
Balloon dilation performs poorly as a salvage management strategy for recurrent bulbar urethral strictures following failed urethroplasty
IntroductionOther Section
Urethral dilation and direct visual internal urethrotomy (DVIU) have long been a part of the treatment armamentarium for urethral stricture disease (USD). The success rate for these procedures is highly dependent upon stricture length, location, and the degree of spongiofibrosis. The greatest endoscopic success has been observed with bulbar urethral strictures less than 1 cm in length (1-3). Overall long-term success rates for short bulbar strictures (<2 cm) have been reported to be 35–70% for both dilation and DVIU compared to 80–95% for urethroplasty (4-6). However, open reconstruction requires surgical expertise, general anesthesia with prolonged operative times, longer postoperative urethral catheterization, and higher risk of perioperative morbidity. For these reasons, the American Urological Association (AUA) 2016 Guideline on male USD states that surgeons may offer any of the above-stated techniques for the initial management of a short (<2 cm) bulbar urethral stricture (7).
The optimal management strategy for recurrent USD following urethroplasty remains undefined. Previous studies have established that repetitive endoscopic interventions in the absence of prior urethroplasty have failure rates exceeding 80% (8,9). Repetitive endoscopic treatment also places the patient at risk for development of longer, more complex strictures which would make a future open reconstruction more challenging (10). However, it is unclear if a less invasive treatment option would have similar failure rates or if it would be a viable solution in patients who have undergone complex open urethral reconstruction.
As a tertiary referral center, we frequently encounter patients who have failed initial USD management. After failed bulbar urethroplasty, we have observed that these secondary strictures are often soft and pliable, which may make them amenable to reconfiguration. In lieu of DVIU, which may be associated with an exacerbation in scar formation and stricture complexity, balloon dilation has been of particular interest to us as a minimally invasive treatment strategy. In select circumstances, we have reserved salvage urethral balloon dilation as an alternative to formal secondary urethroplasty. Herein, we aim to evaluate the role and efficacy of endoscopic urethral balloon dilation for recurrent USD after failed urethroplasty.
MethodsOther Section
In completing a retrospective review of our Institutional Review Board (IRB)-approved single-surgeon USD database, we identified patients who underwent balloon dilation procedures for bulbomembranous USD at our institution between 2007–2018. Patients who underwent a concomitant open or other endoscopic urethral procedure at the time of balloon dilation were excluded. Treatment failure was defined as the need for subsequent surgical intervention due to recurrent USD.
All balloon dilations were performed with an 8-cm, 24-French UroMax Ultra™ balloon dilator (Boston Scientific Corp.) over an Amplatz Super Stiff™ GuideWire (Boston Scientific Corp.). Each procedure was performed under direct vision, guided by a 16-French flexible cystoscope inserted alongside and parallel to the wire within the urethra. Direct visualization allowed for precise positioning of the balloon across the stricture and an atraumatic, controlled dilation. The balloon was left inflated for approximately 4 minutes at 20 atmospheres (ATM) of pressure. A 20 French Council tip catheter was placed over the wire to gravity drainage for 48 hours postoperatively.
Stricture characteristics including etiology, length, location, severity stage, and prior surgical procedures were compared between patients with and without balloon dilation treatment failure. Stricture staging was defined as previously described in the literature: stage 0 = no identifiable stricture, stage 1 = wide caliber stricture that easily allows scope passage, stage 2 = passable stricture but requires gentle dilation with a 16 French flexible cystoscope, stage 3 = impassable stricture with scope but lumen visible, and stage 4 = obliterative stricture with no visible lumen (11). Follow-up was defined as time from balloon dilation to most recent patient encounter as documented in the electronic medical record. Follow-up protocol for patients undergoing balloon dilation includes cystoscopy at three months, sooner if worse. Categorical variables were compared with the Fisher’s exact test. Continuous variables were compared with the Mann-Whitney U test. Parameters associated with treatment failure on univariate analysis were included in multivariable models of treatment failure. Specifically, overall history of prior treatment irrespective of type was evaluated. Italicized P values within the tables are <0.05 indicating that they are statistically significant.
