Development of targeted therapeutic strategies and refinement of sperm DNA fragmentation testing
We read with interest a well written and insightful commentary by Drs. Christensen and Humaidan. The authors strongly endorsed the sperm DNA fragmentation (SDF) practice recommendations of Agarwal et al. (1) and raised some important aspects regarding the testing of SDF (2) such as: (I) possible mechanism to explain the implication of SDF on the reproductive outcome; (II) ideal treatment strategies for SDF; and (III) laboratory methodology for SDF.
Two-step hypothesis provides an explanation for the observation of the differing effect of high SDF on reproductive outcomes with natural pregnancy, intrauterine insemination (IUI), in vitro fertilization (IVF), and intracytoplasmic sperm injection (ICSI). The hypothesis highlighted the concept of poor sperm DNA integrity resulting in greater susceptibility to DNA damage in the face of stress (3). However, the relative contribution of intrinsic and extrinsic factors further complicates the issue. High SDF in ejaculated sperm can be a result of either testicular (e.g., protamine deficiency) (4) or post-testicular event (e.g., high oxidative stress during epididymal transit) (5), or many a time, both. Better treatment outcome is only possible with the utilization of targeted treatment strategies based on accurate diagnosis of the underlying condition.
Treatment of factors associated with elevated SDF before application of ART, as suggested by the authors, is of paramount importance. Among treatment strategies currently available, reversal or mitigation of risk factors and/or underlying etiology is the only possible means to promote natural conception in a couple (Table 1). The clear relationship between varicocele and SDF has been reported and summarized by Cho et al. (6) The reversal of etiology by varicocelectomy significantly improves pregnancy rates in patients with clinical varicoceles and high SDF (7,8). The effect of short abstinence in lowering SDF has been documented (9) and its implication on IUI (10) and ICSI (11) outcomes were reported. However, its definite role in improving natural pregnancy rate awaits further studies. While sperm selection and the use of testicular sperm can decrease SDF, assessment of DNA content of an individual sperm during ICSI is still not feasible. Therefore, the risk of complications of pregnancy with very high SDF remains (12). It is important to recognize that the possibility of natural conception offered by reversal of risk factors could restore the fertility potential of the couple, thus providing the possibility of family planning without resorting to assisted reproduction (ART). Hence, the financial burden and risk associated with ART (13) may be avoided. Restoration of fertility potential in an infertile couple empowers them with the autonomy in family planning as their fertile counterpart. Natural conception probably protects the health of offspring by sperm selection mechanisms in vivo since only motile sperm can gain access to female reproductive tract (Table 1). It has been shown that sperm recovered from uterus and oviducts have higher fertilization rate (14).
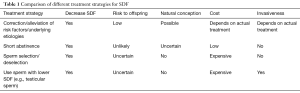
Full table
Lastly, the accuracy and precision of a laboratory test depend on multiple factors. Drs. Christensen and Humaidan enlightened us that “the time has now come to move to the most precise detection method” and “it is essential that the same level of quality control is used for detection of sperm DNA damage as for assessment of conventional semen parameters” (2). In addition to methodological aspects and quality control, as mentioned by the authors, sperm preparation and abstinence period are among other factors (9). Various SDF tests including Sperm Chromatin Structure Assay (SCSA), sperm chromatin dispersion (SCD) and Terminal deoxynucleotidyl transferase dUTP Nick-End Labeling (TUNEL) assays, though detecting a somewhat different type of DNA damage, generally show moderate correlation with each other with correlation coefficients ranging from 0.3 to 0.7 (15,16) pointing to a common origin of damage (3). Drs. Christensen and Humaidan discussed significant advantages of the use of flow cytometry due to its high reliability and precise results. To this end, we recently conducted and published the first multicenter study to create a wider acceptance of establishing TUNEL in the evaluation of SDF as a robust, precise and reproducible test when conducted under standardized assay conditions. The same set of semen samples was independently analyzed in two laboratories (Cleveland, USA, and Basel, Switzerland) by using identical instruments (Accuri C6, BD Biosciences, USA) and protocol. A high correlation in TUNEL results was seen between the two laboratories (r=0.94), and a strong positive correlation was observed between the average SDF rates (r=0.719) (17). Although skepticism in the clinical application of SDF tests persists given the arguable lack of test standardization with precise cut-off levels, numerous studies illustrated the prognostic value of SDF tests in the assessment of sperm DNA damage and fertility potential of an individual irrespective of the testing method used (18). We agree with Drs. Christensen and Humaidan about the importance of precision of a technique in specialized andrology laboratories with standard protocol and quality control. In this scenario, the reliability and clinical application could be ascertained despite the use of different methods of SDF tests. Currently, all SDF tests share the common pitfall that the nature and type of DNA damage are unknown (19). While single-stranded DNA defect may be repaired by oocyte machinery, extensive double-stranded DNA breaks are virtually not repairable and incompatible with normal embryo and fetal development. (20) Although there is a lack of studies on the capacity of human oocytes to repair double-stranded DNA breaks, animal data showed that female mice with defective DNA double-stranded break repair had increased frequencies of zygotes with sperm-derived chromosomal aberrations (21). The capacity to repair sperm DNA breaks also depends on the quality of oocytes. It is demonstrated in human studies that ART outcomes in the presence of SDF vary in women with different ovarian reserves (22,23). Therefore, the pregnancy outcome is the interplay among multiple male and female factors. However, differentiation of types and location of sperm DNA damage is one of the key element before clinical significance of DNA breaks can be characterized. Refining SDF tests based on the currently evolving knowledge is essential in improving the performance of these advanced tests.
