
Biochemical evaluation of kidney disease
Introduction
Kidney disease is associated with substantial morbidity and mortality, emphasising the importance of diagnosis and monitoring. Establishing the presence of kidney disease can be difficult, due to the many aetiologies, and the assays’ ability to identify the disease at the earliest possible occurrence. The cause may be pre-renal, as seen with hypovolaemia; intrinsic renal disease, such as diabetic nephropathy; and post-renal, due to an obstruction, such as benign prostatic hyperplasia. To this end, many different biochemical markers exist, predominately in blood and urine, which can be used as markers of renal function or renal injury. Other markers may also be measured in kidney disease in order to assess the effect of kidney function on pathophysiological processes.
Some markers of renal function are used to determine glomerular filtration rate (GFR). Despite the kidney performing a wide array of functions, GFR is considered to be a robust indicator of renal function (1). It is defined as the volume of plasma that can be cleared of a particular analyte per unit time. The ideal marker of GFR is a substance that is endogenously produced by the body at a relatively fixed rate, freely filtered at the glomerulus, without being secreted or reabsorbed by the tubules, and does not undergo extrarenal elimination (2). For example, urea is seen as a poor marker of GFR, as it is produced at variable rates, undergoes marked reabsorption by the tubules, and its level is influenced by many other conditions, such as liver disease (3).
The kidneys are responsible for many roles essential to life, such as filtering the blood of metabolic wastes and toxins, endocrine functions, and maintaining the composition of the extracellular fluid (ECF). Assessing these functions individually can be difficult and expensive, so a versatile marker of kidney function is desirable. Creatinine is used to stage chronic kidney disease (CKD), along with urine albumin content if the abnormalities have persisted for longer than 3 months (4), and acute kidney injury (AKI) (5). Exogenous substances, such as inulin and radioisotopic markers, provide the most accurate estimation of GFR (6,7), but have a number of disadvantages; they are time consuming procedures, not routinely available, and possible radiation exposure (8). An endogenous marker that can circumvent these limitations is desirable.
Plasma biomarkers of renal function
These are markers that can be measured in a plasma (or serum) sample in order to give a numeric value that either directly indicates renal function, or can be inserted into a formula that estimates a parameter related to renal function, such as estimated GFR (eGFR).
Creatinine
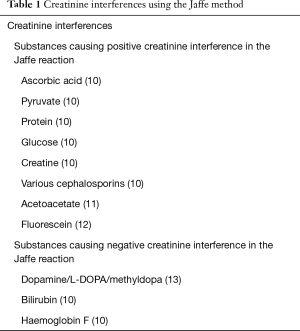
Creatinine is the most widely available and commonly used biomarker of renal function. It is derived from creatine, which is used in muscles as a quick-acting store of energy. Creatine undergoes spontaneous, irreversible conversion to its anhydride form, creatinine. While creatinine is freely filtered and minimally reabsorbed, 20–30% is also secreted by the proximal tubule (9), thus overestimating the creatinine and underestimating the eGFR, but this is somewhat offset in the Jaffe method by the non-creatinine chromogens (Table 1). In addition to these multiple methodological interferents, a further limitation of using creatinine to determine GFR is evidenced by the curvilinear relationship between creatinine and GFR, which makes it prone to not being able to detect mild to moderate reductions in GFR clearly (1)—if the reference interval of creatinine is 50–100 µmol/L, and a patient has an initial result of 50 µmol/L and follow-up result of 100 µmol/L, there GFR will have halved, despite their creatinine being within the reference interval. This emphasises two key points regarding creatinine—eGFR should be used where possible to track renal function (see formula section), and comparing a patient’s values to their previous values is more important than comparing a patient’s values to a reference interval.
Full table
The most widely used method to determine creatinine level is the Jaffe reaction and its variations (14), based on the detection of colour change when creatinine reacts with alkaline picrate. Whilst it is relatively inexpensive and the most widely used, it is liable to a number of common interferents, such as ketones (positive interferent) and bilirubin (negative interferent) (15), refer to Table 1. Furthermore, these interferents are often very difficult to remove without compromising the specimen. Analysing platforms used in the laboratory use aqueous calibrators that do not have consistent levels of these interfering chromogens in them, creating biases between laboratories and instruments of up to 20% (16).
Other methods used to determine creatinine concentration include the various enzymatic methods, and chromatographic methods. Enzymatic methods, typically used in point of care testing, are routinely more expensive, despite being less associated with interferents (although not immune) than the Jaffe method (17). They typically use hydrogen peroxide in their reactions, so may be liable to interference from an antioxidant, such as vitamin C. Chromatographic methods are more accurate than the Jaffe methods, but are not widely available, have a long turnaround time, and require specialised instrumentation and labour. The differences between methods and between calibrators, and patient samples (non-commutability) limits the transference of results between laboratories.
