
The lumbosacral angle is a significant predictor for using a semi-rigid ureteroscopic approach in middle ureteral stones
Introduction
Recently, the widespread use of flexible and semi-rigid ureteroscopes with narrow diameters has improved ureteroscopy (URS) outcomes for urolithiasis(1,2). Many factors influence URS outcome for ureteral stones, including stone size, stone composition, patient background, device availability, and history of extracorporeal shockwave lithotripsy (3-5). Reports on the outcomes of middle ureteral stones are controversial. Some suggest that the stone-free rate for middle ureteral stones is worse than that for upper ureteral stones (6). Middle ureteral stones pose challenges to all surgical stone treatment strategies; the location over the iliac vessels may hinder semi-rigid ureteroscope access. Therefore, the tortuosity of the ureter is significant when considering the approach of ureteroscopy.
In orthopedics, pelvic cavity morphology has been evaluated using indices such as lumbosacral angle (LSA). Many studies have investigated the relationship between pelvic cavity morphology and diseases such as osteoarthritis (7-9). However, to our knowledge, no study has examined the relationship between pelvic cavity morphology and curvature of the ureter as a pelvic organ. Hence, we hope to explore the possibility of using the pelvic cavity’s anatomical parameters to sufficiently predict changes in the ureter’s curvature to predict further the difficulty of approaching the middle ureteral calculus and whether this would improve surgical outcomes. This study evaluated the pelvis in three dimensions and investigated the relationship between the anatomy and potential approach to middle ureteral stones. We present the following study in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-21-1043/rc).
Methods
A retrospective cohort study was conducted at the Hara Genitourinary Hospital, Kobe, Japan, between December 2017 and January 2021. From 967 patients who underwent URS for upper urinary stones, we analyzed 141 with middle ureteral stones, with or without renal stones. Stones located overlying the sacroiliac joint by kidney, ureter, and bladder (KUB) X-ray or computed tomography (CT) were defined as middle ureteral stones (10). Some cases with anatomical malformations such as “retrocaval ureter” and cases in which the stones had spontaneously expelled or had risen to the renal pelvis at the time of surgery were excluded. Cases with ureteral stricture requiring balloon dilatation were also excluded. As a result, 124 patients were finally left in this study. Each patient was evaluated for body mass index (BMI), previous stone treatment, stone size, stone density, American Society of Anesthesiologists score, reachability of the stone, type of ureteroscope, ureteral endoscopic findings at the stone site, time to reach the stone, time until penetrating the stone bed, endoscopic stone-free rate, and complications. In this study, patients with urinary tract infection, back pain, or large stones (>10 mm) were pre-stented and underwent URS within a month. All data were retrospectively collected from a prospective hospital database.
The shape of the pelvic cavity was measured in all the cases as described here: The line connecting the inferior margins of both sacroiliac joints in preoperative KUB X-ray imaging was set to “ab.” The distance of the pelvic cavity parallel to ab was set to the transverse diameter. The vertical line created from the superior margin of the pubic symphysis to ab was put to the vertical diameter (9) (shown in Figure 1A). In the sagittal section of the preoperative non-contrast computed tomography (NCCT) image, the line connecting the sacral promontory angle to the superior point of the pubic symphysis was labeled “cd”. The perpendicular line from the dorsal-most point of the sacrum to the cd was designated as the pelvic depth. In this study, the LSA was defined as the angle between the tangential line to the posterior border of the sacral vertebrae (S) 1 and the posterior endplate of lumbar vertebrae (L) 5 (shown in Figure 1B) (8). All measurements in this study were performed in the supine position. Stone hardness was expressed in mean Hounsfield units. The stone size was measured in the largest dimension on the NCCT image. Measurements were performed by two urologists accordingly. Surgeries were performed by 11 urologists, including senior residents and a surgeon who had experience with at least 1,000 cases of URS. When a resident performed surgery, an expert supervisory physician always instructed them. The surgical procedure is described as follows: First, a safety guidewire (Sensor™, Boston Scientific, USA) was inserted into the ureter, and the tip was guided into the renal pelvis and then fixed. A 6-Fr semi-rigid ureteroscope (Karl Storz, Germany) was routinely performed for optimal dilation without a working guidewire. The lower ureter was not dilated with ureteral dilators before proceeding to semi-rigid ureteroscopy. As the primary endpoint, we evaluated the middle ureteral stone’s