
Does Medicaid cover artificial urinary sphincter and male urethral sling surgery?—a state-by-state analysis
Highlight box
Key findings
• Artificial urinary sphincter insertion and male urethral sling procedure are under the coverage of Medicaid in nearly all states.
What is known and what is new?
• Many patients experience urinary incontinence following radical prostatectomy. However, many of these patients do not pursue surgical management of their urinary incontinence.
• There is no readily available report on the Medicaid coverage of artificial urinary sphincter insertion and male urethral sling procedure in the United States.
• In this study, we report that artificial urinary sphincter insertion and male urethral sling procedure are covered by Medicaid in most states.
What is the implication, and what should change now?
• Knowledge of Medicaid coverage for surgeries aimed at treating urinary incontinence may result in increased utilization of these treatment modalities and improve access to care in the Medicaid cancer survivorship population.
Introduction
Stress urinary incontinence (SUI) is defined as involuntary leakage of urine with effort or exertion (1). The reported average incidence of SUI is estimated to be 0.74%, 3.78%, and 2.67% in men aged 19–44, 45–64, and 65+ years old, respectively (2). Additionally, SUI is one of the most common side effects after radical prostatectomy (RP) with several large series demonstrating an incidence of 6–8% (3,4). While 56% of patients with SUI experience symptom resolution by 12 months following RP (5-7), up to 16% of patients experience persistent post-prostatectomy SUI, and some patients may experience urinary incontinence as a late complication of this procedure (8). SUI can have a devasting effect on mental well-being and quality of life (QOL), with this effect being more pronounced in men (9-12). In fact, some studies suggest that urinary function is the single strongest predictor of patient health-related QOL after RP (7,13). Considering the significant morbidity associated with urinary incontinence as well as the relatively high prevalence of SUI in those undergoing urologic procedures, many patients may elect surgical treatment to address their urinary incontinence.
The most common indication of surgical intervention for SUI in males is after radical prostatectomy (RP) due to intrinsic sphincter deficiency (14). Surgical therapy with artificial urinary sphincter (AUS) or male sub-urethral slings (MS) is the current standard treatment in men with SUI who fail or are not interested in conservative management (15). Both AUS and MS have been shown to improve QOL, with AUS placement being the most effective long-term treatment for men with severe SUI (16,17). However, MS is an alternative treatment option for SUI in patients with limited manual dexterity who would have difficulty manipulating an AUC, or in men with milder SUI, particularly, if there is no history of prior radiation (15). Nonetheless, elective surgical procedures are associated with significant costs and therefore, the financial burden of these procedures may limit the access of uninsured or underinsured patients, especially in light of the COVID-19 pandemic (18,19).
The Affordable Care Act (ACA) significantly changed the access to healthcare for many Americans when it was passed in 2010. One component of the ACA involved increasing income eligibility for individuals with an income 138% of the federal poverty line (20). As of 2021, 38 out of 50 states have adopted Medicaid expansion (21). With the improvement in Medicaid coverage, access to elective surgery has been shown to increase within the orthopedic literature (22). Additionally, Mesquita-Neto et al. found that following Medicaid expansion, cancer patients were diagnosed at an earlier stage and had improved access to surgical care (20). Accordingly, as more men are diagnosed with and treated for prostate cancer and other pelvic malignancies, there will likely be a need for a number of these men to be treated for SUI.
Barnard et al. recently reported that the Medicaid coverage of malleable penile prostheses (MPP) and inflatable penile prostheses (IPP) varied from state to state (23). To the best of our knowledge, there are no reports on the Medicaid coverage of SUI-related surgeries despite the increasing popularity of these treatments. With a growing number of Medicaid patients undergoing surgery for pelvic malignancies, there is a need to better understand the coverage of SUI-related surgeries for this patient population. Consequently, we sought to determine the state-by-state Medicaid coverage of AUS and MS.
