
Bilateral ileal ureter substitution for patients with ureteral strictures secondary to gynecological tumors radiotherapy: a multi-center retrospective study
Introduction
Radiotherapy represents an important therapeutic component in the management of many gynecologic malignancies, which can be employed as primary treatment, or neoadjuvant, or adjuvant therapy. Radiotherapy is indicated in up to 60% of cervical cancer patients, 45% of endometrial cancer patients, 35% of vulvar cancer patients, 100% of vaginal cancer patients, and 5% of patients with ovarian cancer (1). However, the surrounding normal tissues usually receive some of the doses. The incidence of ureteral stricture was reported to be 1.0%, 1.2%, 2.2%, 2.5%, and 3.3% at 5, 10, 15, 20, and 25 years after radiation, respectively (2).
Patients with ureteral strictures may suffer from flank pain, dilation of the upper urinary tract, and deterioration of renal function. Due to the influence of gynecological tumors and the fragility of tissues after radiotherapy, ureteral injury is difficult to manage. A percutaneous nephrostomy or indwelling ureteral stents was usually used to relieve hydronephrosis (3,4). However, percutaneous nephrostomy or the insertion of ureteral stents could not only impair the quality of life but also lead to infection, stones, and even deterioration of renal function (5).
Bilateral ureteral stricture caused by pelvic radiotherapy is more complicated and more difficult to deal with. Although ureter reconstruction is a definitive option, it is limited by the surgical complexity and adhesions or tissue degeneration caused by radiation (6,7). Radiation-induced bilateral ureteral stricture often occurs at 4–6 cm proximal to the ureteric orifice (4). Ureteroureterostomy or ureteroneocystostomy is not suitable for reconstruction because of excessive tension of the anastomosis. The use of psoas hitch or Boari flap is also limited because the capacity of the bladder is insufficient for a Boari flap, especially in combination with radiation cystitis or contracted bladder (7,8).
Using bowel segments for ureteral reconstruction is a promising option. However, possibly due to the presence of bowel adhesion and the risk of tumor recurrence, there is limited literature on bilateral ileal ureter substitution secondary to radiotherapy (7,9-12). The present study aims to analyze the characteristics of radiation-induced ureteral strictures and summarize our experience with bilateral ileal ureter substitution. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tau-21-255).
Methods
Patients
From June 2010 to June 2019, 18 patients treated by bilateral ileal ureter substitution were enrolled. The demographics, gynecological cancer histories, laboratory data, imaging studies, perioperative data, and follow-ups were recorded. All patients were consecutively and preoperatively diagnosed with bilateral ureteral strictures. The diagnosis was made based on subjective criteria, such as flank pain, pyelonephritis, and the radiological criteria including retrograde urography or antegrade + retrograde urography, computed tomography urography (CTU), and diuretic renography. Time of ureteral strictures was defined as the interval from the last radiotherapy to the discovery of symptoms or abnormal imaging examination and was categorized as short-term (less than 12 months) and long-term (over 12 months). The main surgical indication for bilateral ileal ureter substitution was patients with bilateral long or multiple ureteral strictures, which cannot be treated simply by ureteroureterostomy, ureteroneocystostomy, or Boari flap, and the patients had one of the following conditions: (I) intolerance to ureteral stents (9 cases); (II) deterioration of the renal function after indwelling ureteral stent (3 cases); (III) recurrent urinary tract infection with ureteral stents or nephrostomy tubes (1 case); (IV) patients’ willingness (5 cases). The surgical indications for augmentation ileocystoplasty included (I) irritation symptoms of bladder; (II) a bladder volume less than 100 mL in the urodynamic study. Exclusion criteria included (I) elevated serum creatinine above 1.5 mg/dL; (II) bowel disease; (III) tumor recurrence; (IV) intolerance to surgery. Complications were evaluated by the Clavien-Dindo classification system (13). This study was approved by the ethics committee of our hospital (No.: 2020-SR-283). Informed consent was obtained from all participants. All research procedures were conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Surgical technique
Polyethylene glycol electrolytes were taken to clean the intestines, and enteral nutrition emulsions were consumed to ensure a scum-free diet the day before surgery. The patient was placed in a supine position after general anesthesia. A midline incision and splitting of the bilateral line of Told were performed to expose both ureters. The level of the healthy ureter was judged by observing whether the urine can flow out of the ureteral stump smoothly. Intraoperative indocyanine green fluorescent imaging could help determine the level of the healthy ureter in difficult cases. The ureter proximal to the injury site or the renal pelvis was spatulated for subsequent anastomosis. A 20–30 cm ileal segment was removed at least 15 cm away from the ileocecal valve after measuring the ureter defect length. Small intestine continuity was restored with side-to-side anastomosis using a linear stapler. There was a reverse “7” configuration in all patients (Figure 1), in which the internal ureteral stents were placed. Usually, the bowel goes above the inferior mesenteric artery through the left colonic mesentery (Figure 2A). The left ureter/renal pelvis and ileal graft were anastomosed end-to-end by continuous suture with 4-0 barbed suture, while the right ureter was anastomosed end-to-side on the same ileal graft. The terminal ileal graft was turned up about 2 cm to form an anti-reflux nipple by full-thickness- seromuscular suture (Figure 2B). We performed the ileocystostomy in a two-layer fashion, with successive mucosa-to-mucosa sutures and intermittent seromuscular-detrusor muscle sutures.
