Laser hair removal for genital gender affirming surgery
Introduction
Genital gender affirming surgery (GAS) involves reconstruction of the genitals to match a patient’s identified sex. The use of hair-bearing flaps in this procedure may result in postoperative intra-vaginal and intra-urethral hair growth (1). This undesirable side effect is associated with irritation, infections, hairball and calculi formation, and ultimately a lower patient satisfaction with genital GAS (2-4). Because genital GAS aims to treat gender dysphoria—a condition diagnosed and deemed treated by self-reports (5-7) —addressing patient satisfaction is critical.
To prevent the unwanted hair growth and associated complications, genital GAS has become a recognized indication for hair removal (3,8). However, even with the significant increase in incidence of genital GAS within the past 50 years (9,10), there is limited data regarding hair removal practices in preparation for genital GAS and notable variation in hair removal techniques among practitioners. Consolidation of the limited literature can help guide the implementation of standardized care. To this end, we present a practical approach to hair removal prior to genital GAS. Modern hair removal techniques and a review of the literature provide context for our recommendations.
Hair removal techniques
Hair removal has advanced from physical methods of shaving, plucking, and waxing to the more technologically sophisticated techniques of electrolysis and laser hair removal (LHR) (11,12). While no technique achieves 100% permanent removal of all unwanted hair, electrolysis and LHR are the preferred treatments for permanent removal because of their higher efficacy. Surgeons performing genital GAS require preoperative permanent hair removal from any skin area that will either be brought into contact with urine (e.g., used to construct a neourethra) or be moved to reside within a partially closed cavity within the body (e.g., used to line the neovagina) (13-15). Hair within a neourethra will obstruct urine outflow, promote urine retention within the urethra, and often become encrusted with stone and sebaceous debris—all of which increase the risk of urinary infections and post-void dribbling of urine. Hair within the neovagina serves as a nidus for infection and encrustation of debris. Hair bearing skin that remains outside of the body after GAS does not need to be removed (Table 1).

Full table
Prior to the advent of LHR, electrolysis was the predominant method used for removal of unwanted hair. Electrolysis is the process of electric epilation, in use since 1875 and approved by the FDA for permanent hair removal (16,17). It involves the insertion of a fine needle or probe into each hair follicle for delivery of an electric current in attempt to destroy the follicular unit responsible for hair regeneration (17). Hair reductions up to 90% have been reported; however, the treatment efficacy is highly variable and operator- and modality-dependent, with regrowth ranging from 15–50% (16,18). Because each hair follicle must be treated individually, multiple hours of treatment on a weekly or biweekly basis for up to a year are generally required for best results (17,19).
LHR is an FDA-approved form of permanent hair reduction rather than permanent hair removal. The distinction between hair removal and reduction is mechanistic: LHR does not reduce the number of hair follicles, as electrolysis does, but rather reduces the number of hairs by damaging the follicular bulb while leaving the follicle intact. The mechanism of action of LHR is based on selective photothermolysis: laser light selectively targets melanin in the hair shaft, leading to destruction of the follicular epithelium (20). LHR can be performed with ruby, alexandrite, diode, and neodymium:yttrium aluminum garnet (Nd:YAG) lasers and intense pulsed light (IPL) sources, which operate at different wavelengths suitable for varying skin types and indications (21). Since the first FDA approval of LHR in 1995, LHR has become the fastest growing procedure in cosmetic dermatology, spread to several home-based devices, and demonstrated the longest hair-free period for removal of unwanted hair (12,21,22).
LHR has significant benefits over electrolysis, though studies with long-term follow-up are limited (23). Alexandrite-LHR provides higher clearance rates than electrolysis (74% vs. 35%, respectively) 6 months following treatment, is 60 times faster and less painful, and requires fewer treatment sessions (24). Electrolysis may be cheaper per session, but many hours may be required to treat each area of hair; in contrast, LHR will treat the entire area for hair removal during each session with faster procedure times, low occurrence of side effects, and fewer needed sessions (25). In addition, a Cochrane systematic review of 30 controlled trials concluded that efficacy of LHR is superior to that of electrolysis (23,26).
