of removing the entire prostate tissue from the internal capsule. Arterial embolization, on the other hand, is a procedure in which the blood supply to the prostate is blocked by direct injection of small particles. Resection usually requires the most prostate tissue to be removed, whereas vaporization usually removes less tissue due to the risk of damaging the sphincter (11).
More and more clinical RCTs are exploring the efficacy and safety of new BPH surgery. However, there are conflicting conclusions about the relative efficacy of different surgical procedures and the corresponding clinical endpoints in the existing evidence. Specifically, Zhang et al. (12) and Xu et al. (13) compared diode laser enucleation with plasma endoprostate enucleation in a RCT and found that the former can significantly reduce the International Prostate Symptom Score (IPSS) compared with the latter. Wu et al. (14) came to the opposite conclusion. Similar contradictory conclusions between the various surgical procedures can also be found in many other RCTs (15-20). This is partly because most RCTs have very limited sample sizes, short follow-up, and are mostly single-center studies. So the results are not necessarily general. Systematic reviews and meta-analysis methods can generate more reliable evidence-based medical evidence by combining the results of as many studies as possible. Therefore, this study systematically quantified the relative efficacy and safety of various surgical procedures by systematically searching relevant literature. We present the following article in accordance with the PRISMA reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-22-377/rc).
Methods
Literature search
This study mainly searched the databases of PubMed, Ovid, Embase, ScienceDirect China National Knowledge Infrastructure Project and Wanfang database for clinical RCTs comparing the international prostate score, length of hospital stay, maximum urinary flow rate, operation time, and complication rates (outcome) of PAE, GLL PVP, diode laser enucleation of prostate (DILEP) (Intervention) and PKRP, TURP (Comparison) in patients with BPH (Population). The search terms “prostate hyperplasia”, “prostate hypertrophy”, “prostate tumor”, “TURP”, “enucleation vaporization diode laser”, “greenlight laser”, “prostate artery embolization”, and “plasma kinetics” were systematically searched in the databases in a reasonable combination. Endnote X9 (Clarivate, London, UK) was used for document management, and the documents that met the inclusion criteria were screened one by one.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (I) the type of literature design was a clinical RCT; (II) the interventions studied were PAE, GLL PVP, DILEP. PKRP, TURP in patients with BPH were the control group; (III) the primary endpoints studied included functional indicators such as IPSS, IPSS QoL, Qmax, prostate size, operation time, hospital stay, complication rate, and other indicators; and (IV) the standard deviation of the studied indicators was either provided in the literature or it could be calculated.
The exclusion criteria were as follows: (I) observational studies, reviews, academic conferences, reviews, and case reports; (II) the study population was a special subgroup of BPH rather than the general population (e.g., only patients with a prostate larger than a specific diameter or patients with other diseases); (III) Gray literature or withdrawn articles; and (IV) original data were not provided in the appendix materials. A total of 14 clinical RCTs were included in this study for meta-analysis.
Document sorting and evaluation
In this study, two independent researchers screened the literature and extracted the following data from the included literature: the author and the time of the study, the operation method of the intervention and control group, the sample size of the experimental group and the control group, the main indicators, the IPSS, the QoL indicator IPSS QoL, the Qmax, the post-void residual volume (PVR), the size of the prostate, the level of serum prostate-specific antigen (PSA), and the incidence of postoperative complications, operation duration, hospital stay, and so on. This study used the Cochrane Risk of Bias tool for systematic reviews and meta-analyses of RCTs. Two investigators independently assessed risk of bias for each included study based on seven aspects (21): (I) method of random number generation (selection bias); (II) group concealment (selection bias); (III) blinding of investigators and subjects (implementation bias); (IV) blinding (detection bias) to the primary endpoint measure; (V) integrity of research results and data; (VI) selective reporting; (VII) other biases. The evaluation criteria are as follows: (I) if the evaluation criteria are met, the risk of bias is low; (II) a risk of bias was considered possible if one or more of the criteria were only partially met or were less accurate; (III) a high risk of bias was considered to exist if one or more of the criteria were not met or not reported.
Statistical methods
All data analysis in this study were statistically analyzed by Stata SE 17.0 software (Stata Corp., College Station, TX, USA). Since the main clinical indicators observed in this study were continuous variables, they were expressed in the form of mean ± standard deviation. The incidence of complications was the measurement data, the statistics were expressed in percentage, and the effective value was expressed in a 95% confidence interval (CI). The Cochrane Q test evaluated the heterogeneity between studies, and I2 statistic was calculated to quantify the heterogeneity between studies. When the statistic I2 corrected by degrees of freedom was ≥50%, the random-effects model of the limited maximum likelihood probability method was used to merge the mean difference. Otherwise, the fixed-effects model of the reverse variance method was used to merge the effect values, and the chi-square test evaluated the intergroup difference in complication rate. Heterogeneity between studies was assessed using the Cochrane Q test and the I2 statistic. Meta-analyses with 5 or more included studies were evaluated for publication bias by funnel plot description and using Egger’s and Begg’s tests (22,23). All statistical results of this study were statistically significant, with P≤0.05, and the hypothesis tests were two-sided.