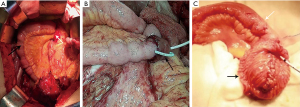
Normal saline was used to fill the bladder for further confirmation of the bladder capacity during the operation in suspicious patients, and augmentation ileocystoplasty was performed simultaneously in proper patients. After the fibrotic bladder wall around the bladder dome was opened, the distal ileal segment was incised on the antimesenteric border and oversewed in a “U” shape. The distal segment was then subsequently sutured into a hemi-pouch for augmentation cystoplasty. Afterwards, the mucosa of the hemi-pouch was sutured to the dissected bladder wall (Figure 2C). In addition, we only tried to loosen the tissues around the bladder during the operation, namely “autologous augmentation”, for patients with a bladder volume greater than 100 mL but less than 200 mL.
The ERAS protocol includes (I) analgesia: constant speed epidural analgetic pump and NSAIDs; (II) symptomatic treatment of nausea and vomiting; (III) liquid diet after flatus, and gradually resume full diet.
Follow-up
The follow-ups of patients were performed at 1, 3, and 6 months after surgery and at least twice a year afterwards. The patients regularly received symptoms evaluation, physical examinations, bimanual examination, urine routine test, blood tests (including serum creatinine, tumor markers, electrolyte test, and blood gas analysis), and transvaginal ultrasound at each visit. Cystoscopy is performed 1 month after the surgery when removing the ureteral stent. Radiographic examinations including CTU/functional cine magnetic resonance urography (MRU) were performed every 6 months. Surgical success was defined as no restenosis, relief of symptoms, no deterioration of hydronephrosis.
Statistical analysis
All analyses were performed with SPSS® Statistics, version 20.0. The Kolmogorov-Smirnov test was used to check whether the data were normally distributed. The independent sample t-test was used for continuous variables. The chi-square test or the Fisher’s exact test was used for categorical variables. The rank-sum test was used for non-normal distributions. A two-sided value of P<0.05 was considered to indicate statistical significance. A line chart of creatinine and eGFR for each patient was used to trend the renal function before and after the surgery. The hydronephrosis-free survival and renal-impairment-free survival outcomes were analyzed by Kaplan-Meier analysis.
Results
Baseline characteristics
A total of 18 female patients with bilateral ureteral strictures caused by radiotherapy underwent ileal ureter substitution. The mean age of the patients was 46.6±8.4 years. All the patients had a history of gynecological tumor, including cervical cancer (15, 83.3%) or endometrial cancer (3, 16.7%). The stages of cervical cancer ranged from IA to IIA, and endometrial cancers were from I to II. The tumors were treated by radical hysterectomy ± bilateral salpingo-oophorectomy, and adjuvant radiotherapy was applied after surgeries. There was no sign of recurrence. The patients had been suffered from bilateral ureteral strictures for a median of 12 (2–106) months. The strictures were located on the lower or mid-lower ureter. The mean length of the left ureteral stricture was 9.6±2.6 cm, and the mean length of the right ureteral stricture was 8.8±3.2 cm. Symptoms included flank pain (9, 50.0%), fever (1, 5.6%), anasarca (1, 5.6%), and 7 patients (38.9%) were found hydronephrosis during periodic review without any complaints. In addition, no patients had bowel-related symptoms. All patients had a history of indwelling double-J ureteral stents, and uni- or bilateral percutaneous nephrostomy had been indwelled for 9 [2–30] months before surgery. The detailed characteristics and history of radiotherapy were shown in Table 1.

