Penile traction therapy for Peyronie’s disease—what’s the evidence?
Introduction
Peyronie’s Disease (PD) is manifested by the development of a fibrous inelastic scar within the tunica albuginea, which can lead to penile deformity, penile curvature, shrinkage, narrowing, hinging, shortening, and painful erections. These symptoms subsequently cause painful and/or unsatisfying sexual intercourse (1-7).
Treatment options range from reassurance to medical, mechanical, and surgical options (1). Medical treatment options for PD are used to treat patients in the early/acute phase of the disease. Although several reports in the literature exist of penile curvature stabilization and/or improvement in other clinical symptoms, recent guidelines describe that the available evidence reveals no significant benefit from common medical treatment options, especially for reducing penile curvature (3). On the other hand, according to the recent therapy guidelines, medical treatment options including either oral or intralesional injection therapy have been widely accepted as the standard of care at the first presentation of men with PD (8). In addition to oral and intralesional injection therapy, several authors have also used other non-surgical treatment modalities to treat patients with PD, including topical therapy, extracorporeal shockwave therapy, iontophoresis, and penile traction therapy (PTT) (1-4). PTT, which produces gradual mechanical traction to the penis, has been described as an efficient, nonsurgical treatment option for men with PD. It has been suggested that application of PTT results in an enhancement in the length of the penis in both erect and flaccid forms (6,7).
In this article, we aim to review the current literature regarding the use of PTT in men with PD, and, additionally, its use in specific patient subgroups, including men with shortened penis prior to penile prosthesis placement.
Penile traction therapy (PTT) and Peyronie’s disease (PD):
Experimental data
Several studies have revealed that there are many similarities between PD and Dupuytren’s contracture (5,9). The most important finding was that several genes associated with collagen degradation, such as matrix metalloproteinases and those related to myofibroblast differentiation, were similar in both diseases, suggesting that the two conditions may share a common pathophysiological pathway (5,10). Therefore, investigators suggested that both conditions may potentially respond to similar therapeutic modalities (5). It has been previously shown that the use of mechanical traction and tissue expansion therapy leads to an alteration of connective tissue by cellular proliferation and expansion of the extracellular matrix (5). Tissue traction, or the use of tension to evoke a biologic response, has been investigated in numerous other clinical conditions and in several disciplines. The mechanism, namely “mechanotransduction”, has been described as a process that converts mechanical stimuli to cellular biochemical responses (5). Although the concept of ‘tissue traction therapy’ had not been studied in the penis or PD models until the early 2000s, the biochemical response to tissue traction has previously been investigated in skin, bone, skeletal muscle and Dupuytren’s models (11-14). In Dupuytren’s contracture, a pro-fibrotic clinical condition similar to PD, continuous and prolonged mechanical tension on the fibrotic tissue may cause collagen remodeling and tendon healing (15). Additionally, histological staining studies have shown that, after traction therapy, there is reorganization and remodeling of collagen fibers into uniform, densely packed fibrils that are parallel to the axis of mechanical strain (16). Chung et al. performed the first experimental study related to the efficacy of tissue traction therapy in PD in a rigorously designed model (5). Briefly, using a cyclic strain culture system, the authors investigated the cellular changes to the tunical tissue following equibiaxial traction forces. The authors hypothesized that the observed protein alteration following mechanical traction should replicate the changes seen in tunical tissue following PTT. In this study, both qualitative [immunohistochemistry (IHC)] and quantitative (Western Blot assay) measurements were examined, hence increasing the value and reliability of the study. The results of this excellent study revealed that there was a significant increase in smooth muscle α-actin, β-catenin, and Hsp-47 protein contents measured in PD patients, as compared with the control group. Changes in IHC and Western immunoblot assays were seen after exposure to cellular equibiaxial tractional forces. IHC staining revealed a decrease in α-actin staining while Western Blot assay showed a prominent increase in metalloproteinase-8 expression with no measured change in β-catenin level in the stained PD group (5). This interesting study of cells obtained from PD and normal human tunica albuginea cultured in a mechanical strained environment provided important and promising evidence for the use of PTT in men with PD for plaque remodeling. Evidence obtained from these basic science experiments lends support to the clinical use of PTT. It is expected that PTT use in PD should yield similar outcomes as those seen with Dupuytren’s disease or any other similar clinical conditions.