reachability using semi-rigid URS. Whether operators continue using semi-rigid URS or place a ureteral access sheath (UAS) and change the scope to a flexible one after that depends on each operator. If the curvature of the ureter prohibited access to the stone, a second guidewire was inserted through the working channel, which served as a working guidewire, and straightened the ureter to reach the stone. If the stone could not be accessed directly with semi-rigid URS, a 9.5-/11.5-Fr (Flexor®, Cook Medical, Bloomington, USA) or a 10-/12-Fr (Uropass®, Gyrus Medical Ltd., Cardiff, UK) or 11-/13-Fr (Navigator®, Boston Scientific, Natick, MA) or 12-/14-Fr (Navigator®, Boston Scientific, Natick, MA) UAS was selected by the feeling any resistance during insertion and placed just below the stone. If UAS was used, the stone was fragmented using a flexible ureteroscope (URF-P7®, Olympus, Tokyo, Japan), achieved with 120-W holmium: YAG laser source (VersaPulse PowerSuite, Lumenis, Yokneam, Israel) with a 200-µm end-firing laser fiber (Slim Line, Lumenis). The laser lithotripter was used at 6–8 Hz, 0.6–0.8 Joule with MOSES™ technology (Lumenis, Yokneam, Israel) or long pulse intermittently on the stone bed for fragmentation. Quarried fragments were removed using a Nitinol basket (N-circle®, Cook Medical). After removing the stone, the ureter was assessed, and we determined whether a 6-Fr ureteral double-J stent should be placed or not accordingly.

Cases in which the stone could be reached by a semi-rigid ureteroscope using a safety guidewire were considered reachable. In contrast, those in which the stone could not be reached by semi-rigid URS or required a working guidewire were considered unreachable. 4.8 Fr semi-rigid ureteroscope was used in some cases not accessible with 6.0 Fr semi-rigid ureteroscope. However, a 4.8 Fr ureteroscope could not be prepared in all cases, so the 6.0 Fr semi-rigid ureteroscope was used to determine the reachability. The time to reach the stone was defined as the time from the ureteroscope passing through the external urethral orifice to reach the stone. The time until penetrating the stone bed was defined as the time that the stone was freed circumferentially from the ureteral mucosa. We retrospectively examined the relationship between the reachability of the middle ureteral stone and anatomical indices and treatment outcomes for the patients.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Hara Genitourinary Hospital (No. 20201119-2) and individual consent for this retrospective analysis was waived.
Statistical analysis
Logistic regression analysis was performed on the four aforementioned anatomical variables to determine the significant predictors of reachability. Receiver operating characteristic (ROC) curves were created for significant risk factors, cutoff values were established, and the calculated cutoff values were used to divide the entire population into two groups. The Mann-Whitney U and Chi-square tests were used to analyze the differences accordingly. All statistical analyses were conducted using EZR (Saitama Medical Center, Jichi Medical University, Japan). P<0.05 was considered statistically significant and missing values were omitted from the analysis.
Results
The patients’ clinical characteristics are summarized in Table 1. Middle ureteral stones in 60.6% of the cases were reachable. The proportion of female patients was higher in the reachable group (44.2%) than in the unreachable group (23.4%) (P=0.022). The median age of the patients was 63 [24–81] years in the reachable group and 57 [33–92] years in the unreachable group. In reachable and unreachable groups, the median BMI was 24.7 (14.3–48.1) kg/m2 and 23.8 (17.3–41.9) kg/m2. Most patients had an ASA score of 1. A preoperative double-J stent was placed in 48 (65.8%) patients in the reachable group and 19 (40.4%) patients in the unreachable group (P=0.008).
Table 1
| Parameter | Patients with middle ureteral stone | P value | |
|---|---|---|---|
| Reachable Pt (n=77) | Unreachable Pt (n=47) | ||
| Age, median yr | 63 [24–81] | 57 [33–92] | 0.411 |
| Sex | 0.022* | ||
| Male, n (%) | 43 (55.8) | 36 (76.6) | – |
| Female, n (%) | 34 (44.2) | 11 (23.4) | – |
| BMI | 24.7 (14.3–48.1) | 23.8 (17.3–41.9) | 0.311 |
| Stone laterality, n (%) | 0.355 | ||
| Right | 42 (54.5) | 21 (44.7) | – |
| Left | 35 (45.5) | 26 (55.3) | – |
| Previous stone treatment, n (%) | – | ||
| Shockwave lithotripsy | 16 (21.9) | 5 (10.6) | 0.143 |
| Ureteroscopy | 5 (6.8) | 4 (8.5) | 0.736 |
| Percutaneous nephrolithotomy | 0 | 2 (4.3) | 0.151 |
| Open surgery | 0 | 0 | – |
| Stone size, median mm | 7.0 (2–18) | 7.0 (4.3–20) | 0.767 |
| CT values, median Hounsfield unit | 1,050 (114–1,946) | 1,040 (497–1,634) | 0.623 |
| Preoperative double-J stent, n (%) | 48 (65.8) | 19 (40.4) | 0.008* |
| ASA score, n (%) | 0.713 | ||
| 1 | 67 (91.8) | 45 (95.7) | – |
| 2 | 4 (5.5) | 2 (4.3) | – |
| 3 | 2 (2.7) | 0 | – |
| Anticoagulation, n (%) | 1 (1.4) | 1 (2.1) | 1 |
*P<0.05. BMI, body mass index, CT, computed tomography, ASA, American Society of Anesthesiologists.