Hair removal prior to genital GAS
Although the literature on hair removal prior to genital GAS is limited, electrolysis has been commonly used for this indication, as it had been the sole solution for long-term hair removal before the advent of LHR (2,3,13,27,28). Reliance on this practice has persisted in public and professional transgender health care forums, despite the absence of evidence-based clinical guidelines or peer reviewed data to support favoring electrolysis over LHR.
However, more recent studies specific to genital GAS support the use of LHR over electrolysis in this setting. A follow-up study of 232 patients who had undergone electrolysis before genital GAS found that those who underwent preoperative genital electrolysis did not report a reduction in postoperative vaginal hair complications compared to those who were not treated (3). On the other hand, a recent case report of long-pulsed alexandrite LHR on scrotal skin prior to genital GAS demonstrated no intra-vaginal hair growth at 15 months following vaginoplasty (27). Several case reports have also described the use of LHR for removal of urethral hair following hypospadias and stricture repair with minimal side effects and satisfactory outcomes up to 1 year following LHR (29-33).
A proposed approach for preoperative genital LHR
The shift towards LHR as a superior method of hair removal suggests that it should also be the treatment of choice prior to genital GAS. Based on the literature as well as from our own experience, we present the following recommendations specifically for hair removal prior to genital GAS.
Preoperative evaluation: treatment planning and management of expectations
The majority of transgender patients, unfortunately, report that they have experienced discrimination when seeking health services. During preoperative evaluation, practitioners of LHR should be attentive to using correct pronouns for each patient. We recommend that practitioners simply ask what pronouns a patient prefers. Some patients may not have had their name legally changed at the time of evaluation so asking patients their preferred name is also recommended.
LHR practitioners should confirm with patients that they have reviewed with their GAS surgeon which (if any) areas of their genitalia and flap donor sites should be rendered hair-free before surgery. Given the delay to surgery and costs that hair removal can create for patients, unnecessary hair removal should be avoided. Ideally, there can be direct communication between the GAS surgeon and treating dermatologist. In our experience, it is useful for the GAS surgeon to use a permanent ink-marking pen to outline the area to be made hair-free before the patient presents for hair removal. A photograph of this outlined area can also be useful during each treatment to ensure the correct area is being targeted.
Realistic patient expectations should be established, detailing potential adverse outcomes. The mean socio-economic status of transgender patients is lower than that of non-transgender patients, and thus, affordability may be a substantial issue for many patients. The anticipated out-of-pocket costs to the patient and the likely number of treatments needed should be established before treatment (while LHR is not often covered by insurance, some companies cover LHR prior to genital GAS). Patients should be informed that each treatment will target existing hair bulbs, but that resting (telogen) follicles will grow hairs in between treatments until all the follicles have been treated. Patients should be aware that, in some cases, hair may regrow years later—though late onset hair regrowth is generally more sparse, thinner, and paler (21). LHR achieves best results for dark hair on light skin, as it targets the melanin in the hair bulb. Patients with darker skin should be treated with longer wavelength lasers to protect the epidermis (34). For these same reasons, LHR is not suitable for blond or white hair, and patients with these features should be directed to undergo electrolysis instead. Although home laser units are now available, patients should be advised that the process is significantly more time consuming and may not yield the same results.
Preparation before LHR
Hair should be shaved prior to LHR to ensure that the melanin of the dermal hair bulb absorbs the laser energy without interference from melanin of hair above the epidermal surface. Shaving hair prior to LHR has been demonstrated to improve the efficacy of laser transmission and the mechanism of selective thermolysis (35). Any plucking, waxing, electrolysis, or other methods that remove the hair bulb should be avoided for at least 4 weeks before LHR because an intact bulb is the chromophore necessary to achieve selective photothermolysis (21,36). Patients should adhere to strict sun avoidance for a minimum of 6 weeks before and after each treatment because any tanning limits treatment efficacy and increases the risk of side effects, such as dyspigmentation (21). Further, patients taking minoxidil (or with partners using the topical agent) should be advised that the stimulating effects of the drug may disrupt hair removal (37).
Anesthesia
Topical anesthetic pretreatment includes 30-minute to 1-hour incubation with creams, such as lidocaine, prilocaine, or tetracaine (21). Tetracaine has been documented in use for LHR of scrotal skin (27). The use of a cooling fan or device may provide comfort during the procedure, and ice can be applied immediately afterwards. Topical steroids can be used following treatment to reduce redness and swelling.