Methods
State Medicaid websites were utilized to access publicly available physician fee schedules for the calendar year 2020. The fee schedules were subsequently searched for current procedural terminology (CPT) codes. The CPT codes 53444, 53445, 53446, and 53447 were used for AUS tandem cuff, AUS insertion, AUS removal, and AUS revision, respectively. Similarly, the CPT codes 53440 and 53442 were used for MS placement and revision, respectively. Individual search queries were performed for each CPT code, and coverage status, as well as physician fee reimbursement amount, were recorded. The median and range for physician fees were determined for each CPT code.
Statistical analysis
Student’s t-test was utilized to compare the mean physician reimbursements for states which have adopted Medicaid expansion under the ACA to those states which have not adopted Medicaid expansion (AL, FL, GA, KS, MS, NC, TX, SC, SD, WY, WI). TN has not adopted Medicaid expansion; however, their reimbursement rates were not publicly available so they were excluded from this analysis.
Results
Coverage by the state
Of the 50 states analyzed, 49 published publicly accessible physician fee schedules. The state of Tennessee subcontracts to several insurance agencies, and therefore, Medicaid fee-for-service data could not be obtained as all of these agencies require a patient claim to be submitted before making their data available for access. All 49 of the available states reported coverage for removal with and without revision of the AUS, and 48 states reported coverage for insertion of an AUS and insertion of a tandem cuff (Figure 1). Comparably, all 49 states reported coverage for placement of MS, and 48 states reported coverage for removal or revision of MS.
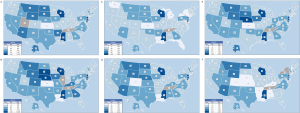
Utah did not report reimbursement for insertion of the tandem cuff, and the state of Illinois did not report reimbursement for AUS insertion. Finally, New York did not report reimbursement for MS revision.
Physician reimbursement
The median of physician reimbursement for each AUS related procedure was $624.00 ($181.84–$10,960.90) for tandem cuff, $665.54 ($199.89–$11,949.86) for AUS insertion, $528.03 ($146.90–$1,893.12) for AUS removal, and $630.29 ($208.55–$11,586.74) for AUS revision.
The median of physician reimbursement was $652.57 ($198.00–$5,237.35) for MS placement and $554.47 ($104.27–$2,288.93) for MS revision. Mississippi reported the highest reimbursement for all surgeries related to AUS and MS with the exception of AUS removal, which was highest in Delaware. Kansas reported the lowest reimbursement for AUS insertion, AUS removal, tandem cuff placement, and MS placement surgeries. Colorado reported the lowest reimbursement for AUS revision and MS revision surgeries (Table 1, Table 2).
Table 1
| Procedure | Tandem cuff | Insertion | Removal | Revision |
|---|---|---|---|---|
| Current procedural terminology code | 53444 | 53445 | 53446 | 53447 |
| State | ||||
| AL | $495.00 | $712.00 | $453.00 | $680.00 |
| AK | $898.08 | $669.85 | $669.85 | $669.85 |
| AZ | $841.06 | $798.61 | $679.53 | $856.09 |
| AR | $860.13 | $713.35 | $796.19 | $590.87 |
| CA | $636.26 | $634.03 | $595.31 | $591.21 |
| CO | $577.66 | $852.58 | $535.95 | $208.55 |
| CT | $469.01 | $521.36 | $380.91 | $484.04 |