Results
Search results
Using the combination of medical subject words (MeSH) to systematically search in PubMed, Ovid, Embase, ScienceDirect, and other medical databases, 434 relevant literatures were retrieved. With reference to the established literature inclusion criteria, a total of 14 articles were finally included in the meta-analysis. The detailed literature retrieval and screening process are shown in the PRISMA flow chart, as shown in Figure 1. The included articles were 14 clinical RCTs. A total of 1,940 patients were divided into three groups to compare the effectiveness and safety of the different surgical procedures. Namely, the comparison of GLL PVP and TURP, the comparison of PAE and TURP, and the comparison of DILEP and PKRP, with 7, 4, and 3 articles included in each group, respectively. The basic information of the included articles is shown in Table 1. The Cochrane system evaluation system assessed the bias risk of the included literature. As shown in Table 2, there was a possible selection bias in the random number generation method in the 5 literatures. There may be a hidden selection bias in the 6 literatures. There was obvious selection bias with hidden grouping in 3 literatures. There was obvious bias in the blinding of investigators and subjects in 4 studies. Five studies had possible biases in blinding investigators and subjects. Seven studies had possible outcome measurement bias. One article had significant outcome measurement bias. There are possible biases in the research results and data integrity of the three literatures. Four studies were subject to selective reporting bias. There were possible other biases in 8 studies.
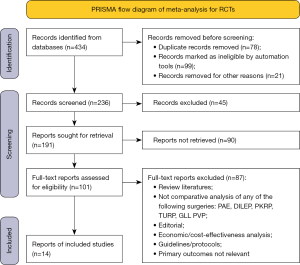
Table 1
| Author | Intervention/control | Sample size in each group |
Age (years), mean ± SD | IPSS, mean ± SD | IPSS QoL, mean ± SD | IIEF-S, mean ± SD | Qmax, mean ± SD | Post-void residual, mean ± SD | Prostate volume, mean ± SD | PSA, mean ± SD | Complication events | Operative time (minutes), mean ± SD | Hospital stays (days), mean ± SD | Quality score of NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. [2019] (12) | DILEP/ | 79/ | 73.7±8.4/ | 24.5±3.2/ | 4.7±0.7/ | N/a | N/a | 204.6±191.1/ | 56.2±11.9/ | N/a | 30.3% (2376)/ | 61.3±19.0/ | 7.9±1.1/ | 7 |
| PKRP | 78 | 71.5±8.9 | 25.3±3.0 | 4.9±0.7 | 199.5±186.8 | 55.5±13.1 | 21.1% (1676) | 94.5±31.5 | 9.5±1.1 | |||||
| Xu et al. [2013] (13) | DILEP/ | 40/ | N/A | 4.88±1.24/ | 1.18±0.45/ | N/a | 23.45±3.33/ | 1.25±3.10/ | 27.4±5.54/ | 1.14±0.28/ | 25.0%/ | 33.73±6.96/ | 4.95±0.95/ | 6 |
| PKRP | 40 | 5.28±1.32 | 1.23±0.48 | 23.32±3.67 | 2.15±5.02 | 26.1±5.12 | 1.05±0.26 | 47.5% | 50.28±6.24 | 5.30±0.93 | ||||
| Wu et al. [2016] (14) | DILEP/ | 40/ | 75.4±8.4/ | 22.4±5.3/ | N/a | 17.1±2.7/ | 6.8±2.8/ | 163.8±41.7/ | 98.6±21.6/ | 5.6±3.2/ | 50.0%/ | 113.5±25.4/ | 3.6±1.5/ | 7 |
| PKRP | 40 | 73.6±6.2 | 21.8±4.5 | 17.5±2.6 | 7.6±3.1 | 147.5±47.2 | 93.3±18.5 | 6.2±3.8 | 82.5% | 98.7±31.5 | 4.8±1.8 | |||
| Al-Ansari et al. [2010] (24) | GLL PVP/ | 60/ | 66.3±9.4/ | 27.2±2.3/ | N/a | N/a | 6.9±2.2/ | 53.2±25/ | 61.8±22/ | N/a | 0%/ | 89±18/ | 2.3±1.2/ | 8 |