Cystatin C
Cystatin C is a marker of renal function that offers potential advantages over creatinine. It is a small protein (approximately 13 kDa) produced by all nucleated cells, so is less dependent on muscle mass, although it may be increased in hyperthyroidism, corticosteroid use, and rapid cell turnover (18,19). Cystatin C is typically measured using either a turbidimetric or nephelometric immunoassay technique. The method for cystatin C typically has less interferences associated with it, relative to the creatinine methods, but being an immunoassay, is still potentially liable to heterophilic antibodies (20). Nephelometric and turbidimetric techniques are also interfered by turbidity of the assay, such as in hypertriglyceridaemia (21). The method is automated, and although many times more expensive to run than creatinine, it is cheaper than other routinely available analytes, such as 25-hydroxyvitamin D or B-type natriuretic peptide (22). Cystatin C values between assays are not standardised, so values cannot be compared between methods (23). While studies are yet to conclusively demonstrate a clinical benefit with routine testing of cystatin C over creatinine, cystatin C may have clinical utility in certain clinical scenarios, such as patients with conditions affecting muscle mass, and in patients with eGFR values between 60–90 mL/min/1.73 m2 without albuminuria, in order to utilise it as a more sensitive marker for CKD. Due to its shorter half-life, serum levels of cystatin C also change more quickly than creatinine (24). Cystatin C is able to detect AKI earlier than creatinine in critically ill patients (25).
eGFR
eGFR can be calculated with the use of multiple formulas, all associated with their own potential setbacks. These typically use endogenous biomarkers, and adjust for certain patient variables such as weight (eGFR increases with weight if the creatinine of cystatin C levels remains constant), gender (men have a higher eGFR than women if the creatinine or cystatin C level is the same), age (eGFR decreases with age), and race (adjustments may be needed depending on race) (26). Since these formulas principally rely on creatinine or cystatin C, any potentially incorrect results will also produce errors in eGFR calculation. Historically, the Cockcroft-Gault equation was used to assess renal function, but its use has been limited these days to assisting with medication dosing initiation and adjustment (27,28). Its use has been superseded in the laboratory by equations derived from studies linking creatinine concentration, along with gender and age, to eGFR, corrected for body surface area. The Modification of Diet in Renal Disease formula (MDRD) was recommended for use in laboratories until 2012, when guidelines suggested switching to the CKD-EPI formula (29). The MDRD formula was derived from data using patients with established kidney disease, which was not applicable to patients with healthy kidney function, and as a result, underestimate eGFR in patients with a normal eGFR >90 mL/min/1.73 m2 (30). The CKD-EPI formula has found to be more accurate across the range of eGFR (28,30). Limitations of these formulas include that they can only be used in adults greater than 18 years old and racial differences may exist (29,31). The Schwarz formula is a potential eGFR calculator that can be used in a paediatric population, although care may be needed in its application to certain ethnic groups (31,32). Despite this, there are still potential limitations to the use of eGFR to assess renal function. Using eGFR equations can be problematic in AKI, as the equations assume a steady state of creatinine (23).
A number of other emerging serum and plasma markers may offer clinical value, such as beta-trace protein (prostaglandin D2 synthase) (33), symmetric dimethyl arginine (34), alpha-1-microglobulin (A1M) (35), and beta-2-microglobulin (36). Creatinine clearance, which requires a timed urine collection, urine creatinine and corresponding plasma creatinine, which is an inexpensive alternative to the eGFR, but has its own limitations, such as inconvenience for the patient with collection, and inaccuracies in the urine collection time (1).
Urinary biomarkers of kidney disease
Urinary biomarkers offer potential advantages over blood biomarkers due to the first manifestations of kidney injury appearing in the tubular cells, and subsequently the urine in the lumen (25). They are therefore more sensitive to changes in renal function, typically showing abnormal results within the first day of renal compromise.
Neutrophil gelatinase-associated lipocalin/lipocalin-2 (NGAL)
NGAL can be measured in both plasma and urine. The potential advantage of urine is that acute kidney damage results initially in the damage to renal tubules (25). This addresses one of the major limitations of serum creatinine, which does not increase to a level reflective of the renal impairment in the early stages (8). NGAL exists in many tissues, including the kidney. In animal models, it is upregulated by the kidney very early on after the onset of kidney injury (37). However, it is typically low in patients with stable CKD. Urinary NGAL exists in multiple forms, depending on whether it is released from tubule cells or neutrophils in the circulation. This contributes to the variation between different assays, as the different immunoassays use different antibodies to detect the NGAL. The monomeric form is released by the damaged renal tubules, while the dimeric form is the major form released by neutrophils. Hence, it is this monomeric form that correlates most closely with GFR (37). This requires specific immunoassays, as systemic release from neutrophils may cause increases in NGAL levels independently of kidney injury. In addition, leucocyturia also has the potential to cause significant elevations in urinary NGAL. Patients over 60 years of age have been found to have slightly higher urinary levels compared to younger patients, as have women compared to men, even when creatinine ratio is determined (38). This compromises the utility of plasma NGAL in detecting AKI in patients with severe sepsis. Various assays exist for the measurement of NGAL in urine and plasma, including chemiluminescent, particle enhanced turbidimetric, and enzyme linked immunosorbent assay (ELISA) methods (39).
