
What about the partner? —factors associated with patient-perceived partner dyspareunia in men with Peyronie’s disease
Introduction
Peyronie’s disease (PD) is a wound-healing disorder characterized by fibrous plaque depositions in tunica albuginea leading to penile curvature, deformity, pain and erectile dysfunction. While penile pain typically resolves without treatment, curvature and deformity usually persist past the acute phase. Reported prevalence of PD has ranged from 0.5% to 20.3%, with the higher rates seen within specific populations (1,2).
Men with PD can experience significant emotional and relationship distress (3). PD’s psychological effects have been well-characterized, with 48% of men reporting depressive symptoms that do not resolve over time and 54% of men describing relationship difficulties due to PD (4,5). Additionally, men with PD report higher levels of anxiety with decreased confidence in sexual situations and increased fear of not satisfying their partners (6).
Beyond the limited data on the impact of PD on relationships, there are even fewer reports on how partners of men with PD are affected by the disease. Partner pain is known to negatively impact patients’ sexual relationships (7). Thus, an improved understanding of how PD affects intercourse with partners is needed. In the current study, we aim to characterize PD patients whose curvatures cause pain to partners during penetrative intercourse.
Methods
Following Mayo Clinic Institutional Review Board approval, a database was maintained of all sequential patients undergoing evaluation for PD in the Department of Urology between March 2014 and June 2016. This constituted the initial study population.
As part of the initial evaluation, new patients were asked to complete a 74-item questionnaire regarding their penile curvature and other sexual health concerns. This questionnaire, which contained prompts regarding relationship duration, frequency of sexual intercourse, erection duration, estimated penile curvature, and curve-related sexual dysfunction, was composed by a fellowship-trained Andrologist. A non-validated scale from 0–10 was used to separately assess patient bother associated with penile curvature and erection strength. The standardized 15-item International Index of Erectile Function (IIEF) questionnaire was included to assess erectile function. Branching logic questions were used to limit responses to personally relevant items on the basis of prior responses, resulting in variation of the total number of questions presented to each participant. All patients had the opportunity to decline to answer any question, and not all patients completed each question. For the current study, patients were stratified based on their response to the question: “Does the curvature cause your partner any pain during penetrative intercourse?”
Patients underwent physical exam to evaluate for palpable plaques and to measure stretched penile length in the flaccid state. To measure objective penile curvature, intracavernosal injection of a standard combination of erectogenic medications utilizing either Trimix (papaverine 24 mg/mL, phentolamine 1 mg/mL and alprostadil 10 µg/mL) or Bimix (papaverine 30 mg/mL and alprostadil 10 µg/mL) was performed to achieve a goal erection score of 8/10, or until a maximum of 1 mL of medication was administered. A goniometer was used to estimate the curvature, and men with multiplanar curvatures were assessed in both the anterior/posterior and lateral planes. A “composite curve” was obtained by summing the primary (larger) and secondary (smaller) curves, as this was felt to be a better characterization of the true curvature (2). There were no patients with two discrete curve locations in the current series. All men underwent penile Duplex Doppler ultrasonography (PDDU) using a 12.5 MHz probe to evaluate penile vascular flow, the presence and location of a visible plaque, and the presence and degree of plaque calcification.
Statistical analysis was performed to identify differences in clinicopathologic variables between those patients who did and did not report partner pain with intercourse. The student’s t-test was used to compare continuous variables, while the Chi-square (Fisher exact) test was used for categorical variables. All P values were two-sided, with P<0.05 considered statistically significant. Statistical analyses were performed using SAS software, version 9.3 (SAS Institute, Cary, NC; www.sas.com).
Results
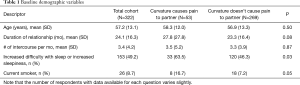
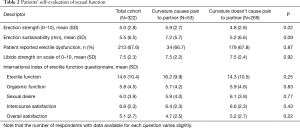
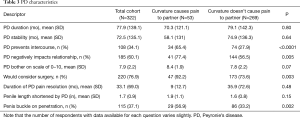
A total of 322 patients with PD met inclusion criteria and completed the initial evaluation and survey. Patient demographics are shown in Table 1. Mean patient age was 57.2 years (SD 13.1). Patients with partner pain were significantly more likely to be current smokers and to have difficulty with sleep. Table 2 details patients’ self-assessment of sexual function. Patient-reported subjective erectile strength on a scale of 0–10 was significantly higher in patients who reported partner pain with intercourse (5.9 vs. 4.8, P=0.02). Table 3 shows characteristics of PD. Those with partner pain were also more likely to consider surgery, report that curvature prevents intercourse, and indicate that the disease was negatively impacting their relationships. Patients with partner pain subjectively report higher frequencies of penile buckling upon penetration. Surprisingly, there was no significant difference in the patient-reported degree of bother with their PD stratified based on whether they did or did not attest to partner pain. As is shown in the table, there was also no significant difference in patient reported pain with erections in either group.