| TURP | 60 | 67.1±8 | 27.9±2.7 | 6.4±2 | 57±21 | 60.3±20 | 16.7% | 80±13 | 1.4±0.6 | |||||
| Bachmann et al. [2014] (25) | GLL PVP/ | 136/ | 65.9±6.8/ | 21.2±5.9/ | 4.6±1.1/ | N/a | 9.5±3.0/ | 110.1±88.5/ | 48.6±19.2/ | N/a | 12.7%/ | N/a | 2.6±1.3/ | 8 |
| TURP | 133 | 65.4±6.6 | 21.7±6.4 | 4.5±0.9 | 9.9±3.5 | 109.8±103.9 | 46.2±19.1 | 16.8% | 4.1±2.1 | |||||
| Capitán et al. [2011] (16) | GLL PVP/ | 50/ | 69.8±8.44/ | 23.74±5.242/ | 4.52±0.27/ | N/a | 8.03±3.14/ | N/a | 51.29±14.72/ | 2.13±1.21/ | 14%/ | N/a | 1.6±1.2/ | 7 |
| TURP | 50 | 67.7±6.7 | 3.52±4.38 | 4.14±1.06 | 3.88±2.71 | 53.10±13.75 | 1.79±1.15 | 32% | 3.6±2.1 | |||||
| Elshal et al. [2020] (15) | GLL PVP/ | 60/ | 64.5±6/ | 4.9±1.3/ | 1.23±0.99/ | 21.1±2.3/ | 25.5±3.12/ | 35.5±4.1/ | N/a | N/a | 26.5%/ | 92±32/ | N/a | 8 |
| TURP | 62 | 66.1±7 | 6.1±2.1 | 1.36±1.1 | 20.4±2.4 | 22.1±3.66 | 16.3±5.4 | 27.5% | 83±28 | |||||
| Lukacs et al. [2012] (26) | GLL PVP/ | 69/ | 66.9±7.8/ | 22±2.1/ | N/a | N/a | 7.79±2.75/ | 89.5±2.3/ | 50.54±16.53/ | N/a | 26.5%/ | N/a | N/a | 6 |
| TURP | 70 | 67.6±7.6 | 20±3.2 | 7.76±2.64 | 75±3.1 | 50.11±14.73 | 39.7% | |||||||
| Telli et al. [2015] (17) | GLL PVP/ | 39/ | 67 [51–87]/ | 20±3.1/ | N/a | N/a | 10.6±3.1/ | 60±5.3/ | 60±3.4/ | N/a | 39.4%/ | N/a | 2±1.1/ | 8 |
| TURP | 62 | 69 [56–87] | 19±4.2 | 12.5±2.2 | 65±6.2 | 55±4.1 | 32.1% | 5±2.5 | ||||||
| Thomas et al. [2016] (18) | GLL PVP/ | 139/ | 63.1±7.3/ | 6.9±6.0/ | 1.3±1.2/ | 12.9±7.5/ | 21.6±10.7/ | 45.6±65.5/ | 23.9±13.0/ | 1.4±1.7/ | 16.4%/ | N/a | N/a | 7 |
| TURP | 142 | 66.2±8.1 | 5.9±6.1 | 1.2±1.3 | 13.9±8.2 | 22.9±9.3 | 34.9±47.1 | 22.4±13.3 | 1.1±0.9 | 21.1% | ||||
| Carnevale et al. [2016] (27) | PAE/ | 15/ | 63.5±8.7/ | 12.8±8.0/ | 2.2±1.2/ | 12.6±7.7/ | 10.1±6.5/ | 62.3±71.0/ | 50.9±19.0/ | 2.2±1.1/ | N/a | N/a | N/a | 6 |
| TURP | 15 | 66.4±5.6 | 6.1±8.6 | 0.9±1.4 | 16.1±5.7 | 27.1±8.7 | 8.3±11.9 | 32.0±11.4 | 1.6±0.9 | |||||
| Abt et al. [2018] (20) | PAE/ | 48/ | 65.7±9.3/ | 10.15±4.1/ | 1.67±2.11/ | 14.64±5.31/ | 13.00±2.32/ | 70.3±7.86/ | 40.67±8.23/ | 2.3±1.7/ | N/a | N/a | 2.2±0.6/ | 7 |
| TURP | 51 | 66.1±9.8 | 6.82±5.5 | 1.55±3.21 | 11.67±4.13 | 22.52±6.55 | 33.7±8.23 | 27.16±6.44 | 1.33±1.12 | 4.2±1.7 | ||||
| Insausti et al. [2020] (8) | PAE/ | 23/ | 75.53±4.74/ | 5.6±3.5/ | 0.7±0.7/ | 15.7±7.2/ | 13.8±4.2/ | 13.1±5.6/ | 39.5±7.5/ | N/a | N/a | 90±35/ | N/a | 6 |
| TURP | 22 | 73.35±4.75 | 8.8±4.5 | 1.64±0.6 | 13.8±6.8 | 16.7±3.7 | 15.0±7.7 | 18.2±4.6 | 112±21 | |||||
| Pisco et al. [2020] (28) | PAE/ | 40/ | 66±7.4/ | 25.5±3.1/ | 4±2.3/ | 52.5±5.6/ | 7.9±7.5/ | 119.6±44.3/ | 68.5±43.1/ | N/a | 18.6%/ | N/a | 0.2±1.2/ | 7 |
| TURP | 40 | 70±7.5 | 27.5±4.5 | 4.5±2.1 | 46±6.6 | 7.3±5.4 | 106±33.2 | 65.5±32.3 | 63.9% | 1.2±2.2 |
PAE, prostatic artery embolization; GLL PVP, GreenLightTM laser photovaporization of the prostate; PKRP, plasmakinetic resection of the prostate; TURP, transurethral prostatectomy; DILEP, diode laser enucleation of prostate; PSA, prostate specific antigen; IPSS, international prostate symptom score; QoL, quality of life; IIEF-S, international erectile function index; Qmax, maximum urinary flow rate; SD, standard deviation; N/a, not available.