Kidney injury molecule-1 (KIM-1)
KIM-1 is another marker of AKI that has potential clinical utility when measured in plasma and urine. It has been identified as an indicator of AKI, with urinary KIM-1 showing significant elevation within 24 hours, well before significant increases in serum creatinine are noted (40). This is due to KIM-1 being a direct marker of renal injury, rather than its relationship to renal function and filtration (41). Elevation of KIM-1 particularly associated with ischaemic kidney injury (42). It is present in damaged proximal tubule apical membranes, and is cleaved by metalloproteinases into the lumen. It is not present on the proximal tubule epithelial cells in the absence of disease, so levels in the urine are correlated with renal tubule damage. Urinary KIM-1 also has utility in CKD, with levels correlating to fibrotic changes in the kidneys (40). KIM-1 measurement in the blood may also have utility, as injured tubule cells lose polarity, and the cleaved KIM-1 may enter the circulation. Indeed, raised levels of KIM-1 in the blood have been associated with acute kidney disease due to renal ischaemia, toxic nephropathy, and diabetic nephropathy. No significant interference to KIM-1 has been identified (42,43). Methods to measure KIM-1 include electrochemiluminescent immunoassay (44) and ELISA (45).
Urinary interleukin-18 (IL-18)
Urinary IL-18 is a urinary marker of AKI. It is expressed by monocytes, macrophages, and proximal tubular epithelial cells, and may be associated with increased infiltration of white blood cells into the renal parenchyma (46). Its utility is in identifying acute tubular necrosis (ATN), being particularly elevated in this disorder, while not being markedly elevated in other renal disorders (47). It should also be noted that IL-18 may also be raised in a number of nonrenal pathologies, such as myocardial infarction and pulmonary disease (46). Recent studies have looked at the combination of urinary KIM-1 and IL-18 to assess their predictive ability for AKI in combination (40). Methods used to measure IL-18 include immunoassays, such as ELISA (46).
Tissue inhibitor of metalloproteinases 2 (TIMP2) and insulin-like growth factor binding protein 7 (IGFBP7)
TIMP2 and IGFBP7 are involved in the cell cycle, both being involved in cell arrest during the first gap phase (G1), with their upregulation coinciding with the early stages of cell injury (48). They are a relatively new urinary biomarker of kidney injury, and thus lack a lot of the evidence of other biomarkers. The performance of these biomarkers is better when they are combined to form the product (TIMP2 × IGFBP7), with TIMP2 found to be a better marker of in patients with AKI induced by sepsis, and IGFBP7 superior in post-surgery patients (25). Studies have highlighted the ability of the TIMP2 and IGFBP7 urinary biomarkers to identify AKI within hours of occurring (49). However, further research is needed to further define the utility of this earlier diagnosis in the clinical setting. Indeed, studies suggest that this earlier recognition of AKI may not limit its progression. A further limitation of the (TIMP2), (IGFBP7) product is that it is increased in diabetics, and further research is needed to fully support its implementation in a clinical setting (50). TIMP2 and IGFBP3 can be measured in urine with a sandwich immunoassay technique (51).
These urinary markers are associated with a number of associated limitations. They are generally more expensive than their routinely available counterparts. In addition, they are not routinely available across analytical platforms. Furthermore, they are not standardised between different assay manufacturers and laboratories, so results are not comparable unless done at the same laboratory with the same method.
Urinary albumin and protein
Urinary albumin and protein have the potential to both indicate the presence of kidney disease, and cause kidney disease. Debate still exists over whether to perform albumin or protein levels in urine (52). Looking just for albumin risks missing the presence of tubular or overflow proteinuria, but albumin has been found to correlate more closely with kidney disease progression in diabetes (53), as well as glomerular disease in hypertension (54). Often, the choice of which to use will come down to the clinical scenario. For example, albumin should be used in diabetes mellitus to assess for microalbuminuria, while proteinuria is recommended in preeclampsia workup (55). Unless a total protein level is specifically required, urinary albumin levels are seen as clinically superior (56). It must be noted that there are causes of albuminuria other than kidney disease, such as upright posture, heart failure, and urinary tract infection. Thus, spot urines upon waking are recommended, with a urinary albumin:creatinine ratio used. Note there are gender specific cut-offs, and positive results should be confirmed, with two out of three positive results within a month being consistent with albuminuria (8). In the laboratory, urinary albumin is typically analysed using a sensitive immunonephelometric method, turbidimetric, although dipstick, electrophoresis, and liquid chromatography do exist (57). Differences exist within and between methods, in part due to the presence of different fragments and modifications of albumin being detected heterogeneously by different assays (58). Protein is potentially analysed using a number of methods, including colorimetric, electrophoretic, or nephelometric assays (59). Like urinary albumin, differences in results exist between these methods, even related methods like the dye-binding assays Coomassie Brilliant Blue and Pyrogallol Red-molybdate, highlighting the need for a common calibrator, or standardisation program, between methods (57).