Full table
Full table
Full table
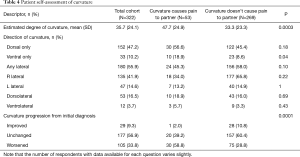
Patient responses to questions related specifically to penile curvature are shown in Table 4. Patients with subjectively-reported ventral curvature or higher subjective degrees of curvature were more likely to cause pain to partners (18.9% vs. 8.6%, P=0.04; 47.7° vs. 33.3°, P=0.0003). Since time of initial PD diagnosis, patients who noted improved or stable penile curvature at time of consultation were less likely to complain of partner pain, whereas those with partner pain were more likely to have experienced worsening of their curvatures.
Full table
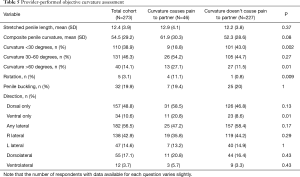
Table 5 shows objective curvature assessments taken of 322 patients. Consistent with patient subjective reports, those with partner pain were more likely to have a purely ventral curvature (20.8% vs. 8.6%, P=0.01) and had non-significantly increased degrees of composite penile curvature (61.9° vs. 52.3°, P=0.08). Objective assessments of the degree of penile curvature were 15–20° higher than subjective reports in both groups of patients. When stratified by degrees of curvature, patients with partner pain were significantly less likely to have curvatures less than 30° but more likely to have curvatures greater than 60°.
Full table
Discussion
The current study reports several novel findings and furthers our limited understanding of the effects of PD on partners. Men with greater subjective penile rigidity were more likely to report pain experienced by their partners. These findings are not surprising, as a less firm erection would be expected to be more pliable and result in a functionally reduced curvature. It is important to highlight that IIEF scores are minimally helpful in the setting of more severe PD, as it requires that the patient be able to participate in penetrative intercourse. As men who exhibit significant difficulty with penetration are likely to score very low on the IIEF, this results in a very heterogeneous outcome. As such, subjective reports on the overall erectile rigidity may be a more reliable measure in this setting.
Findings also demonstrated that those with greater curvatures were also more likely to report partner pain. This is intuitive, as a larger degree of deformity would be expected to deform the orifice penetrated to a greater extent and hence result in greater pain. These findings are also supported by data from Walsh and colleagues, who previously reported an association between curvatures >60° and difficulty in having penetrative intercourse (8).
The direction of curvature was also notably important in differentiating the likelihood for causing partner pain, with ventral curvatures found to be associated. There are several reasons why this particular direction may lead to partner pain. For heterosexual men engaging in vaginal intercourse, ventral curvatures may make penetrating the orifice more difficult due the downward curvature of the penis interacting with the upward-curving vaginal canal. Compared to other directions of curvature, ventral curvatures may make finding other positions during intercourse more difficult or prevent the penis from angulating to compensate for the curvature, resulting in a higher chance of partner pain. It is important to note that the current set of questionnaires does not ask questions on sexual orientation or how and where penetrative intercourse is performed. These factors may represent uncontrolled confounders with the current series.
Beyond the physical characteristics of the erection, PD clearly impacts several psychological aspects of sexual function. Men with PD frequently feel embarrassed, ashamed and clinically depressed about their condition, with many expressing a sense of inadequacy and feeling less masculine. These negative effects of PD on men’s self-image lead to withdrawal from physical intimacy, as any form of sexual activity may remind them of their disease (3,4,6). Many also express anxiety about hurting their partners during intercourse (6). The combination of psychological and physical distress experienced by men with PD is the precursor for relationship problems with their partners.
Although PD has been known to adversely affect relationships including negative psychosocial effects on partners of men with PD, there is a surprising paucity of literature exploring partner satisfaction related to PD (9). Prior reports have suggested that up to 54% of men with PD have relationship problems, with risk factors being loss of penile length, low libido and penile pain (5). Female partners of men with PD have also been found to have decreased sexual function, sexual satisfaction and mood compared with population-based norms (10). Partners may also directly impact the patients’ decisions to correct their deformities, which is supported by our finding that those experiencing partner pain were more likely to consider surgical intervention or other invasive therapies.
