
Baseline urine pH is related to effective urine alkalization by short-term alkaline water supplementation: data from a self-controlled study in healthy Chinese volunteers following a systematic review and meta-analysis of literature
Introduction
Globally, urolithiasis has been reported to affect 1–5% of Asians, 5–9% of Europeans, and 7–13% of North Americans (1-3). Among these, uric acid (UA) calculi account for 8–10% of all cases and are more predominant in regions with hot climates due to supersaturation and crystallization of the urine (4). Along with evolving socioeconomics and lifestyle in recent decades, the prevalence of UA calculi has been on the rise (5).
Studies have shown that formation of UA stones is strongly propelled by presence of acidic urine (6,7), and thus can be prevented by promoting the urine pH to alkaline range (8,9). Use of sodium bicarbonate is a common option for urine alkalization in patients with UA calculi, but not justified for regular use in normal individuals as a prevention, considerably due to gastrointestinal disturbance. On the other hand, a dietary approach could be more acceptable for this purpose (8,10-13). Based on the acid–ash hypothesis, oral use of alkaline water has been attempted to provide more alkaline ions after metabolism. In a randomized trial, supplementation of alkaline water led to minimal increase in systemic pH by 0.014 units compared to that in urine pH by 1.02 (14).
However, there seems to be a paucity of reliable data about the effect of alkaline water on urine pH. Amid the sparse research interest on this topic, the outcomes of urine alkalization with alkaline water supplementation vary greatly across studies and therefore remain inconclusive, probably arising from differences in study design, ethnic group, and source of alkaline water. These need further clarification. It also remains unclear whether the mixed findings were complicated by certain factors like gender and obesity, as this has not been reported. In addition, the outcomes of alkaline water supplementation have rarely been evaluated in a study among Chinese, if any.
To elucidate the usefulness of alkaline water supplementation in urine alkalization, we aimed to perform a systematic literature review of relevant studies exploring the association between alkaline water supplementation and urine pH. Moreover, we aimed to further contribute to the literature by conducting an empirical observation on urine alkalization with alkaline water vs. daily drinking water among healthy Chinese volunteers. We hypothesized that, a priori, gender and body mass index (BMI) in relation to physiology and metabolism of the body, may have a role in the outcomes of alkaline water supplementation. We present the following article in accordance with the PRISMA and STARD reporting checklists (available at https://tau.amegroups.com/article/view/10.21037/tau-22-280/rc).
Methods
Systematic review and meta-analysis
Literature search strategy
Prior to our study in human volunteers, a systematic review and meta-analysis was conducted to assess the effect of alkaline water on urine pH, in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (15).
A systematic literature search using the PubMed, Embase, Medline and Cochrane Library databases was performed to identify relevant studies on alkaline water supplementation and urine pH, from inception to February 01, 2021. The search terms were (“alkaline water” OR “AK water”) AND “urine pH”. The publication language was restricted to English. Reference lists of the relevant studies were also checked to identify potential records.
Patient, intervention, comparison, outcome, and study design (PICOS) question
A question was formulated according to the PICOS framework to guide the review in this study: does alkaline water supplementation (Intervention) increase the urine pH (Outcome) of human (Patient) compared with those who drink regular table water (Comparison)?
Inclusion and exclusion criteria
The included studies were restricted to controlled trials exploring the association between alkaline water supplementation and urine pH published in English language. Other publication types, including abstracts, case reports, proceedings, reviews, and animal experiments were excluded. Duplicate publications or studies with potential data overlap, as well as those with nonignorable missing data, were also considered ineligible.
Quality assessment and data extraction
The level of evidence (LOE) of all included studies was assessed based on the criteria developed by the Oxford Centre for Evidence-based Medicine in 2009. The quality of randomized controlled trials (RCTs) was evaluated using the Cochrane risk of bias tool, and the Newcastle-Ottawa Scale (NOS) was applied for the quality of non-RCTs.