Proteins less than 5 kDa are typically completely filtered, proteins larger than this but smaller than albumin (<66 kDa) are typically partially filtered, and proteins larger than albumin are typically retained (60). Small proteins such as A1M, is mostly filtered at the glomerulus, but 99% is reabsorbed by the proximal tubule cells in health (61). If tubular function is compromised, the A1M:creatinine ratio in urine will increase. Albumin, while also typically 99% reabsorbed by the proximal tubule cells in health, is also largely prevented from entering the glomerular filtrate in health, being retained by the glomerulus. Its presence in urine, typically expressed as its creatinine ratio, indicates significant glomerular damage. Urine transferrin can also be used to this effect (62). Urinary analysis for immunoglobulins may also be done as a marker of distal tubule leakage due to infection or inflammation, although severe glomerular proteinuria or haematuria may also cause an increase (63). A protein selectivity index may be used as a tool to see where the injury is in the nephron, but is generally seen to not be useful (8).
The presence of protein in urine is not linked exclusively to kidney disease. Overflow proteinuria occurs when levels of small proteins in plasma are filtered and exceed the tubules’ capacity for reabsorption. Such proteins may include myoglobin (seen with muscle damage), Bence Jones proteins (seen in plasma cell neoplasms and amyloidosis), and lysozyme (seen in leukaemias) (64). However, the presence of these proteins in high concentrations within the tubule lumen is linked to kidney disease. In healthy individuals, the predominant protein found within urine is the acidic protein, Tamm-Horsfall glycoprotein, which is secreted by the tubules.
Markers of renal tubular function
Damage of the renal tubulointerstitial component is important to consider in renal pathophysiology, as it typically manifests without significant glomerular damage, increased serum creatinine, or reduced eGFR, and are evidenced through overt proteinuria (65). Indeed, chronic renal disease has been found to be more closely correlated by the extent of tubulointerstitial disease than glomerular function markers (66). The various causes of tubulointerstitial disease include various medications, heavy metals, metabolic disorders, renal infections, and autoimmune diseases (67). Since the injury affects the tubules directly, markers are seen in urine.
A1M
A1M is a lipocalin protein freely filtered at the glomerulus, due to its molecular weight of 26 kDa (68). It is almost completely (99%) reabsorbed at the proximal convoluted tubules, so high levels in urine suggest proximal tubular injury or compromised function (65). Its stability at low pH seen in urine adds to its utility as a marker of renal tubular injury. It is typically determined using an immunonephelometric method (69).
Retinol binding protein (RBP)
RBP is a 21 kDa protein that is involved in vitamin A transport systemically, and is otherwise cleared by kidney when vitamin A and transthyretin are not bound. It is broken down and reabsorbed by the proximal renal tubule cells in health (65). Studies have not shown that RBP has any superior clinical utility to A1M (70,71). Immunonephelometric methods are typically used to quantify RBP.
Beta-2-microglobulin
Beta-2-microglobulin is a protein of the light chain portion of the major histocompatibility complex class I, it is freely filtered at the glomerulus, with a molecular weight of 11.8 kDa. Elevated urinary levels are linked to proximal tubular injury (72). It has particular clinical utility in detecting tubular injury related to heavy metal exposure. Immunometric methods are typically used. Care must be taken to ensure the specimen is not exposed to acidic conditions (pH <6.0) for long periods (70).
N-Acetyl-β-D-glucosaminidase
N-Acetyl-β-D-glucosaminidase is a lysosomal enzyme found at high levels in the proximal tubule, and is released into urine upon injury to the proximal tubule cells (73). Methods to determine levels include an enzymatic assay (74). While it is a sensitive marker of tubular injury, it has yet to be shown to have an advantage over other markers of renal tubular function (8).
Glutathione-s-transferase (GST)
GST is a cytoplasmic enzyme that occurs at a high level in the renal tubular cells, and leaks out with damage. One of the possible utilities in using urinary GST was identifying the α-GST isoenzyme (proximal renal tubule specific) and π-GST isoenzyme (distal renal tubule specific) to localise the tubule defect, but studies have not shown a clear demarcation for specific tubule localization (75). Enzymatic immunoassay methods may be used to determine their levels.
Liver-type fatty acid binding protein (LFABP)
LFABP is a 15 kDa protein that is produced by renal proximal tubules, and its expression is proportionally increased in tubulointerstitial disease (65). Methods to measure LFABP are include immunoassays, such as ELISA (66).
Urinary cystatin C
Urinary cystatin C, in contrast to its role as a marker in serum of glomerular function, has potential utility as a marker of tubular damage, with urinary elevations consistent with tubular dysfunction, as compared with normal levels seen in glomerular dysfunction (76). Its level in urine is also correlated with AKI (77).
Most of these markers in urine are typically offered with 24-hour collections, or in spot collections. Twenty-four-hour urines may require an additive to preserve the analyte during the collection period. Spot urines may be used to offer faster turnaround, preserve analyte stability, and are typically easier for the patient. When spot urines are used, the analyte is typically presented as its ratio to urine creatinine, as urine creatinine excretion is typically constant between days in an individual, and can differentiate between dilute and concentrated urine specimens. A setback in using urine creatinine ratios is that creatinine is dependent on muscle mass, so creatinine excretion will differ between genders, body habitus, and extremes of age.
