A syndrome of erectile dysfunction in young men?
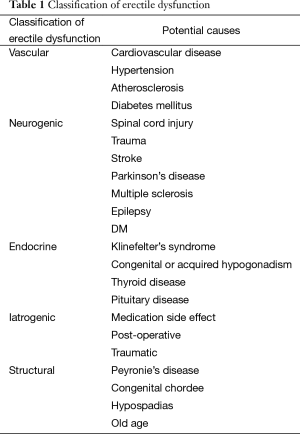
Erectile dysfunction in young men is an increasingly common chief complaint seen in urology clinics across the world (1). The international urologic community has taken an increased interest in this topic, with experts in the field of andrology and sexual dysfunction publishing multiple review articles (2,3) and an AUA Update Series Lesson (4) dedicated to this concerning issue. These articles skillfully address the epidemiology and diagnostic evaluation of ED and categorize ED (Table 1) into psychogenic or organic causes, addressing treatment options with specific interventions for each of the most common diagnoses.
Full table
What has been excluded entirely from all recent discussions of ED in young men is a concept presented many years ago—the concept of increased sympathetic tone as an organic etiology of “psychogenic” erectile dysfunction in young men (5). Previous studies have shown that elevated central sympathetic tone may be one cause of impotence (6,7). This article focuses on the presentation, work-up, and treatment of young men (age: 16–35 years old) with complaints of ED, and we will attempt to present a new method of approaching these patients. It is important to identify the precise etiology of ED in these men before proceeding with potentially unnecessary evaluation and treatment as the process can be anxiety-provoking, invasive, and costly and may provide an unreliable diagnosis which produces further psychological distress in these psychologically fragile young men.
Pathophysiology of hypertonic cavernous smooth muscle as an etiology for ED
Sexuality and erection are controlled by multiple areas of the human brain including the hypothalamus, the limbic system, and the cerebral cortex. Stimulatory or inhibitory messages are relayed to the spinal erection centers to facilitate or inhibit erection (5). Two mechanisms have been proposed to explain the inhibition of erection in psychogenic dysfunction: direct inhibition of the spinal erection center by the brain as an exaggeration of the normal suprasacral inhibition and excessive sympathetic outflow or elevated peripheral catecholamine levels, which may increase penile smooth muscle tone and prevent the relaxation necessary for erection (8). Animal studies demonstrate that the stimulation of sympathetic nerves or systemic infusion of epinephrine causes detumescence of the erect penis (6,7). Clinically, higher levels of serum norepinephrine have been reported in patients with psychogenic ED than in normal controls or patients with vasculogenic ED (9).
Multiple authors have demonstrated that anxiety, depression, and stress clearly produce major neurochemical and neuroendocrine changes in the brain (10,11). Changes in neurobiology would be expected to contribute to impaired erectile function. Stress and anxiety lead to increased epinephrine production, and heightened sympathetic tone leads to exaggerated cavernosal smooth muscle contraction, inability of smooth muscle to relax, and subsequent erectile dysfunction (6,7). Failure to achieve a fully rigid erection may aggravate performance anxiety leading to a vicious cycle.
Patient presentation
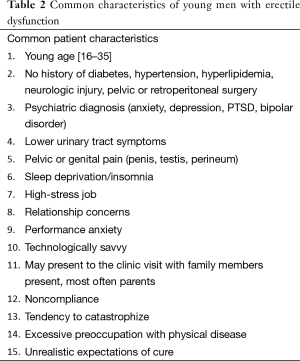
These are among the most challenging patients seen in urology practice today: a young, healthy man with neither systemic disease nor a history of trauma, who has complaints of ED (Table 2). These men often have co-morbid diagnoses, such as anxiety, depression, or mood disorders, which make the issue of ED more complex for both the patient and the urologist (12). The psychological burden of ED in these young men is more pronounced than it might be in older men as this is the phase of life during which many men expect to be highly sexually active (4). These young men are usually technologically savvy and may have scrutinized much of the readily available information on the internet regarding ED. Often they arrive to clinic armed with an understanding of the diagnostic evaluation that may be offered to further investigate the etiology of their concerns. This makes the evaluation and treatment of these men more challenging since additional diagnostic testing is often not indicated after a thorough history and physical examination. In many cases, they may have self-diagnosed and self-treated based on the information that they obtained prior to seeing a physician. Many of these men will see multiple urologists on their quest to find a pathophysiology that they can accept, and many have unrealistic expectations of a rapid cure or a surgical cure.