We agree with Drs. Christensen and Humaidan in that further studies are needed to unravel the mystery of SDF and DNA damage. Refinement in laboratory methods, understanding of pathophysiology, and development of treatment strategies are interrelated with each other, and any improvement in these different aspects must go hand-in-hand in advancing the care of infertile couples.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Agarwal A, Majzoub A, Esteves SC, et al. Clinical utility of sperm DNA fragmentation testing: practice recommendations based on clinical scenarios. Transl Androl Urol 2016;5:935-50. [Crossref] [PubMed]
- Christensen P, Humaidan P. Testing of sperm DNA damage and clinical recommendations. Transl Androl Urol 2017;6:S607-9.
- Aitken RJ, De Iuliis GN. On the possible origins of DNA damage in human spermatozoa. Mol Hum Reprod 2010;16:3-13. [Crossref] [PubMed]
- Carrell DT, Liu L. Altered protamine 2 expression is uncommon in donors of known fertility, but common among men with poor fertilizing capacity, and may reflect other abnormalities of spermiogenesis. J Androl 2001;22:604-10. [PubMed]
- Aitken RJ, Krausz C. Oxidative stress, DNA damage and the Y chromosome. Reproduction 2001;122:497-506. [Crossref] [PubMed]
- Cho CL, Esteves SC, Agarwal A. Novel insights into the pathophysiology of varicocele and its association with reactive oxygen species and sperm DNA fragmentation. Asian J Androl 2016;18:186-93. [Crossref] [PubMed]
- Smit M, Romijn JC, Wildhagen MF, et al. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol 2013;189:S146-50. [Crossref] [PubMed]
- Ni K, Steger K, Yang H, et al. Sperm protamine mRNA ratio and DNA fragmentation index represent reliable clinical biomarkers for men with varicocele after microsurgical varicocele ligation. J Urol 2014;192:170-6. [Crossref] [PubMed]
- Agarwal A, Gupta S, Du Plessis S, et al. Abstinence Time and Its Impact on Basic and Advanced Semen Parameters. Urology 2016;94:102-10. [Crossref] [PubMed]
- Marshburn PB, Alanis M, Matthews ML, et al. A short period of ejaculatory abstinence before intrauterine insemination is associated with higher pregnancy rates. Fertil Steril 2010;93:286-8. [Crossref] [PubMed]
- Sánchez-Martín P, Sánchez-Martín F, González-Martínez M, et al. Increased pregnancy after reduced male abstinence. Syst Biol Reprod Med 2013;59:256-60. [Crossref] [PubMed]
- Celik-Ozenci C, Jakab A, Kovacs T, et al. Sperm selection for ICSI: shape properties do not predict the absence or presence of numerical chromosomal aberrations. Hum Reprod 2004;19:2052-9. [Crossref] [PubMed]
- Land JA, Evers JL. Risks and complications in assisted reproduction techniques: Report of an ESHRE consensus meeting. Hum Reprod 2003;18:455-7. [Crossref] [PubMed]
- Sakkas D, Ramalingam M, Garrido N, et al. Sperm selection in natural conception: what can we learn from Mother Nature to improve assisted reproduction outcomes? Hum Reprod Update 2015;21:711-26. [Crossref] [PubMed]
- Bungum M, Bungum L, Giwercman A. Sperm chromatin structure assay (SCSA): a tool in diagnosis and treatment of infertility. Asian J Androl 2011;13:69-75. [Crossref] [PubMed]
- Feijó CM, Esteves SC. Diagnostic accuracy of sperm chromatin dispersion test to evaluate sperm deoxyribonucleic acid damage in men with unexplained infertility. Fertil Steril 2014;101:58-63.e3. [Crossref] [PubMed]
- Ribeiro S, Sharma R, Gupta S, et al. Inter- and intra-laboratory standardization of TUNEL assay for assessment of sperm DNA fragmentation. Andrology 2017;5:477-85. [Crossref] [PubMed]
- Gosálvez J, López-Fernández C, Fernández JL, et al. Unpacking the mysteries of sperm DNA fragmentation Ten frequently asked questions. J Reprod Biotechnol Fertil 2015;4:1-16. [Crossref]
- Agarwal A, Cho CL, Esteves SC. Should we evaluate and treat sperm DNA fragmentation? Curr Opin Obstet Gynecol 2016;28:164-71. [Crossref] [PubMed]
- García-Díaz M, Domínguez O, López-Fernández LA, et al. DNA polymerase lambda (Pol lambda), a novel eukaryotic DNA polymerase with a potential role in meiosis. J Mol Biol 2000;301:851-67. [Crossref] [PubMed]
- Marchetti F, Essers J, Kanaar R, et al. Disruption of maternal DNA repair increases sperm-derived chromosomal aberrations. Proc Natl Acad Sci U S A 2007;104:17725-9. [Crossref] [PubMed]
- Meseguer M, Santiso R, Garrido N, et al. Effect of sperm DNA fragmentation on pregnancy outcome depends on oocyte quality. Fertil Steril 2011;95:124-8. [Crossref] [PubMed]
- Jin J, Pan C, Fei Q, et al. Effect of sperm DNA fragmentation on the clinical outcomes for in vitro fertilization and intracytoplasmic sperm injection in women with different ovarian reserves. Fertil Steril 2015;103:910-6. [Crossref] [PubMed]