Clinical data
There are several commercially available penile stretching or traction devices for PD, including FastSize Penile Extender device (FastSize Medical, Aliso Viejo, CA, USA), Andro-Penis (Andromedical, Madrid, Spain), Golden Erect extender device (Ronas Tajhiz Teb, Tehran, Iran), SizeGenetics (GRT Net Services Inc., Gresham, OR, USA), Vimax Extender (OA Internet Services, Montreal, Canada) and ProExtender (Leading Edge Herbals, Greeley, CO, USA). These devices consist of parallel rods connected to two padded rings, one proximally at the base of the penis and a second distally underneath the corona. PTT is performed by holding the penis in a small frame and applying a gentle, but progressive, traction force on it, which can be accomplished by the addition of small metal extensions to the parallel dynamic rods and frame for certain time periods (5,7). Available data related to PTT treatment is summarized in Table 1.
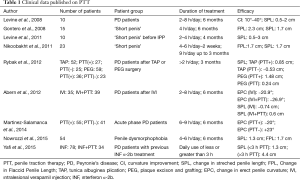
Full table
The first report for the use of PTT in men with PD was presented at the 4th annual meeting of the European Society for Sexual and Impotence Research (ESSIR) in 2001. In this small study, eight men with at least a 3 months history of PD without ED underwent PTT for 4 h per day for a total of 3–6 months. The authors reported a 4.1-cm increase in mean penile length (P˂0.05) and a 14° decrease in mean erect penile deviation (from 34° to 20°; P˂0.05) in this series (17).
Levine et al. evaluated the efficacy of prolonged external PTT as a nonsurgical treatment option in 10 men with PD. In this non-controlled pilot study of PTT, patients were treated using the FastSize penile extender. Traction was applied as the only treatment for 2–8 h per day for 6 months. Penile curvature, and stretched penile length and girth were measured before and after treatment. Additionally, erectile and sexual function was assessed using the International Index of Erectile Function-5 (IIEF-5) and Quality of Life Specific to Male Erection Difficulties (QOL-MED) questionnaires. At the end of the study, all men reported reduced curvature (10–40°), increased penile length (1–2.5 cm), and increased erect penile girth (0.5–1 cm), with correction of hinge effect in four out of four men. However, there was no significant change in quality of life by QOL-MED in this series. The authors of this pilot study concluded that, even though the study included small number of patients, early results suggested that prolonged daily use of PTT treatment should be considered as a new approach for the nonsurgical treatment of PD. Additionally, the authors noted the need for further well designed, randomized studies with larger numbers of patients (18).
One year later, Gontero et al. (19) reported the results of PTT use in men with a minimum of 12 months history of PD and penile curvature of less than 50°. In this study, penile measurements were obtained by photographs taken by the researchers after a vasoactive agent induced an artificial erection. The patients were instructed to use the PTT for a minimum of 5 h per day, up to a maximum of 9 h. The results of this study showed that, in PD patients who completed the study, penile curvature decreased without statistical significance (31° to 27°; P=0.056); however, there was a significant improvement in the mean flaccid and stretched penile length measurements (1.3 and 0.8 cm, respectively). More importantly, the authors reported that there was no further change in penile curvature or length even 6 months after PTT. The results of this study suggested that, although the use of a penile extender device provided minimal improvements in penile curvature, there was a reasonable level of patient satisfaction, most probably because of increased penile length.
Recently, in a nonrandomized prospective controlled trial, investigators specifically assessed the efficacy of a penile traction device for the treatment of men in the acute phase of PD. In this study, 55 patients underwent PTT for 6 months, and were compared with 41 patients with acute phase of PD who did not receive active therapy. The results of the study showed that penile curvature decreased from 33° at baseline to 15° at 6 months and 13° at 9 months with a mean decrease of 20° (P˂0.05) in the PTT group. Additionally, pain scores significantly decreased after 6 months while erectile function and erection hardness also improved significantly in the PTT group, compared to the no intervention group. Furthermore, PTT was associated with the disappearance of sonographic penile plaques in 48% of PD patients, and the need for surgery was eliminated in 40% of patients who were, otherwise, good candidates for surgery. Altogether, these results suggested that PTT is an effective treatment option for the acute phase of PD, with significant decreases in pain and penile curvature, and an improvement in erectile function (6).