Full table
Peri-operative information
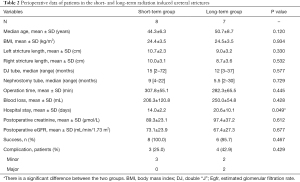
All the patients underwent bilateral ileal ureter substitution successfully, with 4 patients simultaneously receiving augmentation ileocystoplasty due to a small bladder capacity. The mean length of the ileal graft was 29.1±7.4 cm. The mean operative time was 308.4±70.2 min, and the mean estimated blood loss was 254.7±166.2 mL, without blood transfusion during operation. The median postoperative length of stay was 15 d (range, 9–93 d). The comparative outcomes of the short-term group and the long-term group were shown in Table 2. The postoperative hospital stays in the short-term group were significantly shorter than those in the long-term group (14.0 vs. 20.6 days, P=0.049). There were no significant differences in the stricture length, the indwelling time of preoperativeureteric stents or nephrostomy tubes, the operation time, the estimated blood loss, or the postoperative renal function (Table 2). Intraoperative complications occurred in 1 patient. In this case, the sigmoid colon was damaged when separating the adherent intestine tube, and the general surgeon performed a one-stage suture repair.
Full table
Follow-up
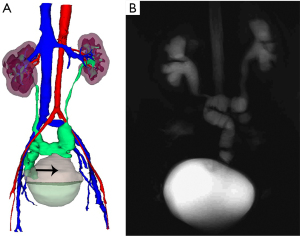
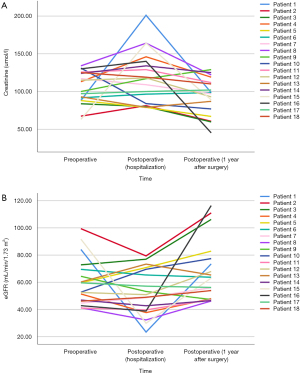
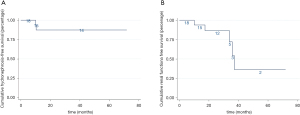
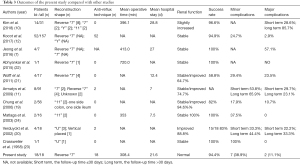
During a median follow-up time of 24.1 (4.5–71.9) months, the surgical success rate was 94.4%. Postoperative radiological upper tract images demonstrated that there was no evidence of obstruction in any patient (Figure 3A,B). Both left and right sides of hydronephrosis were relieved than before. Functional cine MRU showed resolution of preoperative hydronephrosis and good peristalsis in the ileal graft (Video 1). No stenosis of the anti-reflux nipple was observed under the cystoscope (Video 2). The mean pre- and post-operative creatinine were 107.7±26.7 and 97.8±30.7 µmol/L, respectively. The mean pre- and post-operative eGFR were 59.1±18.6 and 66.9±24.3 mL/min/1.73 m2, respectively. The line chart of creatinine and eGFR for each patient was shown in Figure 4. All the patients had stable renal function. The long-term hydronephrosis-free survival and renal-impairment-free survival outcomes were shown in Figure 5.
Regarding the postoperative complications, 8 minor complications (grade ≤2) were developed in 5 patients. Urinary tract infections (4/18, 22.2%) were the most common complications, followed by ileus (3/18, 16.7%). One patient was found to have a urine leak and recovered by conservative treatment. Major complications (grade ≥3) accounted for 2 out of all patients. One patient suffered from a fistula 10 days after surgery, though intraoperative repair for sigmoid injury was performed. However, the patient had abdominal pain caused by a colonic fistula. Thus, the patient was treated with colostomy and was cured with a hospital stay of 93 days. The other patient suffered from a pulmonary embolism and recovered after hemodynamics and respiratory support and anticoagulation therapy.