Full table
Care for these patients, who in many cases are emotional, demanding, and time consuming, may evoke feelings of frustration and anticipatory anxiety in the time-strapped urologist. Early in the encounter, the urologist must understand the patient’s psychosocial environment and establish a rapport and meaningful alliance with the patient and his family, if present (13). It is important to ensure that the doctor-patient interaction is informative and task oriented for greater patient buy-in and compliance with treatment (13,14). Affirm to the patient that regardless of the short time allotted for the visit that the doctor-patient relationship will endure even after the visit. This may be accomplished through a scheduled follow-up telephone call, electronic message, follow-up clinic visit, or a written letter. It may also be beneficial to refer the patient to a sex therapist or counselor though many young men will reject the idea that there is a psychosocial element to their ED and may refuse to consider therapy.
Initial evaluation: the subjective and the objective
The urologist must discuss the topic of ED delicately and caringly in order to earn the patient’s trust and be permitted to address his problem (15). It is important early during the visit to engage the patient and provide him reassurance that you will work as a team to evaluate and treat his disorder. A detailed history is the most important component of the evaluation. A thorough sexual history has many components. It should begin with information regarding onset, duration, severity, patient-suspected etiology of the ED. Ask the patient to define his specific concerns. The term “erectile dysfunction” is very broad, and the patient may actually have arousal issues or ejaculatory concerns or a combination of concerns. Ask specific questions regarding erectile hardness and sustainability during self-stimulation versus with a partner (global versus situational ED). Determine if the patient has ED in certain positions (lying down versus upright or seated). Inquire about libido and nocturnal erections. It is also important to ask the patient about past treatments and response. Inquire about any concomitant pain issues, irritative or obstructive voiding symptoms, or pelvic floor complaints.
Additional information to obtain includes a psychosocial and cultural history to assess past and present relationships, emotional or professional stressors, current and previous psychological/behavioral diagnoses and treatments, educational level and employment status, and location of domicile. A methodical medical history should be obtained to identify medical conditions that might be contributing to the patient’s ED. A thorough physical examination should be performed on all new patients with emphasis on the cardiovascular, genital, endocrine, and neurologic systems. On physical examination in a man with hypertonic cavernous smooth muscle, the penis may initially be contracted and tender to palpation. As the exam proceeds and the patient becomes less anxious, the penile tissue will often noticeably relax.
After a full history and physical examination, the urologist likely has a perception of the etiology of the problem. Additional laboratory evaluations may be necessary to evaluate for specific types of organic disease. These tests might include serum chemistry, complete blood count, lipid profile, thyroid stimulation hormone/free thyroxine, and early morning serum testosterone to assess for metabolic abnormalities, such as diabetes mellitus, hyperlipidemia, renal dysfunction, thyroid disease, and hypogonadism (16). These are not mandatory components of the assessment in a patient with hypertonic cavernous smooth muscle as the source of ED.
Oftentimes, after a thorough history and physical examination, additional diagnostic testing is not necessary to categorize ED (17). Depending on concerns raised from the history and physical examination, directed lab-work or additional studies may be conducted to ensure that the patient does not have medical disease that might be causing ED. All men with suspected vasculogenic erectile dysfunction deserve a cardiovascular assessment (18).