Abern et al. also described the use of PTT as a part of a combination treatment modality for men with PD. This study aimed to investigate the benefit of PTT when combined with intralesional verapamil injections and oral L-Arginine 1 g b.i.d. and pentoxifylline 400 mg t.i.d. in men with PD. Briefly, 74 men with PD completed 12 intralesional verapamil injections. Patients who opted for PTT used the device for 2–8 h daily. Stretched penile length and erect penile curvature using penile ultrasonography were measured. A ≥10° improvement in penile curvature was considered a clinically significant response to therapy. Men who used the device more than 3 h per day gained 0.6 cm in stretched penile length vs. 0.07 cm when used less than 3 h per day, while men who did not use the device lost 0.74 cm of stretched penile length on average. In summary, this study showed that better curvature improvement and stretched penile length gain was seen in the combination group. Additionally, multivariate analysis revealed that length improvement was related to the duration of traction device use (20).
More recently, in a similar study by Yafi et al., the benefit and duration of daily PTT was assessed in men with PD who underwent interferon α-2b therapy. A total of 112 patients underwent a median of 12 interferon α-2b injections, with daily use of PTT reported by 31% of patients. The results of this study showed that the use of penile traction did not affect change in penile girth. However, men who used PTT 3 or more hours per day gained significantly greater stretched penile length compared to those who did not undergo PTT (21).
The use of penile traction therapy (PTT) before penile surgery
Inflatable penile prosthesis (IPP) implantation is the standard of care for the treatment of patients with advanced ED, and/or is unresponsive to nonsurgical therapy. In most series, though the patient/partner satisfaction rates are generally high, concerns remain about penile length after IPP placement amongst a considerable group of patients. In a non-controlled pilot study, the effect of PTT in men with a shortened penis before IPP placement was investigated. This study included 10 patients who were instructed to wear the device for 2–4 h daily for 2–4 months before IPP placement. Baseline stretched penile length (SPL) was compared with post-traction SPL and post-implant inflated erect length. None of the patients complained about penile loss postoperatively, while 70% of men had measured length gain of up to 15 cm, compared with the baseline pre-traction SPL (22).
Similarly, in men who underwent IPP placement after radical prostatectomy, and were dissatisfied with post-significant loss of penile length post-operatively, authors recommended PTT for 6 months before IPP revision surgery in order to increase penile length. After 6 months of therapy, there was a 2.3-cm increase in SPL, which enabled the placement of a prosthesis that was 20% longer in length (15 to 18 cm), and erect penile length increased by 4.4 cm. These results suggested that the use of PTT increases penile corporal length, and, thus, the length of an IPP in a patient unsatisfied with his current IPP (23).
In another study conducted by Moncada-Iribarren et al., PTT was used in men who underwent PD surgery. In this series, 12 men had plaque incision + graft placement while 28 underwent penile plication. Patients were randomized to PTT vs. observation. PTT was applied for 8–12 h per day for at least 4 months. Penile shortening for both groups was from 0.5 to 4 cm. The use of PTT led to an increase in SPL, which ranged from 1 to 3 cm. Additionally, sustained treatment with PTT for 4 months caused an increase in SPL from 1 to 4 cm (24).
In a more recent study, authors have assessed patient outcomes with regards to SPL change and penile satisfaction after penile plication and partial plaque excision and grafting with or without postoperative application of PTT. The results of this study showed that, in patients who used PTT, there was no perceived length loss, while 58% reported a mean erect length gain of 1.1 cm, suggesting that postoperative PTT can result in length preservation, and, in most cases, measured and perceived length gain is possible after correction of the curvature (11).
Penile traction therapy (PTT) and penile dysmorphophobia
Penile dysmorphophobia has been defined as a body dysmorphic disorder. Body dysmorphia is a somatoform disorder conferred by preoccupation with an imaginary or trivial flaw in the physical appearance, which leads to deficiency in several areas of functioning. This problem can cause major depression and social dysfunction, which may ultimately lead to social isolation (25). Small penis syndrome has been described as an anxiety related to the external genitalia with the penile length being shorter than normal size for a normal adult (25). Studies have actually shown that, while there is an increase in men who are concerned about their penile length, most men complaining of short penis have, in fact, a normal sized penis (25,26). Real ‘Short penis-micropenis’ is defined as penile lengths of less than 4 and 7.5 cm, respectively in the flaccid and stretched configurations (26). According to recent literature, the use of PTT in men with a ‘normal sized’ penis is suggested as an alternative option against several surgical interventions which actually may cause devastating results (27).