The preoperative and perioperative parameters are shown in Table 2. Treatment with only semi-rigid URS was administered to 18 (23.4%) patients in the reachable group. Both scope types were used in 59 (76.6%) and 47 (100%) patients in the reachable and unreachable groups. Distal ureteral orifice stenosis was observed in 5 (6.6%) and 12 (26.1%) patients in the reachable and unreachable groups, respectively (P=0.005). The median pelvic vertical diameter was 9.09 (4.67–13.10) cm and 8.78 (6.97–11.58) cm, the median pelvic transverse diameter was 14.23 (12.51–16.66) cm and 13.86 (9.85–15.67) cm , the median pelvic depth was 9.89 (7.62–11.78) cm and 9.68 (7.83–12.29) cm , and the median LSA was 150.65° (125.73–172.16) and 143.74° (128.46–160.67) (P=0.020) in the reachable and unreachable groups, respectively. We examined whether there was a difference in LSA by gender, but there was no significant difference (128.46 in males vs. 125.73 in females: P=0.175).
Table 2
| Parameter | Patients with middle ureteral stone | P value | |
|---|---|---|---|
| Reachable Pt (n=77) | Unreachable Pt (n=47) | ||
| Pelvic cavity, cm (%) | |||
| Pelvic transverse diameter | 14.23 (12.51–16.66) | 13.86 (9.85–15.67) | 0.267 |
| Pelvic vertical diameter | 9.09 (4.67–13.10) | 8.78 (6.97–11.58) | 0.303 |
| Pelvic depth | 9.89 (7.62–11.78) | 9.68 (7.83–12.29) | 0.469 |
| Lumbosacral angle | 150.65 (125.73–172.16) | 143.74 (128.46–160.67) | 0.020* |
| Type of ureteroscopy, n (%) | <0.001* | ||
| Semi-rigid | 18 (23.4) | 0 | – |
| Semi-rigid + Flexible | 59 (76.6) | 47 (100.0) | – |
| Ureteral findings at the site of the stone, n (%) | |||
| Edema | 60 (80.0) | 31 (67.4) | 0.292 |
| Polyps | 22 (28.9) | 15 (32.6) | 0.57 |
| Kink of ureter | 9 (11.7) | 10 (21.3) | 0.12 |
| Distal ureteral orifice stenosis, n (%) | 5 (6.6) | 12 (26.1) | 0.005* |
*P<0.05.
Our analysis regarding predictors of the reachability of middle ureteral stones is shown in Table 3. Multivariate analysis was performed for the four items that were significantly different in the univariate analysis for reachability: sex, presence of double-J stenting, presence of ureteral stenosis, and LSA. Logistic regression analysis indicated that LSA and female sex were significant predictors of a semi-rigid ureteroscopic approach to middle ureteral stones (odds ratio =1.08; 95% CI: 1.03–1.14; P=0.003, and odds ratio =3.23; 95% CI: 1.12–9.32; P=0.03, respectively). The cutoff value of the LSA was 149.9°, with a sensitivity of 55.1% and specificity of 72.7% (shown in Figure 2). In general, males have a prostate grand and longer urethra than females and have a narrower pelvis. Their differences may lead to the results of semi-rigid reachability. Multivariate analysis separately by genders showed that LSA was associated with reachability only in the male (odds ratio =1.09; 95% CI: 1.03–1.16; P=0.005, shown in Table 4).