Table 2
| Author | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Zhang et al. [2019] (12) | Low | Low | Low | Low | Low | Low | Low |
| Xu et al. [2013] (13) | Unclear | Unclear | High | Unclear | Low | Unclear | Unclear |
| Wu et al. [2016] (14) | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| Al-Ansari et al. [2010] (24) | Low | High | High | Low | Low | Low | Low |
| Elshal et al. [2020] (15) | Low | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Capitán et al. [2011] (16) | Unclear | Unclear | Low | Unclear | Unclear | Unclear | Unclear |
| Bachmann et al. [2014] (25) | Low | High | Unclear | Unclear | Low | Low | Unclear |
| Lukacs et al. [2012] (26) | Unclear | Unclear | Unclear | Low | Unclear | Low | Low |
| Telli et al. [2015] (17) | Low | Low | Unclear | Low | Low | Unclear | Low |
| Thomas et al. [2016] (18) | Unclear | Low | High | Unclear | Unclear | Low | Unclear |
| Carnevale et al. [2016] (27) | Low | High | Unclear | High | Low | Low | High |
| Abt et al. [2018] (20) | Low | Unclear | High | Unclear | Low | Unclear | Unclear |
| Insausti et al. [2020] (8) | Low | Low | Low | Unclear | Low | Low | Unclear |
| Pisco et al. [2020] (28) | Low | Low | Low | Low | Low | Low | Low |
Comparison between the experimental group of DILEP and the control group of PKRP
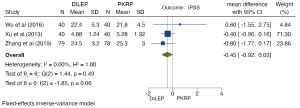
IPSS comparison
A total of 317 patients in three studies were included in this analysis. The heterogeneity test results were H2=1.00, I2=0.00%, and P=0.49, indicating that there was no heterogeneity in the three studies. The fixed-effects model based on reverse variance was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) of IPSS score between the DILEP group and PKRP group was −0.45 (−0.92 to 0.03), and the difference was not statistically significant, indicating that there was no statistically significant difference between the two methods in improving IPSS score, Q=1.44, P=0.06 (Figure 2).
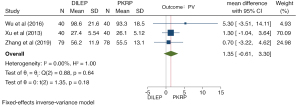
Comparison of postoperative prostate volume (PV)
A total of 317 patients in three studies were included in this analysis. The heterogeneity test results were H2=1.00, I2=0.00%, P=0.64, indicating that there was no heterogeneity in the three studies. The fixed-effects model based on reverse variance was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) in postoperative PV between DILEP group and the PKRP group was 1.35 (−0.61 to 3.30). The difference was not statistically significant, indicating that there was no statistically significant difference between the two methods in the change of postoperative PV, Q=0.88, P=0.18 (Figure 3).
Comparison of PVR
A total of 317 patients in three studies were included in this analysis. The heterogeneity test results were H2=1.50, I2=33.22%, P=0.22, indicating that there was no heterogeneity in the three studies. The fixed-effects model based on reverse variance was used to combine the mean difference. The results of meta-analysis showed that the mean difference (95% CI) of PVR between the DILEP group and PKRP group was −0.74 (−2.56 to 1.07), and there was no significant difference, indicating that there was no significant difference in the effectiveness of the two methods in improving the PVR, Q=2.99, P=0.42 (Figure 4).