Indirect markers of renal function
Many biochemical analytes are affected by changes in renal function, whether it is due to reduced production by the kidneys, reduced clearance, or altered physiology. Some biochemical markers are particularly useful to monitor in renal disease, due to their diagnostic, therapeutic, or prognostic utility.
Fibroblast growth factor 23 (FGF23)
FGF23 is a phosphatonin molecule produced predominantly by osteoblast bone cells. It is stimulated by PTH, phosphate, calcitriol, and a cleavage product of Klotho (78). FGF23 promotes renal phosphate wasting by binding to the Klotho-FGF receptor complexes in the proximal renal tubule. This promotes phosphate wasting. It also suppresses 1-alpha-hydroxylase in the kidney, suppressing calcitriol production and hence phosphate absorption from the gastrointestinal system. FGF23 increases very early on in CKD, and increases to proportionately greater levels with the degree of CKD present. This increase is independent of FGF23 clearance by the kidneys (79). FGF23 is typically measured using an automated chemiluminescent immunoassay. Care must be taken when results are compared between different testing platforms, as some will have antibodies to the intact FGF23 (iFGF23), while others will have antibodies directed against the C-terminal peptide fragments of FGF23 (cFGF23) (78). Result correlation between these two assays is weak. FGF23 may be elevated by many nonrenal conditions such as fibrous dysplasia, tumour-induced osteomalacia, and hereditary rickets (80).
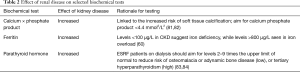
Many biochemical parameters are commonly abnormal in renal disease, reflecting the kidney’s role in functions other than plasma filtration. Some of these biochemical parameters may be increased, such as uric acid, chromogranin A, and amylase; while others may be decreased, such as calcitriol, erythropoietin, and ionised calcium. Some biochemical parameters are typically monitored in renal disease, including those seen in Table 2.
Full table
Conclusions
Markers of kidney disease tend to be restricted by a few common limitations. Firstly, many are not widely available, with testing being limited to certain methods, analysers and manufacturers. This limits their utility in being used to routinely monitor kidney disease. In contrast to most analytes, creatinine is widely available, and relatively specific for renal function. This is in contrast to the urinary markers, many of which are new and unfamiliar to clinicians, relatively costly, and lack the demonstrated clinical benefit over current methods to fully justify their wide implementation. Another difficulty is the heterogeneity between the different markers and their ability to detect different pathologies and influence outcomes. Diagnosing AKI or CKD stage may be done differently between the studies, limiting the ability to directly compare different biomarkers and studies to one another.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Swan SK. The search continues--an ideal marker of GFR. Clin Chem 1997;43:913-4. [PubMed]
- Seegmiller JC, Eckfeldt JH, Lieske JC. Challenges in Measuring Glomerular Filtration Rate: a Clinical Laboratory Perspective. Adv Chronic Kidney Dis 2018;25:84-92. [Crossref] [PubMed]
- Hosten AO. BUN and Creatinine. In: Walker HK, Hall WD, Hurst JW (eds). Clinical Methods: the History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths, 1990;874-8.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl 2013;3:136-50.
- Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012;2:1-138.
- Stevens LA, Levey AS. Measured GFR as a confirmatory test for estimated GFR. J Am Soc Nephrol 2009;20:2305-13. [Crossref] [PubMed]
- Burballa C, Crespo M, Redondo-Pachón D, et al. MDRD or CKD-EPI for glomerular filtration rate estimation in living kidney donors. Nefrologia 2018;38:207-12. [Crossref] [PubMed]
- Lamb EJ, Jones GRD. Kidney Function Tests. In: Rifai N, Horvath AR, Wittwer C (eds). Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 6th Edition. Philadelphia: W.B. Saunders, 2018:479-516.
- Kooman JP. Estimation of renal function in patients with chronic kidney disease. J Magn Reson Imaging 2009;30:1341-6. [Crossref] [PubMed]
- Peake M, Whiting M. Measurement of Serum Creatinine – Current Status and Future Goals. Clin Biochem Rev 2006;27:173-84. [PubMed]
- Kemperman FA, Weber JA, Gorgels J, et al. The influence of ketoacids on plasma creatinine assays in diabetic ketoacidosis. J Intern Med 2000;248:511-7. [Crossref] [PubMed]
- Dick JB, Bartlett WA, Ibrahim U, et al. Interference of fluorescein with creatinine assays. Ann Clin Biochem 1991;28:311-3. [Crossref] [PubMed]
- Creatinine method insert chemistry information sheet. California: Beckman-Coulter. Brea, 2015.