Table 3
| Parameter | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Sex (Female) | 3.23 | 1.120–9.320 | 0.03* |
| Preoperative double-J stent | 2.2 | 0.826–5.880 | 0.114 |
| Lumbosacral angle | 1.08 | 1.030–1.140 | 0.003* |
| Distal ureteral orfice stenosis | 0.36 | 0.077–1.650 | 0.187 |
*P<0.05.
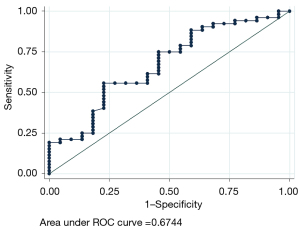
Table 4
| Parameter | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Male | |||
| LSA | 1.09 | 1.03–1.16 | 0.005* |
| Double-J stent | 1.71 | 0.54–5.40 | 0.356 |
| Ureteral orifice stenosis | 0.887 | 0.29–2.70 | 0.832 |
| Female | |||
| LSA | 1.04 | 0.92–1.17 | 0.545 |
| Double-J stent | 2.92 | 0.30–28.4 | 0.356 |
| Ureteral orifice stenosis | 0.01 | 0.00–inf | 0.994 |
*P<0.05. LSA, lumbosacral angle.
The treatment outcomes are shown in detail in Table 5. Patients were divided into two groups according to whether their LSA was ≥150° (group 1) or <150° (group 2). There was no significant difference in the total operative time or time until penetrating the stone bed between the two groups. However, the time to reach the stone in Group 2 was longer than in Group 1 (P=0.049). The endoscopic stone-free rate in group 1 was 84.8%, which was not statistically significant compared to group 2 (86.0%, P=1.00). A double-J stent was placed postoperatively in 82.6% and 85.7% of the patients in groups 1 and 2, respectively. Of all the patients, 6.5% developed ureteral trauma after the procedure (0% in group 1 and 7.1% in group 2). In these cases, double-J stenting was performed, and no stricture occurred later (Clavien-Dindo Classification III). 36.4% of all patients developed renal colic (Clavien-Dindo Classification I: 29.0% in group 1 and 38.5% in group 2). It happened by the following day in most cases. Moreover, the use of UAS or double-J stent did not affect the occurrence of colic (P=1.00 and P=0.567, respectively). No ureteral avulsion or perforation was observed in this study. No statistical difference was found in the complication rates between the two groups.
Table 5
| Parameter | Total | Group 1 | Group 2 | P value | |
|---|---|---|---|---|---|
| LSA ≥150° | LSA <150° | ||||
| Time to reach the stone, median sec | 256.5 (40–1,830) | 245.5 (40–1,170) | 362 (90–1,830) | 0.049* | |
| Time until penetrating the stone bed, median min | 15 (2–125) | 13.5 (2–95) | 19 (3–125) | 0.129 | |
| Endoscopic stone free, n (%) | 110 (87.3) | 39 (84.8) | 49 (86.0) | 1 | |
| Postoperative double-J stent, n (%) | 105 (85.4) | 38 (82.6) | 48 (85.7) | 0.786 | |
| Perioperative complications, n (%) | – | ||||
| Ureteral avulsion | 0 | 0 | 0 | – | |
| Ureteral trauma | 8 (6.5) | 0 | 4 (7.1) | 0.125 | |
| Postoperative complications, n (%) | – | ||||
| Renal colic | 36 (36.4) | 9 (29.0) | 20 (38.5) | 0.478 | |
| Fever (>38.0) | 9 (7.2) | 3 (6.5) | 6 (10.7) | 0.508 | |
| Blood transfusion | 0 | 0 | 0 | – |
*P<0.05. LSA, lumbosacral angle.
Discussion
Our study produced two crucial clinical observations. First, gradual LSA and females were significant positive predictors of the possibility of a semi-rigid ureteroscopic approach to middle ureteral stones. Second, the operative time to reach the stone was longer in the LSA <150° group than in the LSA ≥150° group.