The data extracted from the included studies were as follows: first author, year of publication, study country, target population, study duration, research methodology, characteristics of participants, and related outcomes. When necessary, the authors of these studies were contacted for further information.
The search and selection of relevant studies, quality assessment and data extraction were performed by two reviewers independently. All between-reviewer discrepancies were reconciled through group discussion.
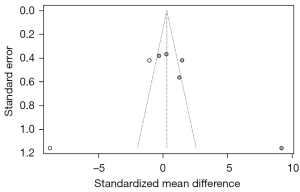
Our meta-analysis was processed with RevMan software (version 5.3; Cochrane Collaboration, Oxford, UK). Summarized standardized mean differences (SMDs) of pooled data with 95% confidence intervals (CIs) were calculated to assess the outcomes of alkaline water supplementation on urine pH. Chi-square-based Q-test and I2-statistic test were used to examine the statistical heterogeneity among included studies (16). If no heterogeneity existed (P>0.10), the fixed-effect model was used; otherwise, the random-effect model was employed. The tests for significance were two-sided. Publication bias among included studies was assessed with inverted funnel plotting.
The pre-post comparison in human volunteers
Study population
Several months after completion of our meta-analysis, we tentatively approached 100 medical students from Guangzhou Medical University to be recruited as healthy volunteers in early October of 2021. Among these, there were 51 males and 49 females, with a male-to-female ratio close to 51.25% vs. 48.76% as released by the Chinese Population Census 2021. Given the paucity of reference data on this topic, our consideration for initial sample size (n=100) was based on the total number of subjects included in all studies we meta-analyzed (n=94, see below). In addition, the normal range of urine pH in healthy subjects (5.5 to 7.5), measured to the nearest 0.1, corresponds to a spectrum of twenty 0.1-pH units, such that we speculated that 100 subjects with 51 males and 49 females (nearly 2.5-fold of twenty) could be suitable. Furthermore, as a convenience sample, the initial sample size of 100 healthy subjects was considered proper, regarding the number of students readily available in our institution who would be voluntary but not obliged to participate in a human study. The inclusion criteria were (I) aged ≥18 years old; (II) habitually on a regular balanced diet; (III) willing to comply with our study protocol, in particular, the daily measurement of urine pH. The exclusion criteria were (I) urinary system malformation; (II) active or uncontrolled urinary tract infection; (III) urolithiasis, pregnancy, diabetes and parathyroid disorders; (IV) projected menstrual period (for females) or having any known health problems that could interfere with urine pH measurements during the study; (V) uncertainty in maintaining a stable diet throughout the study. After careful screening of potential participants by interviews and physical checkup, our final study sample consisted of 73 healthy volunteers according to the inclusion and exclusion criteria, comprising 50 males and 23 females. This human subjects study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the First Affiliated Hospital of Guangzhou Medical University (No. GMU-2020-163) and informed consent was taken from all individual participants.
Alkaline water supplementation and outcome measures
The human volunteers study was conducted in two sessions from 21 October to 3 November, 2021, lasting a total of 2 weeks. In the baseline session (days 1–7, from 21 to 27 October, 2021), the subjects remained on daily consumption of normal tap water (H2O). In the experiment session (days 8–14, from 28 October to 3 November, 2021), alkaline water was exclusively used for fluid intake (pH 8.0–9.0). The major components of the alkaline water source used in this study were: (I) Metasilicic acid (H2SiO3) ≥10 mg/L; (2) Na+, 93–150 mg/L; (3) HCO3−, 247–350 mg/L. Throughout the study, the volunteers were instructed to remain on water intake following their daily habit or investigation protocol (depending on study sessions), to refrain from strenuous or intensely sweating exercises, and to keep a diary on their diet for investigators’ perusal. Acidic drinks, fruit juice and any food that may affect the urine pH were not allowed.