- Cholongitas E, Marelli L, Kerry A, et al. Different methods of creatinine measurement significantly affect MELD scores. Liver Transpl 2007;13:523-9. [Crossref] [PubMed]
- Dimeski G, McWhinney B, Jones B, et al. Extent of bilirubin interference with Beckman creatinine methods. Ann Clin Biochem 2008;45:91-2. [Crossref] [PubMed]
- Carobene A, Ferrero C, Ceriotti F, et al. Creatinine measurement proficiency testing: assignment of matrix-adjusted ID GC-MS target values. Clin Chem 1997;43:1342-7. [PubMed]
- Schmidt RL, Straseski JA, Raphael KL, et al. Assessment of the Jaffe vs Enzymatic Method for Creatinine Measurement in an Outpatient Population. PLoS One 2015;10:e0143205. [Crossref] [PubMed]
- Silva MV, Moscoso Solorzano G, Nishida SK, et al. Are serum cystatin C levels influenced by steroid doses in lupus nephritis patients? J Bras Nefrol 2011;33:306-12. [Crossref] [PubMed]
- Filler G, Bökenkamp A, Hofmann W, et al. Cystatin C as a marker of GFR--history, indications, and future research. Clin Biochem 2005;38:1-8. [Crossref] [PubMed]
- Ristiniemi N, Savage C, Bruun L, et al. Evaluation of a new immunoassay for cystatin C, based on a double monoclonal principle, in men with normal and impaired renal function. Nephrol Dial Transplant 2012;27:682-7. [Crossref] [PubMed]
- Akbas N, Gonzalez G, Devaraj S. Evaluation of the Lipid Interference for Siemens BN ProSpec Cystatin C Assay Using Pediatric Samples. Ann Clin Lab Sci 2015;45:562-4. [PubMed]
- Shlipak MG, Mattes MD, Peralta CA. Update on Cystatin C:Incorporation Into Clinical Practice. Am J Kidney Dis 2013;62:595-603. [Crossref] [PubMed]
- Pasala S, Carmody JB. How to use… serum creatinine, cystatin C and GFR. Arch Dis Child Educ Pract Ed 2017;102:37-43. [Crossref] [PubMed]
- Frazee E, Rule AD, Lieske JC, et al. Cystatin C-Guided Vancomycin dosing in critically ill patients: a quality Improvement project. Am J Kidney Dis 2017;69:658-66. [Crossref] [PubMed]
- Klein SJ, Brandtner AK, Lehner GF, et al. Biomarkers for prediction of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Intensive Care Medicine 2018;44:323-36. [Crossref] [PubMed]
- Diez C, Mohr P, Koch D, et al. Age- and gender-specific values of estimated glomerular filtration rate among 6232 patients undergoing cardiac surgery. Interact Cardiovasc Thorac Surg 2009;9:593-7. [Crossref] [PubMed]
- Nyman HA, Dowling TC, Hudson JQ, et al. Comparative evaluation of the Cockcroft-Gault Equation and the Modification of Diet in Renal Disease (MDRD) study equation for drug dosing: an opinion of the Nephrology Practice and Research Network of the American College of Clinical Pharmacy. Pharmacotherapy 2011;31:1130-44. [Crossref] [PubMed]
- Rule AD. The CKD-EPI equation for estimating GFR from serum creatinine: real improvement or more of the same? Clin J Am Soc Nephrol 2010;5:951-3. [Crossref] [PubMed]
- Johnson DW, Jones GR, Mathew TH, et al. Chronic kidney disease and automatic reporting of estimated glomerular filtration rate: new developments and revised recommendations. Med J Aust 2012;197:224-5. [Crossref] [PubMed]
- Florkowski CM, Chew-Harris JS. Methods of Estimating GFR – Different Equations Including CKD-EPI. Clin Biochem Rev 2011;32:75-9. [PubMed]
- Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol 2009;4:1832-43. [Crossref] [PubMed]
- Zheng K, Gong M, Qin Y, et al. Validation of glomerular filtration rate-estimating equations in Chinese children. PLoS One 2017;12:e0180565. [Crossref] [PubMed]
- Chen HH. Beta Trace-Protein versus Cystatin C: Which is a Better Surrogate Marker of Renal Function versus Prognostic Indicator in Cardiovascular Diseases? J Am Coll Cardiol 2011;57:859-60. [Crossref] [PubMed]
- Bode-Böger SM, Scalera F, Kielstein JT, et al. Symmetrical dimethylarginine: a new combined parameter for renal function and extent of coronary artery disease. J Am Soc Nephrol 2006;17:1128-34. [Crossref] [PubMed]
- Kusano E, Suzuki M, Asano Y, et al. Human alpha 1-microglobulin and its relationship to renal function. Nephron 1985;41:320-4. [Crossref] [PubMed]
- Donadio C, Lucchesi A, Ardini M, et al. Cystatin C, beta 2-microglobulin, and retinol-binding protein as indicators of glomerular filtration rate: comparison with plasma creatinine. J Pharm Biomed Anal 2001;24:835-42. [Crossref] [PubMed]
- Haase-Fielitz A, Haase M, Devarajan P. Neutrophil gelatinase-associated lipocalin as a biomarker of acute kidney injury: a critical evaluation of current status. Ann Clin Biochem 2014;51:335-51. [Crossref] [PubMed]