Discussion
Radiotherapy is a widely used treatment in gynecological tumors. For cervical cancer, primary radiotherapy for early-stage cervical cancer has an oncology outcome that is indistinguishable from surgery (14). In addition, adjuvant radiotherapy for mid-risk to high-risk cervical cancer can reduce the risk of disease progression (15). For mid-risk to high-risk endometrial cancer, adjuvant radiotherapy can reduce the risk of local recurrence (16). However, even though great efforts have been taken to adjust the target area of radiotherapy, it will inevitably affect normal tissues. Radiation induces apoptosis of ureteral cells with inflammation, which will eventually cause ureteral scars and lumen stenosis.
The treatment of radiation-induced ureteral stricture is complicated, and bilateral ureteral stricture is more difficult to deal with. Since radiogenic injury to ureters is irreversible and progressive, drainage with nephrostomy tubes or long-term ureteral stents should be permanent. In this long-term conservative treatment process, many complications may be inevitable, such as infection, inadequate relief of obstruction, irritative bladder symptoms, and suprapubic and loin pain (5). Surgical reconstruction can provide an alternative, permanent treatment to improve patients’ quality of life. Traditional reconstructive strategies, such as ureteroureterostomy, ureteroneocystostomy, psoas hitch, and Boari flap, require sufficient length of the ureter or sufficient bladder capacity. The inflammatory exudation and fibrosis caused by radiotherapy increase the complexity of surgery, and it is difficult to meet the principle of tension-free anastomosis.
The use of ileal segments for ureter reconstruction was first reported by Shoemakers in a patient with urinary tuberculosis in 1906 (17), and it became an accepted procedure in the late 1950s (18). For bilateral ureteral stricture, several configurations of ileal graft were designed to bridge the ureteral stump and bladder, such as “7”, “11”, “Y”, and “U” (10-12,19-22). “U” shaped ileum remained a problem that one side of the intestine was antiperistaltic (23). “11” and “Y” configurations required two segments of ileum, thus, blood supply and mesangial tension caused difficulty on surgery (24). The “7” configuration and reverse “7” configuration could achieve bilateral peristaltic anastomosis (11). Accordingly, the reverse “7” configuration was applied for most cases of bilateral ileal ureter substitution.
Compared with the results of previous studies (Table 3), we reported a considerable success rate of bilateral ileal ureter for long ureteral strictures secondary to radiotherapy, with a low complication rate. Hydronephrosis was significantly relieved in all cases. No patients needed further management or suffered renal insufficiency. Our promising results were established in proper preoperative evaluation and selection. Ruling out the possibility of recurrence and metastasis in gynecological tumors before reconstruction was essential at first. In our patients, no gynecological tumors infiltrated outward in terms of tumor staging. Regular reexamination indicated no recurrence or distant metastasis occurred in all patients after tumor resection. In addition, it is noteworthy that patients should have a good and stable preoperative renal function (19,20). Previous studies discussed that the creatinine threshold before ileal ureter replacement ranged from 1.7–2.0 mg/dL (19,21,25). The ileal graft selected for the bilateral ureteral substitution was longer, which may cause an easier postoperative metabolic problem. We set the criteria as the creatinine should not be higher than 1.5 mg/dL. Patients who did not meet the requirements of creatinine were recommended to indwell ureteral stents or nephrostomy tubes to relieve renal function. Furthermore, comparing to ureteral stents, we recommended nephrostomy for 3 months, ensuring enough ureteric rest before reconstruction.
Full table
Radiation-induced ureteral injuries have different characteristics in different periods. In the short term, pathological changes manifest mainly as inflammatory exudation, and in long-term it is mainly fibrosis (26). We found that short-term ureteral strictures were mostly detected by re-examination, and long-term ureteral strictures were mostly found by the complaints caused by long-lasting hydronephrosis. For this reason, patients in the short-term group firstly tended to adopt conservative drainage methods to observe the effect, while those in the long-term group underwent surgical treatment as soon as the condition improved after urine drainage. Thus, the long-term group had a shorter time on nephrostomy and DJ stents on the contrary. No difference in operation time or blood loss was observed. We think the possible reason was that the experienced surgeon had rich experience in reconstructive surgery, which covered up the impact of acute exudation and chronic fibrosis on surgery. However, the longer strictures and difficulty in the determination of the healthy ureters in the short-term group would result in a little longer operation time, without significant difference. A small number of cases may also produce bias. The short-term group allowed for a quicker recovery from surgery. The reason may be that the three complications in the long-term group lengthened the hospital stay. Therefore, although there was no significant difference in the surgical success rate, complications, and postoperative renal function, we proposed to review patients with pelvic radiotherapy regularly to detect and treat hydronephrosis as early as possible.