On entering the study, the subjects were measured for body weight and height. BMI was calculated as body weight (kg) divided by squared height (meter), to the nearest 0.1. According to manufacturer’s instructions, urine pH was determined thrice per day (in the first morning sample, at 2 o’clock in the afternoon, and at 8 o’clock in the evening) using a pH meter, to the nearest 0.1 (SevenDirect SD20, Mettler-Toledo Inc, USA); then the mean value was specifically computed for that study day. The mean urine pH during the baseline session was defined as baseline urine pH, while that during the experiment session was defined as alkalized urine pH. Alkalization gains in urine pH (AGU-pH) was defined as alkalized urine pH minus baseline urine pH. Effective urine alkalization, corresponding to the favorable outcome of alkaline water supplementation, was determined when an AGU-pH >0 was noted and found to be statistically significant in any given participant.
Any adverse events with alkaline water supplementation during the experiment session, including appetite loss, dyspepsia, and abdominal discomfort, were recorded.
Statistical analysis
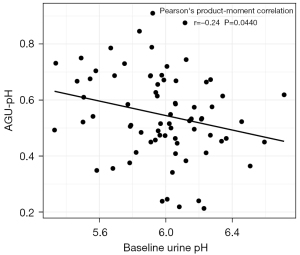
Of all subjects, quantitative data including age, BMI, and pH value, were expressed as mean ± SD. The mean urine pH values were compared between the baseline and experiment sessions by paired t-test. The association between AGU-pH and baseline urine pH was evaluated with Pearson’s product-moment correlation, yielding a product-moment correlation coefficient. The optimal cut-off value of baseline urine pH in relation to effective urine alkalization was determined using receiver operating curve (ROC) analysis with calculation of Youden index. Two-sided P value <0.05 was deemed statistically significant. All statistical analyses in human volunteers were performed using R software (R 3.4.4).
Results
A total of four studies (17-20) with 94 subjects were included in our meta-analysis (Figure 1) of literature prior to human volunteer study. Among them, two were RCTs and two were self-controlled studies. The durations of alkaline water supplementation ranged from one to four weeks in these studies. With a high degree of heterogeneity detected across studies (I2=94%, P<0.001), the random-effect model was applied for the meta-analysis. Results of the meta-analysis showed that supplementation of alkaline water could significantly increase the urine pH (SMD =2.04, 95% CI: 0.31 to 3.76, P=0.02) (Figure 2). No obvious publication bias was detected by inverted funnel plotting (Figure 3).
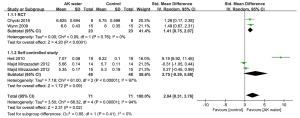
However, the quality of these four articles was considered poor (LOE III or IV). Either random sequence generation or allocation concealment was not clearly reported in the RCTs. The two non-RCTs were rated as high risk of bias (NOS score <5). Small sample size was a common problem, as reflected by the total number of subjects (n=94) from all of the included studies. None of these studies took into consideration the potential effect of BMI or gender. Chinese participants were not included as the whole study population or part of study cohorts, either.
Our study population included a total of 73 volunteers, aged 18 to 25 years old (mean: 20 years old). The baseline characteristics of the volunteers are presented in Table 1. Of these subjects, 50 were men (68.5%) and 23 were women (31.5%). There were 12 (16.4%) subjects with a BMI ≥25.0 and 10 (13.7%) with a BMI <18.5, while the large majority [51 (69.9%)] had a BMI ranging from 18.5 to 24.9.
Table 1
| Characteristic | Value |
|---|---|
| Age, years (mean ± SD) | 20±2.74 |
| Gender, n (%) | |
| Male | 50 (68.5) |
| Female | 23 (31.5) |
| BMI, n (%) | |
| ≥25 | 12 (16.4) |
| 18.5–25 | 51 (69.9) |
| <18.5 | 10 (13.7) |
SD, standard deviation; BMI, body mass index.