ResultsOther Section
Patient characteristics
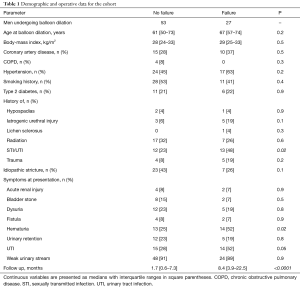
In total, 80 patients underwent balloon dilation procedures for bulbomembranous USD at our institution between 2007–2018. The cohort was divided into two groups: those who failed balloon dilation (27 patients) vs. those without failure (53 patients). There were no significant differences between the groups with regards to basic demographic characteristics including age, body mass index (BMI), and medical co-morbidities (Table 1). However, there was a significant difference in percentage of patients with hematuria (P<0.05). In addition, it was noted that the follow-up was significantly higher in the failure group than the no-failure group (P<0.0001). Overall complications of balloon dilation were uncommon (6/80, 7.5%) and tended to be minor in nature: urinary tract infection (1/80, 1.3%) and urinary retention (5/80, 6.3%) (Table 2).
Full table

Full table
Stricture characteristics and prior management
Stricture location, length, and stage were comparable between the two groups. The majority of USD in our cohort was located in the proximal bulbar urethra (48/80, 60%). Distal bulbar and membranous strictures accounted for 13.8% (11/80) and 26.3% (21/80), respectively (Table 2). Median stricture length was 1 cm. Almost three-quarters (59/80, 73.8%) of patients in our cohort had a severity stage 3 stricture. Over 75% of patients had some form of prior stricture treatment, including dilation (34/80, 42.5%), DVIU (19/80, 23.8%), or urethroplasty (48/80, 60%) (Table 2).
Balloon dilation outcomes
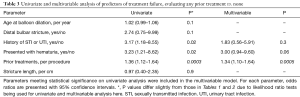
The overall success rate for balloon dilation of USD in our cohort was 66.3% (53/80). Failure rate of balloon dilation was higher in the group with prior treatment, namely prior dilations and prior urethroplasties (P<0.05). Failure cases were more likely to have strictures following urethroplasty (21/27, 78%) vs. 51% (27/53) in the no-failure group (P=0.03). Among the 27/80 (33.8%) failures, median time to recurrence was 4 months (IQR, 2–12 months). These patients had a greater incidence of prior stricture intervention (P=0.01) and number of prior interventions in general (P=0.0003). This group also had a greater incidence of prior urethroplasty specifically (P=0.04). On multivariable analysis, prior treatments were an independent risk factor for failure (P=0.0005) (Table 3). Overall, the failure rate of balloon dilation among those with prior urethroplasty is significantly greater than those without prior urethroplasty [21/48 (44%) vs. 6/32 (19%); P<0.05].
Full table
DiscussionOther Section
We found that endoscopic balloon dilation performed poorly as a salvage management strategy for recurrent USD in our cohort. In our cohort, the failure rates for balloon dilation of strictures following urethroplasty was more than two times higher relative to those with no prior urethroplasty. Our results confirm the finding of previous studies—repetitive endoscopic management for anterior USD has a high rate of treatment failure (8,9).
There are theoretical advantages to balloon dilation for the management of USD. This controlled dilation occurs by radial expansion which reduces shear trauma, bleeding, and may be better tolerated relative to sequential rigid dilation (12). It is a technically simple and efficient procedure, and has minimal recovery time. This enables it to easily be performed in the outpatient setting with a low incidence of complications. It can either be accomplished under direct vision or under fluoroscopic guidance with an “on-table” urethrogram (13-15). We chose to perform our dilations under direct vision, with the guidance of flexible urethroscopy, as we felt this gave us the best control and accuracy. Because of these advantages, many practicing urologists have adopted the concept of a “reconstructive surgical ladder”, which entails utilizing minimally invasive, endoscopic techniques before resorting to open reconstruction (16). This practice pattern is not supported by USD literature though and likely stems from inexperience with open reconstructive techniques.
It is well established that formal urethroplasty is the gold standard management strategy for USD and offers the greatest chance of cure. Repeat urethroplasties after a prior urethroplasty have shown comparable outcomes compared to patients who had only prior excisions (17). However, it requires surgical expertise, general anesthesia with prolonged operative times, longer postoperative urethral catheterization, higher risk of perioperative morbidity, and is the most invasive of the treatment options. After failed urethroplasty, all of these risks become even more apparent during salvage reconstruction compared to virgin cases. A short, simple endoscopic procedure can be an attractive management approach in this particular setting for patient and surgeon alike, especially in patients with multiple co-morbidities. Nonetheless, our data highlights the poor performance of balloon dilation as a salvage strategy and provides important prognostic information for reconstructive urologists and their patients for a fairly common clinical scenario. Balloon dilation will often only delay, but not obviate the need for salvage open reconstruction and should only be used in select situations when formal urethroplasty is not a feasible option.