| DE | $2,334.30 | $2,320.92 | $1,893.12 | $2,384.51 |
| FL | $451.51 | $486.15 | $392.17 | $506.52 |
| GA | $724.22 | $857.33 | $674.81 | $708.62 |
| HI | $560.48 | $774.74 | $526.92 | $633.87 |
| ID | $697.21 | $661.22 | $563.45 | $710.52 |
| IL | $540.40 | – | $494.90 | $449.50 |
| IN | $575.55 | $545.80 | $465.11 | $586.64 |
| IA | $712.91 | $908.00 | $654.46 | $755.72 |
| KS | $181.84 | $199.89 | $146.90 | $623.48 |
| KY | $577.30 | $886.61 | $528.03 | $630.29 |
| LA | $483.29 | $360.84 | $360.84 | $360.84 |
| ME | $543.40 | $599.43 | $437.64 | $554.37 |
| MD | $631.22 | $641.16 | $511.72 | $643.95 |
| MA | $616.78 | $587.27 | $501.32 | $629.48 |
| MI | $458.21 | $436.81 | $371.64 | $466.33 |
| MN | $567.60 | $543.20 | $462.18 | $578.42 |
| MS | $10,960.90 | $11,949.86 | $1,581.02 | $11,586.74 |
| MO | $506.16 | $647.26 | $409.31 | $529.58 |
| MT | $925.17 | $877.91 | $747.25 | $941.48 |
| NE | $783.63 | $1,555.74 | $726.01 | $806.68 |
| NV | $736.02 | $699.78 | $596.59 | $751.09 |
| NH | $478.45 | $543.42 | $445.67 | $509.98 |
| NJ | $6,502.09 | $6,891.85 | $956.63 | $6,761.93 |
| NM | $720.56 | $716.28 | $574.10 | $742.30 |
| NY | $479.04 | $527.44 | $388.77 | $492.19 |
| NC | $695.72 | $767.61 | $560.67 | $709.94 |
| ND | $816.43 | $776.86 | $661.13 | $831.59 |
| OH | $550.59 | $660.13 | $507.15 | $584.30 |
| OK | $764.52 | $724.30 | $616.32 | $777.55 |
| OR | $573.00 | $547.19 | $465.70 | $583.62 |
| PA | $776.00 | $776.00 | $776.00 | $776.00 |
| RI | $430.34 | $707.84 | $398.35 | $382.31 |
| SC | $552.90 | $524.49 | $446.96 | $563.10 |
| SD | $803.44 | $1,161.37 | $648.29 | $785.93 |
| TN | – | – | – | – |
| TX | $612.66 | $612.66 | $495.32 | $623.62 |
| UT | – | $581.20 | $494.61 | $623.67 |
| VT | $662.40 | $630.14 | $536.36 | $674.53 |
| VA | $655.75 | $625.13 | $531.86 | $667.37 |
| WA | $463.82 | $441.22 | $375.62 | $472.22 |
| WV | $540.08 | $512.85 | $435.97 | $549.00 |
| WI | $1,097.28 | $1,097.28 | $1,097.28 | $1,097.28 |
| WY | $843.87 | $928.33 | $680.70 | $858.96 |
| Mean reimbursement | $1,007.59 | $1,087.40 | $596.93 | $1,020.14 |
| Maximum reimbursement | $10,960.90 | $11,949.86 | $1,893.12 | $11,586.74 |
| Minimum reimbursement | $181.84 | $199.89 | $146.90 | $208.55 |
Table 2
| Procedure | Placement | Revision |
|---|---|---|
| Current procedural terminology code | 53440 | 53442 |
| State | ||
| AL | $590.00 | $347.00 |
| AK | $898.08 | $669.85 |
| AZ | $797.86 | $829.79 |
| AR | $762.30 | $380.80 |
| CA | $744.60 | $462.02 |
| CO | $695.13 | $104.27 |
| CT | $505.11 | $444.73 |
| DE | $2,311.20 | $2,288.93 |
| FL | $484.39 | $490.91 |
| GA | $757.49 | $456.92 |
| HI | $684.87 | $416.54 |
| ID | $661.82 | $687.40 |
| IL | $599.35 | $449.50 |
| IN | $546.31 | $566.90 |
| IA | $801.98 | $486.54 |
| KS | $198.00 | $174.22 |
| KY | $723.37 | $397.99 |
| LA | $483.29 | $360.84 |
| ME | $597.38 | $525.62 |
| MD | $633.57 | $623.74 |
| MA | $585.94 | $610.80 |
| MI | $435.23 | $453.45 |
| MN | $539.43 | $563.83 |
| MS | $5,237.35 | $1,581.02 |
| MO | $550.58 | $484.58 |
| MT | $877.32 | $912.33 |
| NE | $1,152.40 | $374.53 |
| NV | $699.21 | $726.66 |
| NH | $531.48 | $396.45 |
| NJ | $3,080.06 | $956.63 |
| NM | $732.66 | $660.73 |
| NY | $521.18 | − |
| NC | $764.68 | $672.97 |
| ND | $774.64 | $806.81 |
| OH | $652.57 | $421.51 |
| OK | $724.77 | $752.50 |