- Cullen MR, Murray PT, Fitzgibbon MC. Establishment of a reference interval for urinary neutrophil gelatinase-associated lipocalin. Ann Clin Biochem 2012;49:190-3. [Crossref] [PubMed]
- Krzeminska E, Wyczalkowska-Tomasik A, Korytowska N, et al. Comparison of Two Methods for Determination of NGAL Levels in Urine: ELISA and CMIA. J Clin Lab Anal 2016;30:956-60. [Crossref] [PubMed]
- Shao X, Tian L, Xu W, et al. Diagnostic Value of Urinary Kidney Injury Molecule 1 for Acute Kidney Injury: a Meta-Analysis. PLoS One 2014;9:e84131. [Crossref] [PubMed]
- Bonventre JV. Kidney injury molecule-1 (KIM-1): a urinary biomarker and much more. Nephrol Dial Transplant 2009;24:3265-8. [Crossref] [PubMed]
- Sabbisetti VS, Waikar SS, Antoine DJ, et al. Blood Kidney Injury Molecule-1 Is a Biomarker of Acute and Chronic Kidney Injury and Predicts Progression to ESRD in Type I Diabetes. J Am Soc Nephrol 2014;25:2177-86. [Crossref] [PubMed]
- Vaidya VS, Ramirez V, Ichimura T, et al. Urinary kidney injury molecule-1: a sensitive quantitative biomarker for early detection of kidney tubular injury. Am J Physiol Renal Physiol 2006;290:F517-29. [Crossref] [PubMed]
- McWilliam SJ, Antoine DJ, Sabbisetti V, et al. Reference intervals for urinary renal injury biomarkers KIM-1 and NGAL in healthy children. Biomark Med 2014;8:1189-97. [Crossref] [PubMed]
- Zhou R, Xu Y, Shen J, et al. Urinary KIM-1: a novel biomarker for evaluation of occupational exposure to lead. Sci Rep 2016;6:38930. [Crossref] [PubMed]
- Lin X, Yuan J, Zhao Y, Zha Y. Urine interleukin-18 in prediction of acute kidney injury: a systemic review and meta-analysis. J Nephrol 2015;28:7-16. [Crossref] [PubMed]
- Parikh CR, Jani A, Melnikov VY, et al. Urinary interleukin-18 is a marker of human acute tubular necrosis. Am J Kidney Dis 2004;43:405-14. [Crossref] [PubMed]
- Kashani K, Al-Khafaji A, Ardiles T, et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care 2013;17:R25. [Crossref] [PubMed]
- Wang Y, Zou Z, Jin J, et al. Urinary TIMP-2 and IGFBP7 for the prediction of acute kidney injury following cardiac surgery. BMC Nephrol 2017;18:177. [Crossref] [PubMed]
- Liu C, Lu X, Mao Z, et al. The diagnostic accuracy of urinary [TIMP-2]·[IGFBP7] for acute kidney injury in adults: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 2017;96:e7484. [Crossref] [PubMed]
- Westhoff JH, Tönshoff B, Waldherr S, et al. Urinary Tissue Inhibitor of Metalloproteinase-2 (TIMP-2) • Insulin-Like Growth Factor-Binding Protein 7 (IGFBP7) Predicts Adverse Outcome in Pediatric Acute Kidney Injury. PLoS One 2015;10:e0143628. [Crossref] [PubMed]
- Fisher H, Hsu C, Vittinghoff E, et al. Comparison of Associations of Urine Protein-Creatinine Ratio Versus Albumin-Creatinine Ratio With Complications of CKD: a Cross-sectional Analysis. Am J Kidney Dis 2013;62:1102-8. [Crossref] [PubMed]
- Gross JL, de Azevedo MJ, Silveiro SP, et al. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care 2005;28:164-76. [Crossref] [PubMed]
- Shihabi ZK, Konen JC, O'Connor ML. Albuminuria vs urinary total protein for detecting chronic renal disorders. Clin Chem 1991;37:621-4. [PubMed]
- Morris RK, Riley RD, Doug M, et al. Diagnostic accuracy of spot urinary protein and albumin to creatinine ratios for detection of significant proteinuria or adverse pregnancy outcome in patients with suspected pre-eclampsia: systematic review and meta-analysis. BMJ 2012;345:e4342. [Crossref] [PubMed]
- Lamb EJ, McTaggart MP, Stevens PE. Why albumin to creatinine ratio should replace protein to creatinine ratio:it is not just about nephrologists. Ann Clin Biochem 2013;50:301-5. [Crossref] [PubMed]
- Marshall T, Williams KM. Total protein determination in urine: elimination of a differential response between the Coomassie blue and pyrogallol red protein dye-binding assays. Clin Chem 2000;46:392-8. [PubMed]
- Viswanathan G, Upadhyay A. Assessment of proteinuria. Adv Chronic Kidney Dis 2011;18:243-8. [Crossref] [PubMed]
- Sapan CV, Lundblad RL. Review of methods for determination of total protein and peptide concentration in biological samples. Proteomics Clin Appl 2015;9:268-76. [Crossref] [PubMed]
- Delaney MP, Lamb EJ. Kidney Disease. In: Rifai N, Horvath AR, Wittwer C (eds). Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 6th Edition. Philadelphia: W.B. Saunders, 2018:1256-323.