In this study, we defined those cases as reachable in which the middle ureteral stone could only be reached with a safety guidewire because lasers cannot be used in situations where a working guidewire is used to reach the stone. Moreover, especially in the middle ureter, even if the stone is visualized with a working guidewire through semi-rigid URS, laser-firing cannot be performed because of the ineffective irrigation and poor visualization in the absence of a working guidewire. There are many cases in which laser-firing is possible using two channels, even using a working guidewire. However, since the main object of this study was to investigate the relationship between pelvic anatomy and ureteral tortuosity, we considered that reaching the stone using an additional guidewire would not be significant. More, in our hospital, we use a 6-Fr ureteroscope with a one-working channel. We do not use the two working channel URS because it is larger in diameter and increases the risk of ureteral injury. The lower reachability in patients without preoperative double-J stent or with ureteral orifice stenosis was expected in this study because the dilated ureter or ureteral orifice makes the insertion and manipulation of the endoscope easier. However, the finding that LSA contributes to reachability especially in male cases is an essential observation in this study. The larger the LSA, the closer the angle of the sacrum to the L5 approximates the horizontal, the more likely it is that a semi-rigid ureteroscope could reach the stone. We hypothesized that in cases with a larger LSA, the dorsal curvature of the lower ureter would be less pronounced, making it easier to reach the stone using a semi-rigid ureteroscope. Although a semi-rigid ureteroscope is often used in transurethral lithotripsy for upper ureteral stones, many anatomical situations render the upper ureter inaccessible. High-grade hydronephrosis is an important factor as it affects ureteral tortuosity. In our institution, all patients with preoperative hydronephrosis undergo ureteral stenting, so basically, the hydronephrosis disappears before surgery. However, 4 cases of patients with grade 3 or higher hydronephrosis could not be stented. Of these, the reachability of semi-rigid ureteroscope was 50%, and the average time to reach the middle ureteral stone was 152.3 seconds, which was shorter than the overall average. The significantly higher proportion of women in the reachable group in the multiple variable analysis may suggest a larger pelvic cavity or inclination. A lower ureteral muscle tone and mobility of the bladder and urethra can influence the ease of procedure in the female. The male prostatic urethra and well-developed iliopsoas muscles may also have a negative influence (11). To take into account the effect of benign prostatic hyperplasia, we divided the men into two groups: those over 60 years old and those under 60 years old, but there was no significant difference in reachability (P=0.363, unshown data). Although prostate volume was not measured in this study, the data was informative.
In the ROC curve for the LSA, the LSA cutoff value was 149.9°; therefore, we divided the patients into two groups to examine the surgical outcomes. The results showed a significant difference in the time taken to reach the stone between the two groups. This was because group 1 included many cases that could be reached only with a semi-rigid ureteroscope. Hence, the time required for instrument replacement or UAS placement was short. Even when using UAS, the ureter had a gentle tortuosity, so it could easily reach the stone in group 1. The AUC was not so high (0.674, shown in Figure 2), and there were no differences in other perioperative outcomes between the two groups, so the results need to be interpreted carefully. However, we consider that a short time to reach the stone has a positive effect on reducing the risk of infection and a longer time for effective laser-firing in URS. Because of the small number of cases, multivariate analysis did not show a significant difference in the incidence of complications between the two groups, which is a limitation of the present study.
Urologists often perform semi-rigid URS of the middle ureter and encounter resistance, which may present a significant risk (22%) of ureteral stricture development (12). Pre-stenting can resolve this, enabling passive ureteral dilation (13); however, we cannot place a ureteral double-J stent in every case. Therefore, even though smaller ureteroscopes may improve the upper urinary tract access, preoperative LSA measurement can help decide the type of ureteroscope to be used and strategies to be applied to ensure a good field of view especially in male cases. LSA measurement was straightforward and reproducible. Even when different urologists measured it, the error was within about 5 degrees in the present study. This also has the advantage of reducing the time required for intraoperative decision-making and reducing damage to the ureteroscope caused by forceful access to the tortuous ureter. The findings of the pelvic bone in KUB or CT are reproducible. They can be performed non-invasively, which is also the advantage of these procedures. Perez Castro et al. (1) reported that the stone-free rate in patients with middle ureteral stones treated with semi-rigid URS was higher (90.2%) than with flexible URS (80.9%), indicating that semi-rigid URS is also safe and effective (14,15) in proper cases. For middle ureteral stones, it would be advantageous to predict whether they can be treated with a semi-rigid ureteroscope alone.
In this study, as trainees were involved in many cases as a surgeon, we conducted an additional study to see if there was a difference between results performed by trainees and results performed by experienced urologists. Urologists with experience of fewer than 100 cases of URS were defined as a trainee. However, there was no significant difference in the reachability even when the presence of trainee was included as a variable (Logistic regression analysis, odds ratio =0.963; 95% CI: 0.34–3.04; P=0.948). When limited to cases of middle ureteral stones alone, there was a total of 36 cases in this study. However, there was no significant difference in the operative time between the two groups. Further studies are needed to collect single middle ureteral stones to compare surgical outcomes in the future accurately. Moreover, there may be other anatomical factors that are easier to measure and relevant to URS outcomes.