For each subject, positive AGU-pH was noted by comparing the alkalized urine pH to baseline urine pH via t-test. Subgroup analysis stratified by gender and BMI indicated that the outcome of urine alkalization (baseline vs. alkalized urine pH value) was more pronounced in males (6.12±0.39 vs. 6.50±0.34, P<0.001) than in females (6.22±0.53 vs. 6.50±0.43, P=0.058), but did not differ significantly across BMI subgroups (Table 2). In other words, statistically significant increases in urine pH after supplementation of alkaline water were observed in underweight, normal, or overweight/obese subjects (all P<0.01).
Table 2
| Baseline urine pH | Alkalized urine pH | AGU-pH | P value | |
|---|---|---|---|---|
| Gender | ||||
| Male | 6.12±0.39 | 6.50±0.34 | 0.57±0.15 | <0.001*** |
| Female | 6.22±0.53 | 6.50±0.43 | 0.50±0.15 | 0.0575 |
| BMI | ||||
| ≥25 | 6.02±0.40 | 6.52±0.44 | 0.51 ±0.14 | 0.0086** |
| 18.5–25 | 6.27±0.45 | 6.51±0.37 | 0.57±0.16 | 0.0042** |
| <18.5 | 6.04±0.32 | 6.43±0.28 | 0.51±0.14 | 0.0094** |
| Overall | 5.98±0.28 | 6.52±0.29 | <0.001*** |
Data were presented as mean ± SD and processed by paired t-tests. There was no significant difference in alkalized urine pH between males and females, or across all BMI subgroups (P>0.05). **, P<0.01; ***, P<0.001. SD, standard deviation; BMI, body mass index; AGU-pH, alkalization gains in urine pH.
Of all subjects, 62 (84.9%) presented effective urine alkalization (AGU-pH >0 and P<0.05). Noteworthily, subjects who presented effective urine alkalization had lower baseline urine pH compared with those who did not (5.94±0.27 vs. 6.22±0.22, P=0.0016) (Table 3). This finding suggested that the outcome of urine alkalization might be related to the baseline urine pH. For further confirmation, the Pearson’s product-moment correlation analysis was performed, which demonstrated a negative correlation between AGU-pH and baseline urine pH (r=−0.236, P=0.044) (Figure 4). This observation seemingly pointed to a clue that effective urine alkalization was more likely to achieve in subjects with “more acidic” urine. In fact, as shown by distribution histogram of baseline urine pH value (to the nearest 0.1 units), almost all subjects who did not experience effective urine alkalization had a baseline urine pH >6.0 [Youden index(max) = 1.548, cutoff value of urine pH =5.977] (Figure 5A,5B).
Table 3
| Effective urine alkalization | Baseline urine pH | Alkalized urine pH | n |
|---|---|---|---|
| Yes | 5.94±0.27 | 6.52±0.28 | 62 |
| No | 6.22±0.22 | 6.58±0.34 | 11 |
| P value | 0.0016** | 0.5555 |
Data were presented as mean ± SD and processed by t-tests. **, P<0.01. SD, standard deviation.

It is noticeably that the mean alkalized urine pH value was 6.50±0.34 in males, 6.50±0.43 in females, 6.43 to 6.52 in subjects with any BMI, and 6.50±0.29 in the entire study population (all P>0.05). The mean alkalized urine pH value also did not vary between subjects with and without effective urine alkalization (6.52±0.28 vs. 6.58±0.34, P=0.5555). These findings suggested that the 7-day supplementation of alkaline water with the formulation described in our study resulted in a similar range of alkalized urine pH, and did not lead to over-alkalization that adversely favors formation of calcium- or phosphate-containing stones.
None of the volunteers in this study reported any adverse event during the experiment session with alkaline water supplementation.