Area of hair removal
Areas of hair removal for genital GAS can include the forearm, anterior thigh, and scrotum. The surgeon should always confirm with the patient and, whenever possible, the treating dermatologist exactly which area should be rendered hair-free before surgery.
Male-to-female (MtF) genital GAS
Creation of a vulva (vaginoplasty) can include or not include creation of a vaginal cavity. Vaginoplasty without creation of a neovaginal cavity generally does not require any hair removal preoperatively, as any hair-bearing skin will be visible and easily accessible after surgery. Vaginoplasty with creation of a neovaginal cavity requires that the penile shaft skin be made hair-free because with the most common vaginoplasty technique (penile inversion vaginoplasty), the penile shaft skin is used to line the vaginal cavity and will be out of reach for hair removal procedures after surgery (38). Some transgender women undergoing vaginoplasty with vaginal cavity formation may require harvest of scrotal skin for use to line the vaginal cavity. If the surgeon plans to use a pedicled scrotal skin flap, the anterior midline face of the scrotum is dissected but left in continuity with the perineum at midline proximally. The distal end (closest to the base of the penile shaft) is sutured to the end of the penile shaft skin (detubularized along the dorsal midline). The lateral edges of both flaps are sutured together to form a tube, lined on the inside by penile and scrotal skin epithelium. For this, a 10 cm-wide midline vertical strip of scrotal skin extending from the scrotal-perineal junction (proximally) to the base of the penis (distally) should be permanently cleared of hair growth (Figure 1A).
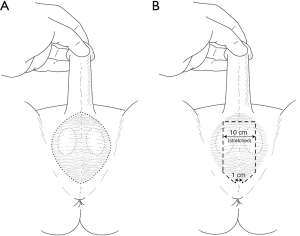
Some surgeons choose to use a portion of excess scrotal skin (normally discarded during the surgery) as a full-thickness free skin graft to augment the length of intact (i.e., still tubularized) penile shaft skin. In such cases, it is difficult to pre-determine exactly which areas of scrotal skin will be used, and it is safest to treat the entire scrotum for permanent hair removal (Figure 1B). Perineal skin never needs to be treated for hair removal preoperatively.
Female-to-male (FtM) genital GAS
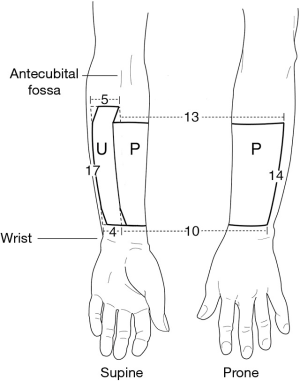
Only transgender men undergoing phalloplasty with urethral lengthening (construction of a neourethra) require preoperative permanent hair removal. The skin-flap area that will be used to construct the neourethra must be rendered free of hair-growth to avoid hair-related complications. Residual hair on the skin that will be used to make the phallus shaft need not be treated, as it is easily accessible for treatment post-op. Skin for phalloplasty with urethral lengthening is commonly harvested from the forearm radial artery (forearm flap) phalloplasty (RAP) (39) or the anterolateral thigh [(ALT) flap phalloplasty] (40-42). With RAP, the skin used for construction of the neourethra is ~5 cm wide and harvested from the medial aspect of the ventral face of the forearm (Figure 2). For RAP, we recommend hair removal of the medial aspect of the entire ventral forearm.
With ALT flap phalloplasty, the skin area used to construct the neourethra can be harvested from the medial or lateral aspect of the same flap template as is used with RAP. The flap is located on the anterolateral surface of the thigh, centered slightly distal or proximal to the halfway point between the anterior superior iliac crest (proximally) and the lateral aspect of the patella (distally) (Figure 3). The exact location of the skin area to be used in ALT flap phalloplasty is less predictable, as the surgical margins vary with the vasculature to the flap area. Generally speaking, the entire flap area lies within the middle 2/3 of the ALT. We recommend that patients undergoing ALT flap phalloplasty ask their surgeon to specify exactly what area should be rendered hair-free before the patient commences hair removal treatments.