The reverse “7” configuration for bilateral ileal ureter substitution was recommended because it corresponds to the natural anatomy and reduces the risk of mesenteric torsion. At the same time, a reverse “7” configuration allowed the ileal ureter to mimic the natural ureteral isoperistaltic movement, not only playing a role in anti-reflux activities but also shortening the duration of urine in the intestine (11). What needs to be emphasized is that the ileum used must be a non-radiated segment. The length of the ileal graft was not limited, and it can be adjusted according to the complicated intraoperative situation. We recommended that the appropriate ileum should be selected from far and near for patients who may have an intestinal injury due to radiotherapy. The colon should be considered as a substitute if needed. Urinary diversion is not recommended because of low quality of life and stoma-related complications. In addition, radiotherapy can result in severe pelvic adhesions, fragile tissues, and easy bleeding. A continuous ileal segment helped minimize the number of anastomoses, reduce blood loss and lower the risk of anastomotic stenosis and urinary fistulas.
It is more complicated when radiation-induced ureteral strictures combined with bladder contracture. Radiation damage is degradation and subsequent remodeling of the connective tissue matrix, which leads to radiation-induced fibrosis (27). The decrease in bladder capacity brings about symptom distress and deterioration of hydronephrosis, and even worsening of renal function. In patients who suffered from bladder irritation symptoms caused by a contracted bladder, augmentation ileocystoplasty could be performed with a continuous ileal segment at the same time.
Nipple nesting sutures are necessary for anti-reflux of the distal anastomosis, while bilateral ureteral proximal anastomosis may not be suitable for an anti-reflux design. To date, it remains undetermined whether an anti-reflux technique is necessary. Some authors considered that anti-reflux implantation was necessary for preventing ileal graft dilation, recurrent urinary tract infection, or metabolic acidosis by stopping the transmission of pressure to the kidney and reducing the duration of contact of urine with the intestinal mucosa (12,20,28). However, others reported that there was no difference in outcome because the natural isoperistaltic waves of ileal grafts kept reflux from reaching the kidney, and an ileal segment longer than 15 cm had been regarded as a defender against the harmful effects on reflux (29,30). Morozov et al. had even claimed that anti-reflux anastomoses might suggest a high rate of strictures (31). In this series, we implemented a distal nipple valve for the anti-reflux procedure in all patients. The anti-reflux nipple was planted into the bladder, which increases the difficulty of urine reflux along the ileal cystostomy. The contraction of the bladder detrusor muscle and the double contractility of the intestine were more conducive to closing the end lumen. Additionally, the ends of the ureters were trimmed into a fish-mouth shape with a diameter comparable to that of the intestine. The proximal anastomosis was made as wide as possible so that urine can flow without resistance.
Strict management during the perioperative period and regular postoperative follow-up of bilateral ileal ureter play an equally irreplaceable role. Only 2 patients suffered from major complications. The sigmoid colon was damaged due to severe intra-abdominal adhesions during the operation in one patient. Although the segment was repaired during the procedure, an intestinal fistula still appeared after the operation, and repair of the fistula was ultimately performed. At present, abdominal imaging shows that the intestinal fistula was cured. This case suggests that it is better to perform bowel preparation when the adhesions caused by radiotherapy are expected to be severe. Once unexpected bowel injury occurs, a primary suture can proceed safely. A simultaneous temporal ileostomy is one secure choice of option for treatment. The other patient suffered from pulmonary embolism. It may be attributed to the hypercoagulable state of cancer patients and the long time in bed. Therefore, ERAS and postoperative prophylactic anticoagulation are also essential. Minor complications were common with urinary tract infection and intestinal obstruction, which were cured by conservative treatment. In addition, blood gas analysis was regularly reviewed and oral sodium bicarbonate tablets were used to prevent postoperative metabolic acidosis.