| OR | $544.38 | $568.08 |
| PA | $776.00 | $776.00 |
| RI | $400.00 | $262.20 |
| SC | $524.84 | $545.11 |
| SD | $899.61 | $495.86 |
| TN | − | − |
| TX | $581.12 | $604.64 |
| UT | $581.28 | $603.87 |
| VT | $628.52 | $654.59 |
| VA | $622.86 | $648.95 |
| WA | $440.02 | $458.42 |
| WV | $512.85 | $532.37 |
| WI | $1,097.28 | $1,097.28 |
| WY | $934.44 | $823.38 |
| Mean reimbursement | $834.26 | $616.88 |
| Maximum reimbursement | $5,237.35 | $2,288.93 |
| Minimum reimbursement | $198.00 | $104.27 |
Reimbursement in states with Medicaid expansion
The mean physician reimbursement was less for AUS procedures in in states which had adopted Medicaid expansion compared to those states which had not adopted expansion ($773.76±$153.75 vs. $1,423.58±$171.80). However, this did not reach statistical significance P=0.08. There was also no statistically significant difference in reimbursement among sling procedures in states with Medicaid expansion and those without ($679.63±$184.81 vs. $879.93±$290.20, P=0.13).
Discussion
We found that almost all states provide Medicaid coverage for AUS and MS without the need for prior authorization. Of note, treatments with AUS and MS are considered optional, meaning that in contrast to mandatory benefits, these procedures are not required by the federal government to be covered by all states. MPP and IPP are also procedures that fall under the optional category. However, as discussed by Barnard et al., state Medicaid coverage of MPP and IPP showed that nearly half of states covered both devices and four states covered just one device with 11 states requiring prior authorization, and the remainder covered neither device (23). This is the first study to evaluate state Medicaid coverage of SUI treatments. We feel that our findings should empower surgeons in most states to offer surgical SUI management to more patients, regardless of insurance coverage, having confidence they will be reimbursed for their services.
Additionally, we found the mean physician reimbursement for AUS procedures in states which had not adopted Medicaid expansion to be almost twice as high ($1,423.58 vs. $773.76). However, this did not reach statistical significance since. The mean reimbursement for sling procedures was also greater in states without Medicaid expansion although there was a less drastic difference ($879.93 vs. $679.63). It is also interesting to note that the cost of living is less in most of the states which have not adopted Medicaid expansion which may further offset the cost differences in these two groups (24).
Approximately 90,000 RPs are performed annually in the United States, and more than 70% of robotic RPs are performed by surgeons who do fewer than 100 cases annually. Therefore, outcomes are often dependent on the experience and skill level of the operating surgeon (25,26). SUI is a relatively common and feared complication of RP by both patients and surgeons and can have devastating social and emotional consequences (8-12). Despite the near-ubiquitous Medicaid coverage of procedures aimed at treating SUI, it has been estimated that only 3.6% of men who have had an RP undergo surgical intervention for the management of SUI (27). This number is well below the reported 40% of patients with persistent bothersome urinary leakage following RP (28).