Laser settings
The laser to be used should be a long-pulsed laser with a wavelength appropriate to target melanin, such as a diode, alexandrite, or long-pulsed Nd:YAG. Selection of laser wavelength should take the patient’s skin color into account, and the fluence, pulse duration, and cooling should be optimized to achieve immediate destruction of the bulb with perifollicular erythema, while protecting the epidermis from thermal injury. Selection of laser settings requires training in the use of these devices. The American Society for Dermatologic Surgery recommends that LHR be practiced only in an appropriate setting by, or under the direct supervision of, a physician.
Number of treatments
An evidence-based review reported that multiple LHR treatments result in increased efficacy of hair removal (22,26,43). The European Society for Laser Dermatology recommends three to eight LHR treatments (36), and the American Academy of Dermatology states that most patients need between two to six treatments. Treatments, which may each take up to 30 minutes, should be spaced at least 6 weeks apart to allow for hair cycling. Our experience with genital GAS is that it is best to wait 3 months after the last planned hair removal treatment before proceeding with surgery, in order to confirm that no further hair regrowth will occur.
Conclusions
Despite long experience with electrolysis for hair removal prior to GAS, evidence-based outcomes studies have shown LHR to be the superior modality. LHR has largely supplanted electrolysis for permanent hair removal in the medical setting. We present a practical approach to LHR for genital GAS, which will inform future studies needed to develop evidence-based guidelines for best practice in the field.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Selvaggi G, Bellringer J. Gender reassignment surgery: an overview. Nat Rev Urol 2011;8:274-82. [Crossref] [PubMed]
- Bowman C, Goldberg JM. Care of the Patient Undergoing Sex Reassignment Surgery. Int J Transgend 2006;9:135-65. [Crossref]
- Lawrence AA. Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Arch Sex Behav 2006;35:717-27. [Crossref] [PubMed]
- Fang RH, Kao YS, Ma S, et al. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br J Plast Surg 1999;52:217-22. [Crossref] [PubMed]
- Cohen-Kettenis PT, Gooren LJ. Transsexualism: a review of etiology, diagnosis and treatment. J Psychosom Res 1999;46:315-33. [Crossref] [PubMed]
- Green R, Fleming DT. Transsexual Surgery Follow-Up: status in the 1990s. Annu Rev Sex Res 1990;1:163-74.
- Kuiper B, Cohen-Kettenis P. Sex reassignment surgery: a study of 141 Dutch transsexuals. Arch Sex Behav 1988;17:439-57. [Crossref] [PubMed]
- Liew SH. Unwanted body hair and its removal: a review. Dermatol Surg 1999;25:431-9. [Crossref] [PubMed]
- Dhejne C, Öberg K, Arver S, et al. An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Arch Sex Behav 2014;43:1535-45. [Crossref] [PubMed]
- Arcelus J, Bouman WP, Van Den Noortgate W, et al. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry 2015;30:807-15. [Crossref] [PubMed]
- Shapiro J, Lui H. Treatments for unwanted facial hair. Skin Therapy Lett 2005-2006;10:1-4. [PubMed]
- Fernandez AA, França K, Chacon AH, et al. From flint razors to lasers: a timeline of hair removal methods. J Cosmet Dermatol 2013;12:153-62. [Crossref] [PubMed]
- Reed HM. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin Plast Surg 2011;25:163-74. [Crossref] [PubMed]
- Trombetta C. My Personal Technique. In: Trombetta C, Liguori G, Bertolotto M, editors. Management of Gender Dysphoria. Milan: Springer Milan,2015:93-104.