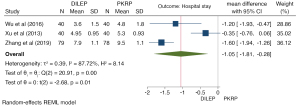
Comparison of hospital stay between DILEP and PKRP
A total of 317 patients in three studies were included in this analysis, and the heterogeneity test result was H2=8.14, I2=87.72%, P=0.00, indicating that there was heterogeneity in the three studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The meta-analysis results showed that the mean difference (95% CI) in hospital stay between the DILEP group and PKRP group was −1.05 (−1.81 to −0.28), which was statistically significant. It showed that DILEP could shorten the hospital stay by about 1 day compared with PKRP, and the difference was statistically significant, Q=20.91, P=0.01 (Figure 5).
Comparison between GLL PVP and TURP
IPSS comparison
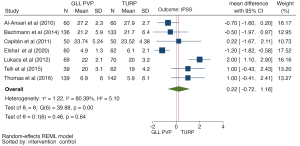
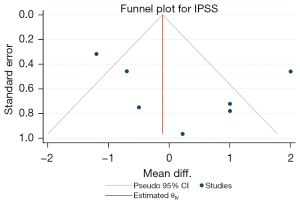
A total of 1,132 patients in 7 studies were included in this analysis. The heterogeneity test results were H2=5.10, I2=80.39%, P=0.00, indicating that there was heterogeneity in the 7 studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) in IPSS score between the GLL PVP group and the TURP group was 0.22 (−0.72 to 1.16), and the difference was not statistically significant, indicating that there was no statistically significant difference between the two methods in improving IPSS score, t=0.46, P=0.64 (Figures 6,7).
Comparison of postoperative QoL IPSS QoL
A total of 632 patients in four studies were included in this analysis. The heterogeneity test results were H2=1.53, I2=34.75%, P=0.20, indicating that there was no heterogeneity in the four studies. The fixed-effects model based on reverse variance was used to combine the mean difference. The results of the meta-analysis showed that the mean difference (95% CI) of IPSS QoL score between the GLL PVP group and the TURP group was 0.13 (−0.02 to 0.27), which was not statistically significant, indicating that there was no statistically significant difference in the effectiveness of the two methods in improving postoperative QoL, IPSS QoL, t=1.74, P=0.08 (Figure 8).

Comparison of postoperative maximum urinary flow rate Qmax
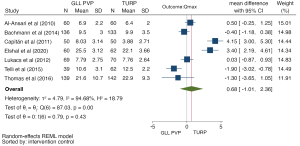
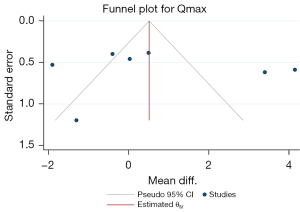
A total of 1,132 patients in 7 studies were included in this analysis. The heterogeneity test results were H2=18.79, I2=94.68%, P=0.00, indicating that there was heterogeneity in the 7 studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of meta-analysis showed that the mean difference (95% CI) of postoperative Qmax between the GLL PVP group and the TURP group was 0.68 (−1.01 to 2.36), which was not statistically significant, indicating that there was no statistically significant difference in the effectiveness of the two methods in improving postoperative Qmax, t=0.79, P=0.43 (Figures 9,10).
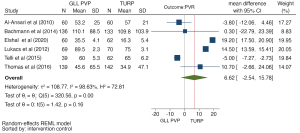
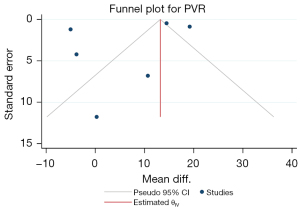
Comparison of PVR
A total of 832 patients from 6 studies were included in this analysis. The heterogeneity test results were H2=72.38, I2=98.63%, P=0.00, indicating that there was heterogeneity in the 7 studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) of PVR between the GLL PVP group and the TURP group was 6.62 (−2.54 to 15.78). The difference was not statistically significant, indicating that there was no statistically significant difference in the effectiveness of the two methods for improving PVR, t=1.42, P=0.16 (Figures 11,12).
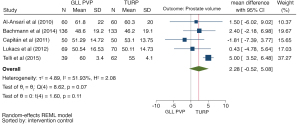
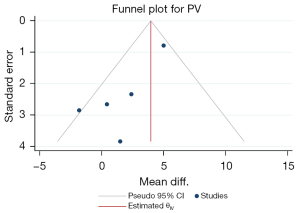
Comparison of postoperative PV
A total of 742 patients in five studies were included in this analysis. The heterogeneity test results were H2=2.08, I2=51.93%, P=0.07, indicating that there was heterogeneity in the five studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) of postoperative PV between the GLL PVP group and the TURP group was 2.28 (−0.52 to 5.08), which was not statistically significant, indicating that there was no statistically significant difference in the effectiveness of the two methods in improving IPSS score, t=1.60, P=0.11 (Figures 13,14).