If the patient complains of loss of sensation on his penile shaft or glans, it is useful to perform hot and cold perception testing and/or additional vibratory sensory testing with biothesiometer. These are tests that can be performed quickly during the office visit and provide useful information about the function of the dorsal nerve of the penis (Table 3).

Full table
If the patient reports a history of trauma to the genitals that preceded his erectile dysfunction, further evaluation with pharmacologic injection and penile color duplex ultrasound (PCDU) would be indicated to assess for arterial insufficiency or venous occlusive dysfunction (19). Prior to PCDU, however, you might give him a trial of oral PDE5 inhibitors. If those medications are effective, you have effectively ruled out significant arterial insufficiency or venous leakage disease as an etiology. Regardless of outcome of PCDU, no surgical intervention would likely be offered to this man who responds well to oral agents.
If the patient reports life-long erectile dysfunction, having never obtained an erection rigid enough for penetration, he should be assessed with an appropriate laboratory evaluation and PCDU.
If the patient obtains erections in certain situations (self-stimulation) without medication, he does not need additional laboratory or ultrasound assessment. His diagnosis can be made from the history alone.
If the patient requires PDE5 inhibitors to obtain and maintain all erections, you might consider laboratory assessment prior to proceeding.
If the patient reports intermittent ability to obtain and maintain an erection, evaluation with combined injection and stimulation test (CIS) will give you additional diagnostic and potentially therapeutic answers. It will determine if he has adequate inflow to obtain erection and if he has adequate venous occlusive function to maintain erection. It may also provide reassurance to the patient that his anatomy is functional. However, it is well documented that due to increased sympathetic tone these young men will often require additional injection or a separate visit in order to respond appropriately with complete smooth muscle relaxation (7,20,21).
Assessment and plan
In most young men with ED, additional testing to assess for the origin of ED is unnecessary as the history gives you the information that you need. With this said, it may be therapeutic for the patient to know his laboratory assessments are normal, in which case additional testing does add significant value to the assessment. From the history alone, we find that most of these men will have situational erectile dysfunction that responds well to low dose oral PDE-5 inhibitors. If the patient does respond well to these medications, the diagnosis of neurogenic erectile dysfunction, clinically significant arterial insufficiency, or venous-occlusive dysfunction can efficiently be ruled out. If the patient responds inconsistently or does not respond to the oral medications, additional workup should be considered, dependent on the additional history provided.
If the patient reports that PDE 5 inhibitors work poorly or inconsistently, we offer CIS to objectively assess erectile function and to provide diagnostic information. For the CIS, inject bimix (such as papaverine 30 mg/phentolamine 0.5 mg/mL—0.2–0.3 cc) and have the patient compress the injection site for 5 minutes. After 5 minutes, instruct the patient to self-stimulate, then assess his response to injection. One could also combine penile color duplex ultrasound (PCDU) with the CIS. However, PCDU is expensive, may not be covered by the patient’s insurance, and may require increased dosages of pharmacologic agents, such as trimix (papaverine 30 mg/phentolamine 0.5 mg/alprostadil 10 mg–0.5 cc) to obtain complete smooth muscle relaxation. This often requires reversal of erection using phenylephrine after the study. In rare patients who failed to achieve and maintain erection with 0.5 mL of trimix, we may proceed with pharmacologic cavernosography or pharmacologic arteriography depending on the results of PCDU.
Management plan
For patients who have ED related to hypertonic cavernous smooth muscle and excessive sympathetic discharge, we recommend a trial of a low-dose alpha adrenergic blocker, such as terazosin 1 mg PO at bedtime nightly. We typically increase the dosage as needed every 2–3 weeks for 3–5 months until the patient experiences improvement of the erection or we determine that treatment is ineffective. We explain the potential side effects of orthostasis, dizziness, and retrograde ejaculation in detail. We also take great care and time in explaining to the patient, and his family/partner if present, the pathophysiologic mechanism of their erectile dysfunction and the biological basis of the treatment plan. This detailed discussion helps to engage the patient in the treatment plan and provides encouragement regarding the potential for response to treatment and recovery. During these encounters, we utilize teaching tools, such as diagrams, drawings, printed handouts, and other visual aids to ensure that the discussion is patient-focused and patient-friendly. Patient education is critical to exploring treatment options and developing confidence in our ability to treat the ED, and their own ability to overcome and eventually resolve the problem of ED.