As a result, many patients with SUI who would presumably benefit from guideline-directed care may be undertreated (15). In fact, it has been previously demonstrated that AUS may be particularly underutilized in patients with post-proctectomy incontinence (29). This is especially alarming as AUS placement is demonstratively the most effective long-term treatment for men with severe SUI, with several large studies publishing success rates of complete continence (0 pad per day) ranging from 20% to 40%, social continence (0-1 pad per day) ranging from 59% to 90%, and patient satisfaction ranging from 73% to 90% (14). Success rates for MS, usually defined as greater than 50% improvement or 1-2 pads per day, are also reported to be between 40% and 88% and complete continence rates reported range from 9% to 75% (8).
A potential explanation for the discrepancy between the number of patients experiencing SUI who would otherwise benefit from surgical intervention and the number of patients seeking surgical treatment may be the lack of awareness regarding the coverage of such interventions. Accordingly, it can be surmised that treatment decisions made by physicians and Medicaid patients may be influenced by limited or inaccurate information on Medicaid coverage of AUS and MS procedures. As such, less effective and more conservative management strategies for treating SUI may be adopted instead of surgical interventions based upon the false presumption that surgical treatments may impose a more significant financial burden or may not reimburse urologic surgeons accordingly. Increasing access to information on Medicaid coverage of surgical management of SUI can allow a more thorough discussion of all the available treatment options without financial reservations from the patient and physician. It may also result in increased utilization of the most effective long-term management for male SUI and ultimately lead to increased patient satisfaction and QOL in a potentially underserved population. Further research is warranted to elucidate the association between the awareness of Medicaid coverage for AUS and MS and the rate of adoption of these surgical management strategies.
The results presented herein should be interpreted in view of the limitations of this study. Namely, the coding recorded within the physician fee schedule may not necessarily indicate successful coverage. However, given the infeasibility to obtain accurate approval rates on a state-by-state basis, the recorded coding within the physician fee schedule was presumed to have been covered successfully. Furthermore, even though there was near-universal coverage for male SUI-related surgeries, prior authorization requirements could not be assessed given the need to submit each patient’s claim, and as such, accurate information to patients seeking approval for AUS and MS surgeries cannot be provided. Lastly, considering the frequent modifications of fee schedules and Medicaid coverage, the data presented in this study may differ from the Medicaid coverage at the time of publication.
Conclusions
AUS and MS-related surgeries in the Medicaid population are covered by nearly all states as confirmed by publicly available data. Knowledge of Medicaid coverage for SUI-related surgery may result in increased utilization of these treatments for male SUI and improve access to care in the Medicaid cancer survivorship population.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-486/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003;61:37-49. [Crossref] [PubMed]
- Shamliyan TA, Wyman JF, Ping R, et al. Male urinary incontinence: prevalence, risk factors, and preventive interventions. Rev Urol 2009;11:145-65. [PubMed]
- Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA 2000;283:354-60. [Crossref] [PubMed]
- Sacco E, Prayer-Galetti T, Pinto F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int 2006;97:1234-41. [Crossref] [PubMed]
- Majoros A, Bach D, Keszthelyi A, et al. Urinary incontinence and voiding dysfunction after radical retropubic prostatectomy (prospective urodynamic study). Neurourol Urodyn 2006;25:2-7. [Crossref] [PubMed]