Discussion
Studies have shown the benefits of alkaline water in gastroesophageal reflux (21,22), certain cancers (23,24), and in reducing the blood viscosity (25). Athletes supplemented with alkaline water after high-intensity interval exercises were found to experience favorable changes in hydration status with lower urine specific gravity, higher urine pH, and more efficient use of lactates (20,26). However, favorable outcomes of urine alkalization by alkaline water supplementation, perceived as a dietary prevention against UA calculi, largely remains indefinite.
To shed light on the current opinions, we conducted a systematic review of literature on this topic. Pertaining to our search strategy, unfortunately, relevant data appeared fairly limited about the outcomes of alkaline water on urine pH. Despite an increase in urine pH after supplementation of alkaline water as indicated by the random-effect model, only four controlled studies were included in our meta-analysis, obviously with a high heterogeneity that precludes a robust determination. Such heterogeneity may arise from differences in study population, design, or ethnic group, and more importantly, the source of alkaline water. This dilemma rendered our subsequent investigation in human volunteers needed.
Overall, we identified effective urine alkalization after alkaline water supplementation, as reflected by positive gains in urine pH from baseline (AGU-pH >0 and P<0.05), in the large majority (84.9%) of our study population consisting of 73 healthy non-athlete Chinese subjects. Such a favorable outcome was not affected by BMI. Interestingly, on an individual basis, effective urine alkalization was determined largely in subjects with an imputed baseline urine pH ≤6.0. The negative correlation between AGU-pH and baseline urine pH indicated that subjects with “more acidic” urine were more likely to show effective urine alkalization after drinking alkaline water, compared to those with higher baseline urine pH. As this can be further interpreted, preventing UA calculi by supplementation of alkaline water is not always justified for all but should be considered only in selected cohorts, such as individuals with a lower urine pH.
Our gender-based subgroup analysis showed that only male subjects showed favorable outcomes from alkaline water supplementation. At a first glance, it was speculated that this could be due to the higher urine pH in normal women compared with men (27). On second thought, the fewer females compared with males (31.5% vs. 68.5%) in this study could be a confounding factor. As per our protocol, we excluded females with a menstrual period projected to occur during the 2-week human study, to avoid interference with urine pH measurements. The lower inclusion rate of females (23 out of 49, 46.9%) could be explained by the theoretical probability of exclusion (50.0%) based on the designed study duration and the mean cycle of menstruation (14 vs. 28 days). We have to inform that this was not foreseen at study design. Despite these, to the best of our knowledge, no study has looked at gender difference in the effect of alkaline water on urine pH. Future studies are therefore needed for further clarification.
In contrast to regular drinking water, alkaline water (pH 8.0–9.0) is usually believed to have an acid-neutralizing action in the body (28). In fact, the role of alkaline water in urine alkalization does not rely merely on alkaline substances it contains, but also on various biochemical processes, such as acid-base interaction in the stomach, bioavailability, renal function, as well as contents of natural minerals that give rise to negative redox potential favoring an antioxidant action (29). As stated above, discrepancy in published studies may be partly attributed to the source of alkaline water. Artificial products aside, natural alkaline water sources vary widely in mineral levels and thus cannot account for a consistent effect on urine pH (30). Further research on urine alkalization using alkaline water in humans is expected to take these factors into consideration.
The mineral-rich alkaline water used in our study was harvested kilometers deep beneath the Keluo-Wudalianchi-Erkeshan cenozoic volcanic rock belt with a remote geological age. Our study showed good safety profiles with short-term supplementation of alkaline water from the described source. In all subjects, the resultant urine pH after drinking alkaline water for seven days seemed to be within a range that could not be construed as over-alkalization, regardless of baseline urine pH or final outcomes of urine alkalization.