If this treatment approach fails, it is useful, however frustrating, to start again from the beginning. Reassess the history to ensure that nothing was missed originally. Obtain labs and perform a PCDU. This will give the objective information that you might need in order to make a diagnosis of a known etiology for ED and to provide the patient reassurance that your evaluation has been thorough.
Brief case presentations
Patient 1
A 19-year-old male presents with a history of anxiety, depression, and asthma and chief complaint of ED that began 1-year ago after a “nerve twinge with subtle pain” during masturbation. He also reports decreased penile sensation since the event. He can obtain and maintain an erection with masturbation. He reports inability to obtain or maintain an erection with a partner unless he takes tadalafil 5 mg. He reports straight phallus, normal libido, orgasm, and ejaculation. The remainder of his history is negative. His physical examination is normal. His previous laboratory assessment, including CBC, CMP, TSH, T4, T and Free T, was normal.
Discussion 1
This man’s situational ED, possibly due to performance anxiety or perhaps fear of a repeat injury and pain. Structural, neurogenic, arteriogenic, and venous occlusive erectile dysfunction can be ruled out as he has normal self-stimulated erections. He responds well to low dose oral PDE5 inhibitors. Additional assessment with cold and hot perception testing and biothesiometer were performed due to his complaint of decreased sensation; both test results were normal. He was started on low dose terazosin once daily at bedtime along with Cialis 5 mg as needed. He is responding well to treatment.
Patient 2
A 25-year-old male presents with a past medical history of mild traumatic brain injury, remote bilateral orchitis, depression, anxiety, and PTSD from childhood bullying. He presents with his mother. His chief complaint is ED that began at 19 years old. He reports that it is "hard to obtain an erection, takes a lot of work to get almost nothing out of it" and “extreme loss of sensation in specific areas” on his penis. He feels that this might be related to “over masturbation without lubricant” 1–3 times per day and reports that he is “addicted to masturbation”, using it as a coping mechanism to manage his PTSD. He reports strong, sustainable erections with tadalafil 5 mg and recovery of sensation when he uses marijuana. He has read extensively on the internet and self-treats with topical vitamin creams, self-administered laser treatment to the penis, pulsed electromagnetic therapy, and hyperbaric oxygen treatment for ED for the past 6 months. He reports no change with any of these treatments. He reports reduced libido and has recently started treatment with HCG and testosterone gel for testosterone of 198 without any change in his symptoms with T of 450. His free T is normal. He lives at home, is unemployed, and is sedentary. He takes Wellbutrin. His physical examination is normal. His CBC, CMP, pituitary, and thyroid functions are normal. Prior to the visit, his mother called the clinic to inform personnel that her son was very sensitive, potentially suicidal, and emotionally disturbed by this problem. He has seen two other urologists already for his erectile dysfunction and been displeased with the outcome of his visits.
Discussion 2
This patient has thoroughly researched erectile dysfunction on the internet and has a powerful knowledge base from which he draws reference. He is also emotionally labile. The most urgent recommendation for this patient is that he seek appropriate psychiatric treatment to help in management of his psychiatric conditions and suicidal ideation. It was also recommended that he seek care with a sexual therapist to work through additional issues related to his “addiction” to masturbation. During his urologic visit we performed both cold and hot perception testing and biothesiometer, which were normal. He was displeased with these findings as they were incongruent with his chief complaints; normal results caused him to become tearful. A penile ultrasound was performed without injection of a pharmacologic agent to assess the appearance of his cavernous tissue and cavernous arteries, which had normal appearance and measurement, respectively, on ultrasound. (This quick bedside procedure has the potential to be both diagnostic and therapeutic for the patient; the importance of this cannot be underestimated).