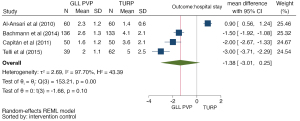
Comparison of hospital stay between GLL PVP and TURP
A total of 632 patients in four studies were included in this analysis. The heterogeneity test results were H2=43.39, I2=97.70%, P=0.00, indicating that there was heterogeneity in the four studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) in hospitalization time between the GLL PVP group and the TURP group was −1.38 (−3.01 to 0.25), and the difference was not statistically significant, indicating that the difference in hospitalization time between the two methods was not statistically significant, t=−1.66, P=0.10 (Figure 15).
Comparison of PAE and TURP
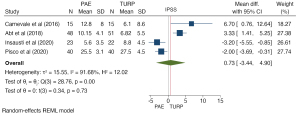
IPSS comparison
A total of 254 patients in four studies were included in this analysis. The heterogeneity test results were H2=12.02, I2=91.68%, P=0.00, indicating that there was heterogeneity in the four studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) in IPSS score between the PAE group and the TURP group was 0.73 (−3.44 to 4.90). The difference was not statistically significant, indicating that PAE can improve IPSS score by about 0.73 points compared with TURP, t=0.34, P=0.73 (Figure 16).
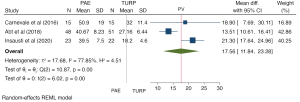
Comparison of postoperative PV
A total of 174 patients in three studies were included in this analysis. The heterogeneity test results were H2=4.51, I2=77.85%, P=0.00, indicating that there was heterogeneity in the four studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) in postoperative PV between the PAE group and the TURP group was 17.56 (11.84 to 23.28). The difference was statistically significant, indicating that the diameter of the prostate after PAE was about 17.56 mm compared with that after TURP. The difference was statistically significant, t=6.02, P=0.00 (Figure 17).
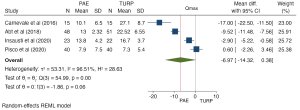
Comparison of postoperative Qmax
A total of 254 patients in 4 studies were included in this analysis. The heterogeneity test results were H2=28.63, I2=96.51%, P=0.00, indicating that there was heterogeneity in the 4 studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) of postoperative Qmax between the PAE group and the TURP group was −6.97 (−14.32 to 0.38), which was statistically significant, indicating that there was a statistically significant difference in the effectiveness of the two methods in improving postoperative maximum urinary flow rate Qmax, t=−1.86, P=0.06 (Figure 18).
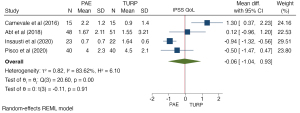
Comparison of postoperative QoL IPSS QoL
A total of 254 patients in four studies were included in this analysis. The heterogeneity test results were H2=6.10, I2=83.62%, P=0.00, indicating that there was heterogeneity in the four studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) in IPSS QoL score between the PAE group and the TURP group was −0.06 (−1.04 to 0.93). The difference was statistically significant. Compared with traditional TURP, PAE was shown to improve the QoL score of patients by about 0.06, t=−0.11, P=0.91 (Figure 19).
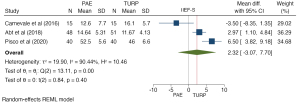
Comparison of PVR
A total of 209 patients in three studies were included in this analysis. The heterogeneity test results were H2=4.36, I2=77.06%, P=0.02, indicating that there was heterogeneity in the three studies. The random-effects model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the meta-analysis showed that the mean difference (95% CI) of PVR between the PAE group and the TURP group was 31.53 (11.62 to 51.43). The difference was statistically significant, indicating that the improvement of the urinary excretion control residue index by PAE was not as effective as traditional TURP, t=3.10, P=0.00 (Figure 20).
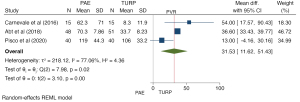
Comparison of international erectile function index
A total of 209 patients in three studies were included in this study. The heterogeneity test results were H2=10.46, I2=90.44%, P=0.00, indicating that there was heterogeneity in the three studies. The random effect model based on the restricted maximum likelihood probability method was used to combine mean difference. The results of the Meta-analysis showed that the mean difference (95% CI) between the PAE group and the TURP on international erectile function index (IIEF-S) was 2.32 (−3.07 to 7.70), and there was no significant difference, indicating that there was no significant difference in the effectiveness of the two methods for the improvement of international erectile function index IIEF-S, t=0.84, P=0.40 (Figure 21).