Men with PD may also exhibit a degree of penile dysmorphia, with inability to objectively and accurately characterize their penile deformities (6). Matsushita and colleagues recently demonstrated that patients often underestimate their degree of curvature and that this is worsened in patients with erectile dysfunction (11). Our study supports this claim as our patients tended to underestimate their degree of curvature by 15–20° on average, with greater curvatures identified on provider measurements following injection of erectogenic agents.
The current study has several notable limitations, including a reliance on data obtained from men with PD about their partners, rather than the partners themselves. As such, we are blinded to confounding partner characteristics including vaginal dryness, vaginismus and vaginal atrophy. Furthermore, the data also only represent a single time-point, with longitudinal follow-up data not available. The question utilized to distinguish the two cohorts is also non-validated (a validated questionnaire does not exist on this topic), and as such, it is possible that some may have misunderstood or misinterpreted what is meant by partner pain.
However, despite these limitations, the study has several strengths. To our knowledge, it represents the first report of characteristics of PD that increase the propensity for partner pain. The data also represent a relatively large series, which permits more robust statistical analyses and greater confidence in the reliability of outcomes.
Partner pain was identified in 16% of our PD patients. Greater erectile function, higher degrees of penile curvature and ventral curvatures were predictors of partner pain during intercourse. Additionally, given the finding that men with partner pain were more likely to seek surgical intervention, the specific disease characteristics reported in this series may assist clinicians in identifying men who are more motivated to select more invasive therapies. Given the shared effects of PD in sexual relationships, this information suggests a need for further research into partner-related treatment outcomes.
Acknowledgements
The authors are grateful to an anonymous and very generous donor who has provided funding for PD research and who made this publication possible.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Mayo Clinic Institutional Review Board (No. 14-008045).
References
- Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's Disease: AUA Guideline. J Urol 2015;194:745-53. [Crossref] [PubMed]
- Ziegelmann MJ, Viers BR, McAlvany KL, et al. Restoration of Penile Function and Patient Satisfaction with Intralesional Collagenase Clostridium Histolyticum Injection for Peyronie's Disease. J Urol 2016;195:1051-6. [Crossref] [PubMed]
- Nelson CJ, Mulhall JP. Psychological impact of Peyronie's disease: a review. J Sex Med 2013;10:653-60. [Crossref] [PubMed]
- Nelson CJ, Diblasio C, Kendirci M, et al. The chronology of depression and distress in men with Peyronie's disease. J Sex Med 2008;5:1985-90. [Crossref] [PubMed]
- Smith JF, Walsh TJ, Conti SL, et al. Risk factors for emotional and relationship problems in Peyronie's disease. J Sex Med 2008;5:2179-84. [Crossref] [PubMed]
- Rosen R, Catania J, Lue T, et al. Impact of Peyronie's disease on sexual and psychosocial functioning: qualitative findings in patients and controls. J Sex Med 2008;5:1977-84. [Crossref] [PubMed]
- Ziegelmann MJ, Alom M, Hebert K, et al. Clinical Factors Negatively Impacting Sexual Relationships in Men With Peyronie's Disease. J Sex Marital Ther 2017.1-7. [Epub ahead of print]. [Crossref] [PubMed]
- Walsh TJ, Hotaling JM, Lue TF, et al. How curved is too curved? The severity of penile deformity may predict sexual disability among men with Peyronie's disease. Int J Impot Res 2013;25:109-12. [Crossref] [PubMed]
- Goldstein I, Knoll LD, Lipshultz LI, et al. Changes in the Effects of Peyronie's Disease After Treatment With Collagenase Clostridium histolyticum: Male Patients and Their Female Partners. Sex Med 2017;5:e124-30. [Crossref] [PubMed]
- Davis SN, Ferrar S, Sadikaj G, et al. Female Partners of Men With Peyronie's Disease Have Impaired Sexual Function, Satisfaction, and Mood, While Degree of Sexual Interference Is Associated With Worse Outcomes. J Sex Med 2016;13:1095-103. [Crossref] [PubMed]
- Matsushita K, Stember DS, Nelson CJ, et al. Concordance between patient and physician assessment of the magnitude of Peyronie's disease curvature. J Sex Med 2014;11:205-10. [Crossref] [PubMed]