It was recommended that the patient focus on relaxation techniques, increase cardiovascular exercise, take cialis 5 mg PO prn as it is effective, and to start scheduled terazosin 1 mg po at bedtime to relax the hypertonic cavernous smooth muscle. It was recommended that he utilize lubricants for masturbation, that he decrease the frequency of masturbation, and that he investigate vibrators to increase glanular stimulation if necessary. It was also recommended that he stop using the various alternative therapies that he has been using for the past 6 months (topicals, lasers, electromagnetic therapies, hyperbaric oxygen), which were likely confounding the issue. At follow up, 4 weeks after the initial visit, the patient reported 60% improvement in his symptoms with seldom use of PDE5 inhibitors.
Patient 3
This is a 17-year-old male with a past medical history of insomnia, anxiety and depression who presents with complaints of gradual onset (2 years ago) of decreased ability to obtain and maintain erections adequate for intercourse. He reports normal nocturnal erections “most days of the week”. He does not masturbate because he feels that masturbation may have desensitized his brain and caused ED; however, he can masturbate and have an erection with normal orgasm/ejaculation. He has had a successful erection and intercourse with a partner, last time 2 weeks ago. He feels that his ED might have been associated with SSRI treatment but noted no improvement after stopping his SSRI. Cialis 5 mg is effective. He reports normal libido “but not where it was”. His testosterone (T) and free T are normal. He is in the care of a sexual therapist and has read extensively on the internet. He takes trazodone nightly for sleep.
Discussion 3
This man’s history is adequate to rule out arterial or venous insufficiency as he can masturbate to produce a rigid, sustainable erection and he responds well to tadalafil. Due to his report of gradual onset, his lack of response to ongoing sexual therapy, and his tremendous anxiety associated with the issue, the decision was made to offer a PCDU to assess for a vascular etiology for his disorder. PCDU revealed normal peak flow bilaterally of 40 cm/sec with no end diastolic flow and 100% rigidity obtained. His erection lasted more than 2 hours and required phenylephrine to resolve the erection.
This man was started on terazosin 1 mg PO daily at bedtime and required a dose increase to 2 mg after 1 month. He has seen 70% improvement in his ED and is taking Cialis less often than prior to his visit.
Patient 4
This is a 22-year-old man who presents with no medical or surgical history who reports that he has never had a rigid erection in his life. He reports normal libido, penile sensation, orgasm, and ejaculation. The remainder of his history is negative. His physical examination is normal with normal genital exam and secondary sexual characteristics. He reported no significant change in erection with PDE5 inhibitors.
Discussion 4
A full battery of labs was ordered and returned normal. A PCDU was ordered which revealed normal arterial inflow with velocities greater than >40 cm/sec with increased end diastolic velocities suggestive of venous leak. After pharmacologic erection, he developed a partial erection that resolved within 1 minute. This was consistent with a diagnosis of venous leak impotence. Pharmacologic cavernosography was performed and revealed bilateral crural leakage. He underwent infrapubic bilateral crural ligation of the penis, which cured his ED. The patient returned to clinic 6 months later with recurrent impotence. A pharmacologic cavernosography revealed recurrent venous leak. Additional crural ligation via a perineal approach was performed. Two months later he reported normal penile erections, and the result has lasted for more than 5 years. He continues to follow up annually in clinic.