Postoperative cine MRU is recommended to help identify the function of the wide bowel used for ileal ureteral substitution. In the previous study, cine MR was reported as a reliable tool for assessing gastric motility and monitoring small bowel peristalsis (32). Dilation of the upper urinary tract or the ileal graft does not mean that the operation has failed because the upper urinary tract with long-term hydronephrosis needs a long time to recover. For bilateral ileal ureter, dynamics image can visualize the movement of the ileal segment and urine excretion, showing advantages in providing high temporal and spatial morphology and monitoring the function of the reconstructed urinary tract to current still imaging examination. At the same time, cine MRU is a nonradioactive examination. In our series, there were no obvious abnormalities in the urine drainage and the peristaltic waves of the replaced ureter-ileal graft. No fixed stenosis was detected. In addition, dynamic MRU was superior for recognizing ureteral jets, which indicated the process of urine being transmitted from the ureter into the bladder.
To our knowledge, this is the largest study in China to date to report surgical experience and promising clinical results of bilateral ileal ureter substitution for extremely complicated ureteral strictures induced by radiotherapy. However, there are still some limitations in our study. First, a fundamental limitation was that all patient data were collected retrospectively. Second, information about initial radiotherapy was incomplete because these complicated cases were all referred by other hospitals, and some relevant information could not be traced back. Third, the number of patients was small because of the low incidence of bilateral ureteral strictures. At last, the follow-up time was short, and long-term follow-up results are needed. In the future, prospective cohorts with a large sample size are urgently needed.
In conclusion, for patients receiving pelvic radiotherapy, a regular reexamination is recommended to detect ureteral stricture as early as possible. Bilateral ileal ureter substitution is a feasible option for patients with bilateral ureteral strictures induced by radiotherapy. Rigorous patient selection, reconstructive principal, surgical technique, and strict postoperative management were the precondition of satisfying outcomes and low complication rates.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tau-21-255
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tau-21-255
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-21-255). XL serves as an unpaid editorial board member of Translational Andrology and Urology. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Ethics Committee of Peking University First Hospital approved the study protocol (No. 2020-SR-283), and this study has conformed to the provisions of the Declaration of Helsinki (as revised in 2013). Informed consent was obtained from all participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Delaney G, Jacob S, Barton M. Estimation of an optimal radiotherapy utilization rate for gynecologic carcinoma. Cancer 2004;101:682-92. [Crossref] [PubMed]
- Levenback C, Eifel PJ, Burke TW, et al. Hemorrhagic cystitis following radiotherapy for stage Ib cancer of the cervix. Gynecol Oncol 1994;55:206-10. [Crossref] [PubMed]
- Li F, Guo H, Qiu H, et al. Urological complications after radical hysterectomy with postoperative radiotherapy and radiotherapy alone for cervical cancer. Medicine (Baltimore) 2018;97:e0173 [Crossref] [PubMed]
- Wit EM, Horenblas S. Urological complications after treatment of cervical cancer. Nat Rev Urol 2014;11:110-7. [Crossref] [PubMed]
- Jeong IG, Han KS, Joung JY, et al. The outcome with ureteric stents for managing non-urological malignant ureteric obstruction. BJU Int 2007;100:1288-91. [Crossref] [PubMed]
- Song SH, Pak S, Jeong IG, et al. Outcomes of stent-change therapy for bilateral malignancy-related ureteral obstruction. Int Urol Nephrol 2015;47:19-24. [Crossref] [PubMed]