- Litwin MS, Melmed GY, Nakazon T. Life after radical prostatectomy: a longitudinal study. J Urol 2001;166:587-92. [Crossref] [PubMed]
- Trofimenko V, Myers JB, Brant WO. Post-Prostatectomy Incontinence: How Common and Bothersome Is It Really? Sex Med Rev 2017;5:536-43. [Crossref] [PubMed]
- Welk BK, Herschorn S. The male sling for post-prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int 2012;109:328-44. [Crossref] [PubMed]
- Cheng MC, Liu SP, Chuang YC, et al. Prevalence and impacts of male urinary incontinence on quality of life, mental health, work limitation, and health care seeking in China, Taiwan, and South Korea (LUTS Asia): Results from a cross-sectional, population-based study. Investig Clin Urol 2022;63:71-82. [Crossref] [PubMed]
- Coyne KS, Kvasz M, Ireland AM, et al. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol 2012;61:88-95. [Crossref] [PubMed]
- Tennstedt SL, Chiu GR, Link CL, et al. The effects of severity of urine leakage on quality of life in Hispanic, white, and black men and women: the Boston community health survey. Urology 2010;75:27-33. [Crossref] [PubMed]
- Lagro-Janssen TA, Hilkens CJ, Klaasen RI, et al. Greater emotional and social effect of urinary incontinence in men than women. J Am Geriatr Soc 2008;56:1779-81. [Crossref] [PubMed]
- Khanna D, Tsevat J. Health-related quality of life--an introduction. Am J Manag Care 2007;13:S218-23. [PubMed]
- James MH, McCammon KA. Artificial urinary sphincter for post-prostatectomy incontinence: a review. Int J Urol 2014;21:536-43. [Crossref] [PubMed]
- Sandhu JS, Breyer B, Comiter C, et al. Incontinence after Prostate Treatment: AUA/SUFU Guideline. J Urol 2019;202:369-78. [Crossref] [PubMed]
- Bauer RM, Grabbert MT, Klehr B, et al. 36-month data for the AdVance XP® male sling: results of a prospective multicentre study. BJU Int 2017;119:626-30. [Crossref] [PubMed]
- Boswell TC, Elliott DS, Rangel LJ, et al. Long-term device survival and quality of life outcomes following artificial urinary sphincter placement. Transl Androl Urol 2020;9:56-61. [Crossref] [PubMed]
- Billig JI, Lan WC, Chung KC, et al. The Increasing Financial Burden of Outpatient Elective Surgery for the Privately Insured. Ann Surg 2020;272:530-6. [Crossref] [PubMed]
- Lin JA, Braun HJ, Schwab ME, et al. Pandemic Recovery: Persistent Disparities in Access to Elective Surgical Procedures. Ann Surg 2021; Epub ahead of print. [Crossref] [PubMed]
- Mesquita-Neto JWB, Cmorej P, Mouzaihem H, et al. Disparities in access to cancer surgery after Medicaid expansion. Am J Surg 2020;219:181-4. [Crossref] [PubMed]
- Kaiser Family Foundation: Status of State Medicaid Expansion Decisions: Interactive Map [Internet]. 2021 Nov 5. [Cited 8 Nov 2021] Available online: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
- Williamson TR, Paoli AR, Hutzler L, et al. Access to Elective Orthopaedic Surgery After the Affordable Care Act Medicaid Expansion: The New York State Experience. J Am Acad Orthop Surg 2020;28:e158-63. [Crossref] [PubMed]
- Barnard JT, Grimaud L, Yafi FA. Does Medicaid Cover Penile Prosthesis Surgery? A State-by-State Analysis. J Sex Med 2021;18:1455-60. [Crossref] [PubMed]
- Composite cost of living index in the different states in the United States as of 2020 [Internet]. 2022 Aug 18. [Cited 19 Aug 2022]. Available online: https://www.statista.com/statistics/1240947/cost-of-living-index-usa-by-state/
- Lowrance WT, Eastham JA, Savage C, et al. Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. J Urol 2012;187:2087-92. [Crossref] [PubMed]
- Carson CC. Artificial urinary sphincter: current status and future directions. Asian J Androl 2020;22:154-7. [Crossref] [PubMed]
- Nelson M, Dornbier R, Kirshenbaum E, et al. Use of Surgery for Post-Prostatectomy Incontinence. J Urol 2020;203:786-91. [Crossref] [PubMed]
- Singla N, Singla AK. Post-prostatectomy incontinence: Etiology, evaluation, and management. Turk J Urol 2014;40:1-8. [Crossref] [PubMed]
- Reynolds WS, Patel R, Msezane L, et al. Current use of artificial urinary sphincters in the United States. J Urol 2007;178:578-83. [Crossref] [PubMed]