In a phase-II prospective study conducted by Gontero, the efficacy of PTT was assessed in 15 men. After a 6-month treatment period, there was a significant gain in penile length (2.3 and 1.7 cm flaccid and stretched, respectively (28). In a similar study of 23 patients, PTT was applied for 4–6 h per day for the first 2 weeks and then 9 h per day until the end of the third month. Both flaccid and stretched penile sizes increased significantly during the first and second follow-up. Additionally, the circumference of the glans penis significantly increased after PTT (29). More recently, in another series, 54 men with a ‘short penis’ underwent PTT 4 to 6 h per day for 6 months. Flaccid, stretched, and erect penile length measurements were performed at baseline and again after 1, 3, 6 and 9 months. Additionally, erectile function was assessed at baseline and at 9 months after treatment by IIEF-5. A significant increase in flaccid, stretched, and erect penile length was observed at the 6th month follow-up, when compared to baseline values. On the other hand, no significant change was seen in penile girth after PTT treatment. Nine out of 13 patients with mild baseline ED reported normal erectile function after 9 months of PTT (25).
Altogether, the results of these studies suggest that PTT should be considered as a noninvasive and effective treatment modality to increase penile length in patients seeking treatment for a ‘Short/small penis’.
Conclusions
PTT is a relatively new area of interest for the nonsurgical treatment of men with PD. Additionally, PTT has been used in patients with postoperative loss of penile length, and for the management of men complaining of a small penis despite an objectively normal size. In the literature, there are an increased number of articles reporting promising results after the use of PTT. It is, however, important to consider several issues regarding PTT, including the efficacy of this therapy in the different subgroups of PD patients. Another important point is that, in comparison to PTT for the treatment of dysmorphophobia and postsurgical short penises, the lengthening benefit of this intervention in PD patients has been found to be inferior. Therefore, realistic expectations, especially in men with PD, should be discussed before recommending PTT. It should also be kept in mind that PTT requires a committed and compliant patient who is willing to devote time to a relatively long treatment period. Studies have shown that when used concomitantly with intralesional injection of both verapamil and INF α-2b, PTT provided a significant increase in stretched penile length when compared to no PTT. Therefore, it seems that PTT, in combination with intralesional plaque therapy, represents a good nonsurgical therapeutic option for men with PD.
In conclusion, level 2b evidence (according to the Oxford Centre for Evidence-based Medicine) suggests that PTT is a tolerable, minimally invasive method for men with PD. However, most of the studies related to this treatment option are not well designed and have a limited number of patients. Another important issue is that the time of device application (3 to 6 h) and treatment duration (3 to 6 months) remain to be defined. Further prospective, randomized, controlled studies with a larger number of patients and longer follow-up periods are needed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vardi Y, Levine LA, Chen J, et al. Is there a place for conservative treatment in Peyronie's disease? J Sex Med 2009;6:903-9. [Crossref] [PubMed]
- Kuehhas FE, Weibl P, Georgi T, et al. Peyronie's disease: nonsurgical therapy options. Rev Urol 2011;13:139-46. [PubMed]
- Gokce A, Wang JC, Powers MK, et al. Current and emerging treatment options for Peyronie's disease. Res Rep Urol 2013;5:17-27. [PubMed]
- Taylor FL, Levine LA. Non-surgical therapy of Peyronie's disease. Asian J Androl 2008;10:79-87. [Crossref] [PubMed]
- Chung E, Brock G. Penile traction therapy and Peyronie's disease: a state of art review of the current literature. Ther Adv Urol 2013;5:59-65. [Crossref] [PubMed]