- Jeong IG, Han KS, Park SH, et al. Ileal augmentation cystoplasty combined with ileal ureter replacement after radical treatment for cervical cancer. Ann Surg Oncol 2016;23:1646-52. [Crossref] [PubMed]
- Knight RB, Hudak SJ, Morey AF. Strategies for open reconstruction of upper ureteral strictures. Urol Clin North Am 2013;40:351-61. [Crossref] [PubMed]
- Gomez-Gomez E, Malde S, Spilotros M, et al. A tertiary experience of ileal-ureter substitution: Contemporary indications and outcomes. Scand J Urol 2016;50:192-9. [Crossref] [PubMed]
- Kim A, Nam W, Song SH, et al. Use of the ileum for ureteral stricture and obstruction in bilateral, unilateral, and single-kidney cases. Urology 2018;111:203-7. [Crossref] [PubMed]
- Armatys SA, Mellon MJ, Beck SD, et al. Use of ileum as ureteral replacement in urological reconstruction. J Urol 2009;181:177-81. [Crossref] [PubMed]
- Kocot A, Kalogirou C, Vergho D, et al. Long-term results of ileal ureteric replacement: a 25-year single-centre experience. BJU Int 2017;120:273-9. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Landoni F, Maneo A, Colombo A, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 1997;350:535-40. [Crossref] [PubMed]
- Rogers L, Siu SS, Luesley D, et al. Radiotherapy and chemoradiation after surgery for early cervical cancer. Cochrane. Database. Syst Rev 2012;5:CD007583 [Crossref] [PubMed]
- Blake P, Swart AM, Orton J, et al. Adjuvant external beam radiotherapy in the treatment of endometrial cancer (MRC ASTEC and NCIC CTG EN.5 randomised trials): pooled trial results, systematic review, and meta-analysis. Lancet 2009;373:137-46. [Crossref] [PubMed]
- Shoemaker GE. Removal of the Ureter with a Tuberculous Kidney. Ann Surg 1911;53:696-8. [Crossref] [PubMed]
- Goodwin WE, Winter CC, Turner RD. Replacement of the ureter by small intestine: clinical application and results of the ileal ureter. J Urol 1959;81:406-18. [Crossref] [PubMed]
- Chung BI, Hamawy KJ, Zinman LN, et al. The use of bowel for ureteral replacement for complex ureteral reconstruction: long-term results. J Urol 2006;175:179-83. [Crossref] [PubMed]
- Verduyckt FJ, Heesakkers JP, Debruyne FM. Long-term results of ileum interposition for ureteral obstruction. Eur Urol 2002;42:181-7. [Crossref] [PubMed]
- Wolff B, Chartier-Kastler E, Mozer P, et al. Long-term functional outcomes after ileal ureter substitution: a single-center experience. Urology 2011;78:692-5. [Crossref] [PubMed]
- Abhyankar N, Vendryes C, Deane LA. Totally intracorporeal robot-assisted laparoscopic reverse seven ileal ureteric reconstruction. Can J Urol 2015;22:7748-51. [PubMed]
- Crassweller PO. Bilateral primary carcinoma of the ureter with use of ileal graft for ureteral replacement: case report. Br J Urol 1958;30:152-60. [Crossref] [PubMed]
- Matlaga BR, Shah OD, Hart LJ, et al. Ileal ureter substitution: a contemporary series. Urology 2003;62:998-1001. [Crossref] [PubMed]
- Boxer RJ, Fritzsche P, Skinner DG, et al. Replacement of the ureter by small intestine: clinical application and results of the ileal ureter in 89 patients. J Urol 1979;121:728-31. [Crossref] [PubMed]
- Lobo N, Kulkarni M, Hughes S, et al. Urologic complications following pelvic radiotherapy. Urology 2018;122:1-9. [Crossref] [PubMed]
- Kochueva M, Dudenkova V, Kuznetsov S, et al. Quantitative assessment of radiation-induced changes of bladder and rectum collagen structure using optical methods. J Biomed Opt 2018;23:1-8. [Crossref] [PubMed]
- Hong P, Cai Y, Li Z, et al. Modified laparoscopic partial ureterectomy for adult ureteral fibroepithelial polyp: technique and initial experience. Urol Int 2019;102:13-9. [Crossref] [PubMed]
- Ali-el-Dein B, Ghoneim MA. Bridging long ureteral defects using the Yang-Monti principle. J Urol 2003;169:1074-7. [Crossref] [PubMed]
- Waldner M, Hertle L, Roth S. Ileal ureteral substitution in reconstructive urological surgery: is an antireflux procedure necessary? J Urol 1999;162:323-6. [Crossref] [PubMed]
- Morozov AV, Pavlenko KA. A direct uretero-enteroanastomosis: a return to the past? Urologiia 2004;4:23-7. [PubMed]
- Froehlich JM, Patak MA, von Weymarn C, et al. Small bowel motility assessment with magnetic resonance imaging. J Magn Reson Imaging 2005;21:370-5. [Crossref] [PubMed]