Several limitations in the present study need to be acknowledged. Firstly, the number of volunteers enrolled was relatively small. A study with larger sample size should not only increase the statistical power but also offer more convincing results. Secondly, our human study was conducted in a short duration and therefore could not account for long-term preventive attempts. Likewise, urine pH is strongly affected by temperatures and climates, which prompts for a need for repeated study in different seasons, especially during the summer. Thirdly, certain confounders, such as urine output, renal function and metabolic rate were not addressed. Moreover, while gender was likely linked to the outcome of urine alkalization and hence the AGU-pH or baseline urine pH, the small sample size and relatively lower proportion of females in this study disabled the reliability of a multivariate regression to account for this. Adjusting for these confounders, and including more factors into a regression model to develop a prediction model and determine the cut-off value based on the model scores, should be encouraged in future studies. In the context of these caveats, our findings should be interpreted with prudence.
In summary, alkaline water supplementation can be useful for urine alkalization. Drinking alkaline water as a prevention against UA calculi may be suitable only for individuals with a lower baseline urine pH (≤6.0). Short-term use of alkaline water is well-tolerated and not associated with over-alkalization of the urine. There seems to be a gender difference in the outcome of alkaline water supplementation, despite more efforts warranted to validate our findings.
Acknowledgments
Funding: This study was funded by Guangzhou Municipal Science and Technology Bureau Project (No. 2060206, No. 202102010306), Guangdong Basic and Applied Basic Research Foundation (No. 2021A1515111208).
Footnote
Reporting Checklist: The authors have completed the PRISMA and STARD reporting checklists. Available at https://tau.amegroups.com/article/view/10.21037/tau-22-280/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-22-280/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-22-280/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-280/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This human subjects study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the First Affiliated Hospital of Guangzhou Medical University (No. GMU-2020-163) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Raheem OA, Khandwala YS, Sur RL, et al. Burden of Urolithiasis: Trends in Prevalence, Treatments, and Costs. Eur Urol Focus 2017;3:18-26. [Crossref] [PubMed]
- Chewcharat A, Curhan G. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis 2021;49:27-39. [Crossref] [PubMed]
- Gadzhiev N, Prosyannikov M, Malkhasyan V, et al. Urolithiasis prevalence in the Russian Federation: analysis of trends over a 15-year period. World J Urol 2021;39:3939-44. [Crossref] [PubMed]
- Khan SR, Pearle MS, Robertson WG, et al. Kidney stones. Nat Rev Dis Primers 2016;2:16008. [Crossref] [PubMed]
- Sakhaee K. Epidemiology and clinical pathophysiology of uric acid kidney stones. J Nephrol 2014;27:241-5. [Crossref] [PubMed]
- Kim JC, Cho KS, Kim DK, et al. Predictors of Uric Acid Stones: Mean Stone Density, Stone Heterogeneity Index, and Variation Coefficient of Stone Density by Single-Energy Non-Contrast Computed Tomography and Urinary pH. J Clin Med 2019;8:243. [Crossref] [PubMed]
- Ferraro PM, Taylor EN, Gambaro G, et al. Dietary and Lifestyle Risk Factors Associated with Incident Kidney Stones in Men and Women. J Urol 2017;198:858-63. [Crossref] [PubMed]
- Jia E, Zhu H, Geng H, et al. Effect of alkalized urine on renal calculi in patients with gout: a protocol for a placebo-controlled, double-blinded randomized controlled trial. Trials 2021;22:743. [Crossref] [PubMed]