Discussion
The procedure of TURP remains the gold standard for treating BPH with a PV of 30–80 mL (15). Although TURP is more satisfactory than other minimally invasive surgical methods, such as laser vaporization and prostate kernel dissection, and postoperative patient subjective functional indicators such as IPSS, QoL, and IIEF-S, TURP is associated with a significant increase in the incidence of postoperative complications, reoperation rate, and perioperative mortality in patients with a large volume of BPH (>80 mL). Most of them are caused by massive postoperative bleeding (29). More importantly, postoperative complications are higher in patients with long-term use of anticoagulants and PV greater than 80 mL. Therefore, urologists have been trying to find a new minimally invasive endoscopic therapy for BPH. These new methods can be divided into three categories according to their respective treatment principles: resection (piece by piece resection of prostate tissue), vaporization (vaporization of prostate tissue using electrode or laser), and prostate core stripping (stripping large prostate from prostate capsule) including the use of bipolar energy and various laser systems, such as holmium laser, potassium titanium phosphate laser, thulium laser, and diode laser.
The prostate core stripping method uses laser or double electrodes to imitate the traditional prostatectomy. Therefore, some studies have found that the core stripping method usually has better postoperative functional indexes than the resection method and vaporization method, such as Qmax, IPSS, QoL, and so on, because the core stripping method can remove more prostate tissue compared with the other two methods, resulting in a significant reduction in the level of serum PSA (30), Although our results are inconsistent with this, considering that most of the people in the literature comparing vaporization and traditional resection in this study are people with PV greater than 80 mL, which itself has a less favorable postoperative prognosis and the incidence of complications, we speculate that the reason for this result is selection bias. However, this study found that the kernel stripping method can effectively shorten the hospital stay by 1.05 days (−1.81 to −0.28 days), and the difference is statistically significant, which is consistent with other previous studies. In addition, this study found that vaporization has lower postoperative functional improvement than traditional TURP, which is consistent with other previous studies (31).
There were some limitations to this study. We only compared the effectiveness and safety of three different surgical methods for BPH. Due to the research characteristics of systematic review and meta-analysis, we could only follow the grouping method of the experimental group and control group in the original contribution and could not cross-compare the effectiveness and safety of more surgical methods. Secondly, due to the different follow-up times between different studies, the measured postoperative functional indexes were not necessarily homogeneous, which may explain the high heterogeneity of some of our models. In addition, this study did not evaluate more novel surgical methods, such as robot-assisted prostatectomy.
Acknowledgments
Funding: The project was supported by Hainan Province Clinical Medical Center.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-22-377/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-377/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lerner LB, McVary KT, Barry MJ, et al. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA GUIDELINE PART I-Initial Work-up and Medical Management. J Urol 2021;206:806-17. [Crossref] [PubMed]
- La Vignera S, Aversa A, Cannarella R, et al. Pharmacological treatment of lower urinary tract symptoms in benign prostatic hyperplasia: consequences on sexual function and possible endocrine effects. Expert Opin Pharmacother 2021;22:179-89. [Crossref] [PubMed]
- Calogero AE, Burgio G, Condorelli RA, et al. Epidemiology and risk factors of lower urinary tract symptoms/benign prostatic hyperplasia and erectile dysfunction. Aging Male 2019;22:12-9. [Crossref] [PubMed]
- Pinto JD, He HG, Chan SW, et al. Health-related quality of life and psychological well-being in patients with benign prostatic hyperplasia. J Clin Nurs 2015;24:511-22. [Crossref] [PubMed]
- Muir G, Klecka J, Culkin DJ, et al. Comparison of GreenLight laser and transurethral resection of the prostate baseline characteristics and outcomes: lessons learned from the Clinical Research Office of the Endourological Society GreenLight Laser Study. Minerva Urol Nefrol 2017;69:285-92. [PubMed]
- Richard C, Robert G, Pradère B, et al. Cost analysis of GreenLight photoselective vaporization of the prostate versus standard transurethral resection of the prostate: Benefit of ambulatory care. Prog Urol 2021;31:275-81. [Crossref] [PubMed]
- Schelin S, Geertsen U, Walter S, et al. Feedback microwave thermotherapy versus TURP/prostate enucleation surgery in patients with benign prostatic hyperplasia and persistent urinary retention: a prospective, randomized, controlled, multicenter study. Urology 2006;68:795-9. [Crossref] [PubMed]