This study has some limitations. First, it was a single-center retrospective study. Second, individual differences in the ureteral diameter were not considered in the study. Third, there was a significant difference in time to reach the stone statistically, though it is unclear how clinically beneficial this is to patients. However, we believe that adequate preparation by preoperative LSA measurement will lead to patient benefit potentially especially in male patients with narrow pelvises.
Conclusions
In conclusion, this study is the first to suggest that gradual LSA and female sex are significant predictors of the possibility of a semi-rigid ureteroscopic approach for middle ureteral stones. Moreover, the time to reach the stone is longer in patients with LSA <150° than in those with LSA ≥150°. In addition to the operative procedure and the patient’s underlying diseases, we suggest that imaging factors could offer beneficial information regarding the difficulty of approach in patients considering surgical treatment for middle ureteral stones.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-21-1043/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-21-1043/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-21-1043/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-21-1043/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Hara Genitourinary Hospital (No. 20201119-2) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Perez Castro E, Osther PJ, Jinga V, et al. Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol 2014;66:102-9. [Crossref] [PubMed]
- Kozyrakis DG, Kratiras ZK, Perikleous SK, et al. How Effective Is Retrograde Semirigid and Flexible Ureteroscopic Lithotripsy for the Treatment of Large Ureteral Stones Equal of or Greater than 15 mm? Results from a Single Center. Urol Int 2019;103:74-80. [Crossref] [PubMed]
- Reddy SVK. Ureteroscopic Lithotripsy; Retrospective Review of Mid and Lower Ureteric Stones- its Results and Complications. UNOAJ [Internet] 2016 Mar 5 [cited 2020 Sep 2];3(2). Available online: https://medcraveonline.com/UNOAJ/ureteroscopic-lithotripsy-retrospective-review-of-mid-and-lower-ureteric-stones--its-results-and-complications.html
- Almusafer M, Jawad Al-Tawri A. Complications of ureteroscopic stone lithotripsy: A multicentre local study. Hamdan Med J 2019;12:119. [Crossref]
- Chew BH, Zavaglia B, Paterson RF, et al. A multicenter comparison of the safety and effectiveness of ureteroscopic laser lithotripsy in obese and normal weight patients. J Endourol 2013;27:710-4. [Crossref] [PubMed]
- Mursi K, Elsheemy MS, Morsi HA, et al. Semi-rigid ureteroscopy for ureteric and renal pelvic calculi: Predictive factors for complications and success. Arab J Urol 2013;11:136-41. [Crossref] [PubMed]
- Onyemaechi NO, Anyanwu GE, Obikili EN, et al. Impact of overweight and obesity on the musculoskeletal system using lumbosacral angles. Patient Prefer Adherence 2016;10:291-6. [Crossref] [PubMed]
- Amonoo-Kuofi HS. Changes in the lumbosacral angle, sacral inclination and the curvature of the lumbar spine during aging. Acta Anat (Basel) 1992;145:373-7. [Crossref] [PubMed]
- Doiguchi Y, Iwasaki K, Yamada K, et al. Correlation between Pelvic Inclination and Radiological Shape of the Pelvic Cavity. Orthopedics & Traumatology 1992;41:641-5. [Crossref]
- Jendeberg J, Geijer H, Alshamari M, et al. Size matters: The width and location of a ureteral stone accurately predict the chance of spontaneous passage. Eur Radiol 2017;27:4775-85. [Crossref] [PubMed]
- Sung JC, Springhart WP, Marguet CG, et al. Location and etiology of flexible and semirigid ureteroscope damage. Urology 2005;66:958-63. [Crossref] [PubMed]
- De Coninck V, Keller EX, Somani B, et al. Complications of ureteroscopy: a complete overview. World J Urol 2020;38:2147-66. [Crossref] [PubMed]
- Osther PJS. Risks of flexible ureterorenoscopy: pathophysiology and prevention. Urolithiasis 2018;46:59-67. [Crossref] [PubMed]
- Turkan S, Ekmekcioglu O, Irkilata L, et al. Is semirigid ureteroscopy sufficient in the treatment of proximal ureteral stones? When is combined therapy with flexible ureteroscopy needed? Springerplus 2016;5:30. [Crossref] [PubMed]
- Alameddine M, Azab MM, Nassir AA. Semi-rigid ureteroscopy: Proximal versus distal ureteral stones. Urol Ann 2016;8:84-6. [Crossref] [PubMed]