- Andersson L, Haraldsson B, Johansson C, et al. Methodological issues on the use of urinary alpha-1-microglobuline in epidemiological studies. Nephrol Dial Transplant 2008;23:1252-6. [Crossref] [PubMed]
- Fraij BM. Transferrin and albumin excretion as a measure of glomerular function. Clin Physiol Biochem 1989;7:296-302. [PubMed]
- Tencer J, Torffvit O, Thysell H, et al. Proteinuria selectivity index based upon alpha 2-macroglobulin or IgM is superior to the IgG based index in differentiating glomerular diseases. Technical note. Kidney Int 1998;54:2098-105. [Crossref] [PubMed]
- Waller KV, Ward KM, Mahan JD, et al. Current concepts in proteinuria. Clin Chem 1989;35:755-65. [PubMed]
- Fiseha T, Gebreweld A. Urinary Markers of Tubular Injury in HIV-Infected Patients. Biochem Res Int 2016;2016:1501785. [Crossref] [PubMed]
- Kamijo A, Sugaya T, Hikawa A, et al. Urinary Excretion of Fatty Acid-Binding Protein Reflects Stress Overload on the Proximal Tubules. Am J Pathol 2004;165:1243-55. [Crossref] [PubMed]
- Perazella MA. Clinical Approach to Diagnosing Acute and Chronic Tubulointerstitial Disease. Adv Chronic Kidney Dis 2017;24:57-63. [Crossref] [PubMed]
- Akerström B, Lögdberg L, Berggård T, et al. Alpha(1)-Microglobulin: a yellow-brown lipocalin. Biochim Biophys Acta 2000;1482:172-84. [Crossref] [PubMed]
- Yu H, Yanagisawa Y, Forbes MA, et al. Alpha-1-microglobulin: an indicator protein for renal tubular function. J Clin Pathol 1983;36:253-9. [Crossref] [PubMed]
- Penders J, Delanghe JR. Alpha 1-microglobulin:clinical laboratory aspects and applications. Clin Chim Acta 2004;346:107-18. [Crossref] [PubMed]
- Donaldson MD, Chambers RE, Woolridge MW, et al. Alpha 1-microglobulin, beta 2-microglobulin and retinol binding protein in childhood febrile illness and renal disease. Pediatr Nephrol 1990;4:314-8. [Crossref] [PubMed]
- Zeng X, Hossain D, Bostwick DG, et al. Urinary β2-Microglobulin Is a Good Indicator of Proximal Tubule Injury: a Correlative Study with Renal Biopsies. J Biomark 2014;2014:492838. [Crossref] [PubMed]
- Skálová S. The diagnostic role of urinary N-acetyl-beta-D-glucosaminidase (NAG) activity in the detection of renal tubular impairment. Acta Medica (Hradec Kralove) 2005;48:75-80. [Crossref] [PubMed]
- Pócsi I, Taylor SA, Richardson AC, et al. "VRA-GlcNAc": novel substrate for N-acetyl-beta-D-glucosaminidase applied to assay of this enzyme in urine. Clin Chem 1990;36:1884-8. [PubMed]
- Shu KH, Wang CH, Wu CH, et al. Urinary π-glutathione S-transferase Predicts Advanced Acute Kidney Injury Following Cardiovascular Surgery. Sci Rep 2016;6:26335. [Crossref] [PubMed]
- Conti M, Moutereau S, Zater M, et al. Urinary cystatin C as a specific marker of tubular dysfunction. Clin Chem Lab Med 2006;44:288-91. [Crossref] [PubMed]
- Nejat M, Pickering JW, Walker RJ, et al. Urinary cystatin C is diagnostic of acute kidney injury and sepsis, and predicts mortality in the intensive care unit. Crit Care 2010;14:R85. [Crossref] [PubMed]
- Fraser WD. Bone and Mineral Metabolism. In: Rifai N, Horvath AR, Wittwer C (eds). Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 6th Edition. Philadelphia: W.B. Saunders, 2018:1422-90.
- Russo D, Battaglia Y. Clinical Significance of FGF-23 in Patients with CKD. Int J Nephrol 2011;2011:364890. [Crossref] [PubMed]
- Liu S, Quarles LD. How fibroblast growth factor 23 works. J Am Soc Nephrol 2007;18:1637-47. [Crossref] [PubMed]
- Mannstadt M, Bilezikian JP, Thakker RV, et al. Hypoparathyroidism. Nat Rev Dis Primers 2017;3:17080. [Crossref] [PubMed]
- Tertti R, Harmoinen A, Leskinen Y, et al. Comparison of calcium phosphate product values using measurement of plasma total calcium and serum ionized calcium. Hemodial Int 2007;11:411-6. [Crossref] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD–MBD). Kidney Int Suppl 2009;76:S121-30.
- Yuen NK, Ananthakrishnan S, Campbell MJ. Hyperparathyroidism of Renal Disease. Perm J 2016;20:78-83. [PubMed]