Conclusions
We are writing this commentary to provide urologists with additional information regarding ED in young men and to open the discussion for new approaches to treatment of ED in young men. Hypertonic cavernous smooth muscle is an organic etiology of erectile dysfunction and should be considered in the differential diagnosis for these young men. Developing a system to explain the pathophysiologic mechanism of the dysfunction may make it easier to effectively treat these complex patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Capogrosso P, Colicchia M, Ventimiglia E, et al. One patient out of four with newly diagnosed erectile dysfunction is a young man--worrisome picture from the everyday clinical practice. J Sex Med 2013;10:1833-41. [Crossref] [PubMed]
- Papagiannopoulos D, Khare N, Nehra A. Evaluation of young men with organic erectile dysfunction. Asian J Androl 2015;17:11-6. [Crossref] [PubMed]
- Cohen SD. The Challenge of Erectile Dysfunction Management in the Young Man. Curr Urol Rep 2015;16:84. [Crossref] [PubMed]
- Sweet G, Shindel AW. AUA Update Series Volume 34: Lesson 1- Erectile Dysfunction in the Younger Man. 2015.
- Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol Clin North Am 2005;32:379-95. [Crossref] [PubMed]
- Diederichs W, Stief CG, Benard F, et al. The sympathetic role as an antagonist of erection. Urol Res 1991;19:123-6. [Crossref] [PubMed]
- Diederichs W, Stief CG, Lue TF, et al. Sympathetic inhibition of papaverine induced erection. J Urol 1991;146:195-8. [PubMed]
- Steers WD. Neural control of penile erection. Semin Urol 1990;8:66-79. [PubMed]
- Kim SC, Oh MM. Norepinephrine involvement in response to intracorporeal injection of papaverine in psychogenic impotence. J Urol 1992;147:1530-2. [PubMed]
- Davidson RJ, Pizzagalli D, Nitschke JB, et al. Depression: perspectives from affective neuroscience. Annu Rev Psychol 2002;53:545-74. [Crossref] [PubMed]
- Ninan PT. The functional anatomy, neurochemistry, and pharmacology of anxiety. J Clin Psychiatry 1999;60 Suppl 22:12-7. [PubMed]
- Althof SE, Needle RB. Psychological factors associated with male sexual dysfunction: screening and treatment for the urologist. Urol Clin North Am 2011;38:141-6. [Crossref] [PubMed]
- Santiago-Lastra Y, Williams BC, Hollingsworth JM. Lesson 40: Dealing with the Difficult Patient Encounter. AUA Update Series 2015. Linthicum, MD: AUA Education and Research, Inc; 2015.
- Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Med Care 1988;26:657-75. [Crossref] [PubMed]
- Lue T. Ch. 23. Philadelphia: Elsevier Inc; 2011. Campbell-Walsh Urology. Physiology of Erection and Pathophysiology of ED.
- Ghanem HM, Salonia A, Martin-Morales A. SOP: physical examination and laboratory testing for men with erectile dysfunction. J Sex Med 2013;10:108-10. [Crossref] [PubMed]
- Miner M, Seftel AD, Nehra A, et al. Prognostic utility of erectile dysfunction for cardiovascular disease in younger men and those with diabetes. Am Heart J 2012;164:21-8. [Crossref] [PubMed]
- Nehra A, Jackson G, Miner M, et al. Diagnosis and treatment of erectile dysfunction for reduction of cardiovascular risk. J Urol 2013;189:2031-8. [Crossref] [PubMed]
- Sikka SC, Hellstrom WJ, Brock G, et al. Standardization of vascular assessment of erectile dysfunction: standard operating procedures for duplex ultrasound. J Sex Med 2013;10:120-9. [Crossref] [PubMed]
- Teloken PE, Park K, Parker M, et al. The false diagnosis of venous leak: prevalence and predictors. J Sex Med 2011;8:2344-9. [Crossref] [PubMed]
- Gontero P, Sriprasad S, Wilkins CJ, et al. Phentolamine re-dosing during penile dynamic colour Doppler ultrasound: a practical method to abolish a false diagnosis of venous leakage in patients with erectile dysfunction. Br J Radiol 2004;77:922-6. [Crossref] [PubMed]