- Martínez-Salamanca JI, Egui A, Moncada I, et al. Acute phase Peyronie's disease management with traction device: a nonrandomized prospective controlled trial with ultrasound correlation. J Sex Med 2014;11:506-15. [Crossref] [PubMed]
- Tan RB, Sangkum P, Mitchell GC, et al. Update on medical management of Peyronie's disease. Curr Urol Rep 2014;15:415. [Crossref] [PubMed]
- Hellstrom WJ. Medical management of Peyronie's disease. J Androl 2009;30:397-405. [Crossref] [PubMed]
- Bjekic MD, Vlajinac HD, Sipetic SB, et al. Risk factors for Peyronie's disease: a case-control study. BJU Int 2006;97:570-4. [Crossref] [PubMed]
- Qian A, Meals RA, Rajfer J, et al. Comparison of gene expression profiles between Peyronie's disease and Dupuytren's contracture. Urology 2004;64:399-404. [Crossref] [PubMed]
- Rybak J, Papagiannopoulos D, Levine L. A retrospective comparative study of traction therapy vs. no traction following tunica albuginea plication or partial excision and grafting for Peyronie's disease: measured lengths and patient perceptions. J Sex Med 2012;9:2396-403. [Crossref] [PubMed]
- Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res 1989.249-81. [PubMed]
- Molea G, Schonauer F, Blasi F. Progressive skin extension: clinical and histological evaluation of a modified procedure using Kirschner wires. Br J Plast Surg 1999;52:205-8. [Crossref] [PubMed]
- Sun JS, Hou SM, Hang YS, et al. Ultrastructural studies on myofibrillogenesis and neogenesis of skeletal muscles after prolonged traction in rabbits. Histol Histopathol 1996;11:285-92. [PubMed]
- Bailey AJ, Tarlton JF, Van der Stappen J, et al. The continuous elongation technique for severe Dupuytren's disease. A biochemical mechanism. J Hand Surg Br 1994;19:522-7. [Crossref] [PubMed]
- Brandes G, Messina A, Reale E. The palmar fascia after treatment by the continuous extension technique for Dupuytren's contracture. J Hand Surg Br 1994;19:528-33. [Crossref] [PubMed]
- Scroppo FI, Mancini M, Maggi M, et al. Can an external penis strecher reduce Peyronie’s penile curvature? Int J Imp Res 2001;13:S21.
- Levine LA, Newell M, Taylor FL. Penile traction therapy for treatment of Peyronie's disease: a single-center pilot study. J Sex Med 2008;5:1468-73. [Crossref] [PubMed]
- Gontero P, Di Marco M, Giubilei G, et al. Use of penile extender device in the treatment of penile curvature as a result of Peyronie's disease. Results of a phase II prospective study. J Sex Med 2009;6:558-66. [Crossref] [PubMed]
- Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie's disease. J Sex Med 2012;9:288-95. [Crossref] [PubMed]
- Yafi FA, Pinsky MR, Stewart C, et al. The effect of duration of penile traction therapy in patients undergoing ıntralesional ınjection therapy for Peyronie's disease. J Urol 2015;194:754-8. [Crossref] [PubMed]
- Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med 2011;8:2112-7. [Crossref] [PubMed]
- Moskovic DJ, Pastuszak AW, Lipshultz LI, et al. Revision of penile prosthesis surgery after use of penile traction therapy to increase erect penile length: case report and review of the literature. J Sex Med 2011;8:607-11. [Crossref] [PubMed]
- Moncada-Iribarren I, Jara J, Martinez-Salamanca J, et al. Managing penile shorthening after Peyronie’s disease surgery. J Urol 2007;177:252. [PubMed]
- Nowroozi MR, Amini E, Ayati M, et al. Applying extender devices in patients with penile dysmorphophobia: assessment of tolerability, efficacy, and impact on erectile function. J Sex Med 2015;12:1242-7. [Crossref] [PubMed]
- Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol 1996;156:995-7. [Crossref] [PubMed]
- Ghanem H, Glina S, Assalian P, et al. Position paper: Management of men complaining of a small penis despite an actually normal size. J Sex Med 2013;10:294-303. [Crossref] [PubMed]
- Gontero P, Di Marco M, Giubilei G, et al. A pilot phase-II prospective study to test the 'efficacy' and tolerability of a penile-extender device in the treatment of 'short penis'. BJU Int 2009;103:793-7. [Crossref] [PubMed]
- Nikoobakht M, Shahnazari A, Rezaeidanesh M, et al. Effect of penile-extender device in increasing penile size in men with shortened penis: preliminary results. J Sex Med 2011;8:3188-92. [Crossref] [PubMed]