- Goddard JC, Vickery RM, Qureshi A, et al. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int 2007;100:607-13. [Crossref] [PubMed]
- Pickens JE, Zakhireh M. Permanent removal of unwanted hair. Aesthet Surg J 2004;24:442-5. [Crossref] [PubMed]
- Richards RN, Meharg GE. Electrolysis: observations from 13 years and 140,000 hours of experience. J Am Acad Dermatol 1995;33:662-6. [Crossref] [PubMed]
- Wagner RF Jr. Physical methods for the management of hirsutism. Cutis 1990;45:319-21, 325-6. [PubMed]
- Richards RN, McKenzie MA, Meharg GE. Electroepilation (electrolysis) in hirsutism. 35,000 hours' experience on the face and neck. J Am Acad Dermatol 1986;15:693-7. [Crossref] [PubMed]
- Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 1983;220:524-7. [Crossref] [PubMed]
- Gan SD, Graber EM. Laser hair removal: a review. Dermatol Surg 2013;39:823-38. [Crossref] [PubMed]
- Lepselter J, Elman M. Biological and clinical aspects in laser hair removal. J Dermatolog Treat 2004;15:72-83. [Crossref] [PubMed]
- Haedersdal M, Gøtzsche PC. Laser and photoepilation for unwanted hair growth. Cochrane Database Syst Rev 2006.CD004684. [PubMed]
- Görgü M, Aslan G, Aköz T, et al. Comparison of alexandrite laser and electrolysis for hair removal. Dermatol Surg 2000;26:37-41. [Crossref] [PubMed]
- Lanigan SW. Incidence of side effects after laser hair removal. J Am Acad Dermatol 2003;49:882-6. [Crossref] [PubMed]
- Haedersdal M, Wulf HC. Evidence-based review of hair removal using lasers and light sources. J Eur Acad Dermatol Venereol 2006;20:9-20. [Crossref] [PubMed]
- Koch D, Pratsou P, Szczecinska W, et al. The diverse application of laser hair removal therapy: a tertiary laser unit's experience with less common indications and a literature overview. Lasers Med Sci 2015;30:453-67. [Crossref] [PubMed]
- Hage JJ, Bouman FG, Bloem JJ. Preconstruction of the pars pendulans urethrae for phalloplasty in female-to-male transsexuals. Plast Reconstr Surg 1993;91:1303-7. [Crossref] [PubMed]
- Beiko D, Pierre SA, Leonard MP. Urethroscopic holmium:YAG laser epilation of urethral diverticular hair follicles following hypospadias repair. J Pediatr Urol 2011;7:231-2. [Crossref] [PubMed]
- Singh I, Hemal AK. Recurrent urethral hairball and stone in a hypospadiac: management and prevention. J Endourol 2001;15:645-7. [Crossref] [PubMed]
- Crain DS, Miller OF, Smith L, et al. Transcutaneous laser hair ablation for management of intraurethral hair after hypospadias repair: initial experience. J Urol 2003;170:1948-9. [Crossref] [PubMed]
- Kaneko T, Nishimatsu H, Ogushi T, et al. Laser hair removal for urethral hair after hypospadias repair. Nihon Hinyokika Gakkai Zasshi 2008;99:35-8. [Crossref] [PubMed]
- Finkelstein LH, Blatstein LM. Epilation of hair-bearing urethral grafts utilizing the neodymium:YAG surgical laser. Lasers Surg Med 1990;10:189-93. [Crossref] [PubMed]
- Sadighha A, Mohaghegh Zahed G. Meta-analysis of hair removal laser trials. Lasers Med Sci 2009;24:21-5. [Crossref] [PubMed]
- Mustafa FH, Jaafar MS. Shaving area of unwanted hair before laser operation is useful in cosmetic procedure: A simulation study. Journal of Dermatology & Dermatologic Surgery 2015;19:36-42. [Crossref]
- Drosner M, Adatto M; European Society for Laser Dermatology. Photo-epilation: guidelines for care from the European Society for Laser Dermatology (ESLD). J Cosmet Laser Ther 2005;7:33-8. [PubMed]
- Vejjabhinanta V, Nouri K, Singh A, et al. Laser for Hair Removal. In: Nouri K, editor. Lasers in Dermatology and Medicine. Springer London, 2012:91-101.
- Edgerton MT, Bull J. Surgical construction of the vagina and labia in male transsexuals. Plast Reconstr Surg 1970;46:529-39. [Crossref] [PubMed]
- Chang TS, Hwang WY. Forearm flap in one-stage reconstruction of the penis. Plast Reconstr Surg 1984;74:251-8. [Crossref] [PubMed]
- Felici N, Felici A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J Plast Reconstr Aesthet Surg 2006;59:153-7. [Crossref] [PubMed]
- Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg 1984;37:149-59. [Crossref] [PubMed]
- Wei FC, Jain V, Celik N, et al. Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg 2002;109:2219-26; discussion 2227-30. [Crossref] [PubMed]
- Casey AS, Goldberg D. Guidelines for laser hair removal. J Cosmet Laser Ther 2008;10:24-33. [Crossref] [PubMed]