- Insausti I, Sáez de Ocáriz A, Galbete A, et al. Randomized Comparison of Prostatic Artery Embolization versus Transurethral Resection of the Prostate for Treatment of Benign Prostatic Hyperplasia. J Vasc Interv Radiol 2020;31:882-90. [Crossref] [PubMed]
- Reich O, Gratzke C, Bachmann A, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 2008;180:246-9. [Crossref] [PubMed]
- Mitchell CR, Hendrick RJ, Webster RJ 3rd, et al. Toward Improving Transurethral Prostate Surgery: Development and Initial Experiments with a Prototype Concentric Tube Robotic Platform. J Endourol 2016;30:692-6. [Crossref] [PubMed]
- Gallucci M, Puppo P, Perachino M, et al. Transurethral electrovaporization of the prostate vs. transurethral resection. Results of a multicentric, randomized clinical study on 150 patients. Eur Urol 1998;33:359-64. [Crossref] [PubMed]
- Zhang J, Wang X, Zhang Y, et al. 1470 nm Diode Laser Enucleation vs Plasmakinetic Resection of the Prostate for Benign Prostatic Hyperplasia: A Randomized Study. J Endourol 2019;33:211-7. [Crossref] [PubMed]
- Xu A, Zou Y, Li B, et al. A randomized trial comparing diode laser enucleation of the prostate with plasmakinetic enucleation and resection of the prostate for the treatment of benign prostatic hyperplasia. J Endourol 2013;27:1254-60. [Crossref] [PubMed]
- Wu G, Hong Z, Li C, et al. A comparative study of diode laser and plasmakinetic in transurethral enucleation of the prostate for treating large volume benign prostatic hyperplasia: a randomized clinical trial with 12-month follow-up. Lasers Med Sci 2016;31:599-604. [Crossref] [PubMed]
- Elshal AM, Soltan M, El-Tabey NA, et al. Randomised trial of bipolar resection vs holmium laser enucleation vs Greenlight laser vapo-enucleation of the prostate for treatment of large benign prostate obstruction: 3-years outcomes. BJU Int 2020;126:731-8. [Crossref] [PubMed]
- Capitán C, Blázquez C, Martin MD, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: a randomized clinical trial with 2-year follow-up. Eur Urol 2011;60:734-9. [Crossref] [PubMed]
- Telli O, Okutucu TM, Suer E, et al. A prospective, randomized comparative study of monopolar transurethral resection of the prostate versus photoselective vaporization of the prostate with GreenLight 120-W laser, in prostates less than 80 cc. Ther Adv Urol 2015;7:3-8. [Crossref] [PubMed]
- Thomas JA, Tubaro A, Barber N, et al. A Multicenter Randomized Noninferiority Trial Comparing GreenLight-XPS Laser Vaporization of the Prostate and Transurethral Resection of the Prostate for the Treatment of Benign Prostatic Obstruction: Two-yr Outcomes of the GOLIATH Study. Eur Urol 2016;69:94-102. [Crossref] [PubMed]
- Ray AF, Powell J, Speakman MJ, et al. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int 2018;122:270-82. [Crossref] [PubMed]
- Abt D, Hechelhammer L, Müllhaupt G, et al. Comparison of prostatic artery embolisation (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: randomised, open label, non-inferiority trial. BMJ 2018;361:k2338. [Crossref] [PubMed]
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc 2018;16:195-203. [Crossref] [PubMed]
- Palma Pérez S, Delgado Rodríguez M. Practical considerations on detection of publication bias. Gac Sanit 2006;20:10-6. [PubMed]
- Al-Ansari A, Younes N, Sampige VP, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol 2010;58:349-55. [Crossref] [PubMed]
- Bachmann A, Tubaro A, Barber N, et al. 180-W XPS GreenLight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European Multicentre Randomised Trial--the GOLIATH study. Eur Urol 2014;65:931-42. [Crossref] [PubMed]
- Lukacs B, Loeffler J, Bruyère F, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol 2012;61:1165-73. [Crossref] [PubMed]
- Carnevale FC, Iscaife A, Yoshinaga EM, et al. Transurethral Resection of the Prostate (TURP) Versus Original and PErFecTED Prostate Artery Embolization (PAE) Due to Benign Prostatic Hyperplasia (BPH): Preliminary Results of a Single Center, Prospective, Urodynamic-Controlled Analysis. Cardiovasc Intervent Radiol 2016;39:44-52. [Crossref] [PubMed]
- Pisco JM, Bilhim T, Costa NV, et al. Randomised Clinical Trial of Prostatic Artery Embolisation Versus a Sham Procedure for Benign Prostatic Hyperplasia. Eur Urol 2020;77:354-62. [Crossref] [PubMed]
- Pirola GM, Castellani D, Lim EJ, et al. Urethral stricture following endoscopic prostate surgery: a systematic review and meta-analysis of prospective, randomized trials. World J Urol 2022;40:1391-411. [Crossref] [PubMed]
- Flanigan RC, Reda DJ, Wasson JH, et al. 5-year outcome of surgical resection and watchful waiting for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol 1998;160:12-6; discussion 16-7. [Crossref] [PubMed]
- Placer J, Gelabert-Mas A, Vallmanya F, et al. Holmium laser enucleation of prostate: outcome and complications of self-taught learning curve. Urology 2009;73:1042-8. [Crossref] [PubMed]
(English Language Editor: J. Jones)