Limitations
As with any clinical study, ours is not without limitations. This is a single center retrospective study. A median follow-up period of 8.4 months may be insufficient to capture all failures and relevant complications even with an early median time to failure seen in our cohort. Our small sample size prevents widespread assertions regarding the true effectiveness of balloon dilation in the salvage setting, and these results should be confirmed with future studies. Given the retrospective nature, there may be a selection bias on patient selection for electing balloon dilation versus a formal reconstruction. Factors unforeseen in a retrospective review may better be elucidated in a prospective study. The details of any prior urethroplasty procedures were outside the scope of this paper and unavailable for analysis. Further, whether any topical balloon coating may improve upon these results remains to be seen.
ConclusionsOther Section
Although balloon dilation is a minimally invasive endoscopic treatment strategy with many advantages, it performs poorly as a salvage strategy for recurrent urethral strictures after failed open urethral reconstruction. Balloon dilation should be utilized sparingly in this setting and reserved for those patients who are at a high surgical risk or unable to tolerate general anesthesia.
AcknowledgmentsOther Section
None.
FootnoteOther Section
Conflicts of Interest: Dr. AF Morey receives honoraria for being a guest lecturer/meeting participant for Boston Scientific and Coloplast Corp. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the UT Southwestern Institutional Review Board with ID# 032011-150. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ReferencesOther Section
- Hafez AT, El-Assmy A, Dawaba MS, et al. Long-term outcome of visual internal urethrotomy for the management of pediatric urethral strictures. J Urol 2005;173:595-7. [Crossref] [PubMed]
- Kumar S, Kapoor A, Ganesamoni R, et al. Efficacy of holmium laser urethrotomy in combination with intralesional triamcinolone in the treatment of anterior urethral stricture. Korean J Urol 2012;53:614-8. [Crossref] [PubMed]
- Zehri AA, Ather MH, Afshan Q. Predictors of recurrence of urethral stricture disease following optical urethrotomy. Int J Surg 2009;7:361-4. [Crossref] [PubMed]
- Steenkamp JW, Heyns CF, De Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: A prospective, randomized comparison. J Urol 1997;157:98-101. [Crossref] [PubMed]
- Heyns CF, Steenkamp JW, De Kock ML, et al. Treatment of male urethral strictures: Is repeated dilation or internal urethrotomy useful? J Urol 1998;160:356-8. [Crossref] [PubMed]
- Launonen E, Sairanen J, Ruutu M, et al. Role of visual internal urethrotomy in pediatric urethral strictures. J Pediatr Urol 2014;10:545-9. [Crossref] [PubMed]
- “Male Urethral Stricture”. American Urological Association Clinical Guidelines. Available online: http://www.auanet.org/guidelines/male-urethral-stricture-(2016)
- Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: Long-term followup. J Urol 1996;156:73-5. [Crossref] [PubMed]
- Jordan GH, Wessells H, Secrest C, et al. Effect of a temporary thermo-expandable stent on urethral patency after dilation or internal urethrotomy for recurrent bulbar urethral stricture: Results from a 1-year randomized trial. J Urol 2013;190:130-6. [Crossref] [PubMed]
- Hudak SJ, Atkinson TH, Morey AF. Repeat transurethral manipulation of bulbar urethral strictures is associated with increased stricture complexity and prolonged disease duration. J Urol 2012;187:1691-5. [Crossref] [PubMed]
- Purohit RS, Blaivas JG, Weinberger JM, et al. A New Staging System for Anterior Urethral Strictures. Urology Practice 2014;1:35-9. [Crossref]
- MacDiarmid SA, Harrigan CT, Cottone JL, et al. Assessment of a new transurethral balloon dilation catheter in the treatment of urethral stricture disease. Urology 2000;55:408-13. [Crossref] [PubMed]
- Vyas JB, Ganpule AP, Muthu V, et al. Balloon dilatation for male urethral strictures “revisited”. Urol Ann 2013;5:245-8. [Crossref] [PubMed]
- Chhabra JS, Balaji SS, Singh A, et al. Urethral Balloon Dilatation: Factors Affecting Outcomes. Urol Int 2016;96:427-31. [Crossref] [PubMed]
- Gelman J, Liss MA, Cinman NM. Direct vision balloon dilation for the management of urethral strictures. J Endourol 2011;25:1249-51. [Crossref] [PubMed]
- Bullock TL, Brandes SB. Adult anterior urethral strictures: a national practice patterns survey of board certified urologists in the United States. J Urol 2007;177:685-90. [Crossref] [PubMed]
- Siegel JA, Panda A, Tausch TJ, et al. Repeat Excision and Primary Anastomotic Urethroplasty for Salvage of Recurrent Bulbar Urethral Stricture. J Urol 2015;194:1316-22. [Crossref] [PubMed]