- Cicerello E. Uric acid nephrolithiasis: An update. Urologia 2018;85:93-8. [Crossref] [PubMed]
- Paonessa JE, Williams JC Jr, Lingeman JE. Addition of Sodium Bicarbonate to Irrigation Solution May Assist in Dissolution of Uric Acid Fragments During Ureteroscopy. J Endourol 2018;32:305-8. [Crossref] [PubMed]
- Cicerello E, Merlo F, Maccatrozzo L. Urinary alkalization for the treatment of uric acid nephrolithiasis. Arch Ital Urol Androl 2010;82:145-8. [PubMed]
- Li HY, Lian PY, Zhou ZY, et al. Treatment of renal uric acid stone by extracorporeal shock wave lithotripsy combined with sodium bicarbonate: 2 case reports. Int J Clin Exp Med 2015;8:14130-5. [PubMed]
- Xue X, Liu Z, Li X, et al. The efficacy and safety of citrate mixture vs sodium bicarbonate on urine alkalization in Chinese primary gout patients with benzbromarone: a prospective, randomized controlled study. Rheumatology (Oxford) 2021;60:2661-71. [Crossref] [PubMed]
- Buclin T, Cosma M, Appenzeller M, et al. Diet acids and alkalis influence calcium retention in bone. Osteoporos Int 2001;12:493-9. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [Crossref] [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- Mirzazadeh M, Nouran MG, Richards KA, et al. Effects of drinking water quality on urinary parameters in men with and without urinary tract stones. Urology 2012;79:501-7. [Crossref] [PubMed]
- Chycki J, Kurylas A, Maszczyk A, et al. Alkaline water improves exercise-induced metabolic acidosis and enhances anaerobic exercise performance in combat sport athletes. PLoS One 2018;13:e0205708. [Crossref] [PubMed]
- Heil DP. Acid-base balance and hydration status following consumption of mineral-based alkaline bottled water. J Int Soc Sports Nutr 2010;7:29. [Crossref] [PubMed]
- Wynn E, Krieg MA, Aeschlimann JM, et al. Alkaline mineral water lowers bone resorption even in calcium sufficiency: alkaline mineral water and bone metabolism. Bone 2009;44:120-4. [Crossref] [PubMed]
- Zalvan CH, Hu S, Greenberg B, Geliebter J. A Comparison of Alkaline Water and Mediterranean Diet vs Proton Pump Inhibition for Treatment of Laryngopharyngeal Reflux. JAMA Otolaryngol Head Neck Surg 2017;143:1023-9. [Crossref] [PubMed]
- Dragomiretska NV, Babov KD, Gushcha SG, et al. Application of mineral waters in the complex treatment of patients with gastroesophageal reflux disease. Minerva Gastroenterol Dietol 2020;66:225-37. [Crossref] [PubMed]
- Fenton TR, Huang T. Systematic review of the association between dietary acid load, alkaline water and cancer. BMJ Open 2016;6:e010438. [Crossref] [PubMed]
- Al Zahrani SM, Omar UM, Rahimulddin SA, et al. Antiproliferative and apoptotic effects of the natural alkaline water (Zamzam) in breast cancer cell line MCF-7. J Cancer Res Ther 2019;15:1098-104. [Crossref] [PubMed]
- Weidman J, Holsworth RE Jr, Brossman B, et al. Effect of electrolyzed high-pH alkaline water on blood viscosity in healthy adults. J Int Soc Sports Nutr 2016;13:45. [Crossref] [PubMed]
- Chycki J, Zając T, Maszczyk A, et al. The effect of mineral-based alkaline water on hydration status and the metabolic response to short-term anaerobic exercise. Biol Sport 2017;34:255-61. [Crossref] [PubMed]
- Worcester EM, Bergsland KJ, Gillen DL, et al. Mechanism for higher urine pH in normal women compared with men. Am J Physiol Renal Physiol 2018;314:F623-9. [Crossref] [PubMed]
- Casado Á, Ramos P, Rodríguez J, et al. Types and characteristics of drinking water for hydration in the elderly. Crit Rev Food Sci Nutr 2015;55:1633-41. [Crossref] [PubMed]
- Liu Y, Wei L, Luo D, et al. Geochemical distribution and speciation of thallium in groundwater impacted by acid mine drainage (Southern China). Chemosphere 2021;280:130743. [Crossref] [PubMed]
- Heer F, Dobenecker B, Kienzle E. Effect of cation-anion balance in feed on urine pH in rabbits in comparison with other species. J Anim Physiol Anim Nutr (Berl) 2017;101:1324-30. [Crossref] [PubMed]



