
Oligometastatic prostate cancer: definition and the role of local and systemic therapy: a narrative review
Introduction
Hellman and Weichselbaum first came up with the hypothesis of an oligometastatic status as a subgroup of patients with a limited number of detectable metastases and still being a potentially curable disease (1,2). Moreover, genomic data from other tumors suggests biological differences between limited metastatic lesions and widely spread cancers (3). Current treatment options also rely on the assumption that the primary tumor can activate distinct progenitor cells to prepare the metastatic niche and that intraprostatic tumor cells can send metastatic clones at different time intervals (4-6). However, the biology of the oligometastatic stage is still yet not well understood.
Although the term ‚oligometastatic prostate cancer’ (OMPC) is widely used, there is no consensus on its definition (7). In recent studies OMPC was defined by specific numbers of metastases and involved sites while the onset of metastasis (de novo versus vs. recurrent) or previous systemic therapy (hormone-sensitive vs. castration-resistant) are still matter of debate (8,9). Also, detection of metastases varies across different imaging modalities, while bone scan and computed tomography of the abdomen represent the most common staging methods.
Treatment options of OMPC increased significantly in the past decade, as hormonal therapy combined with androgen receptor-targeted agents or chemotherapy became the new standard (10). Moreover, local treatment of the primary and of distinct metastases are promising approaches for a multimodal therapy (11,12).
The goal of this review is to summarize the data of the current literature and to assess which treatment represents the current standard of care and what recent changes should be administered. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/tau-20-1033).
Oligometastatic prostate cancer: definition
There are several studies explicitly defining OMPC while all use the number of metastases for definition, ranging from three to five metastatic lesions while some of them don’t take metastatic site into account (13-18). These studies mostly used 18F-fluorodeoxyglucose (FDG) or 11C-choline PET with co-registered CT. Gandaglia et al. found that the metastatic site plays an important role on survival in patients with metastatic PCA, which should be considered for the definition of OMPC (19).
Because of the lately in detail investigated effect of different treatment options on patients differentiated by their tumor burden (low and high risk/volume) two widely used definitions rely on the LATITUDE (20) and CHAARTED (21) criteria. According to LATITUDE the presence of at least two or more of the following criteria define a high-risk tumor: three or more bone metastases, visceral metastases and ISUP grade 4 or higher (20). The CHAARTED trial defined the presence of four or more bone metastases including at least one outside the axial skeleton (vertebral column or spine) or visceral metastases as patients with high volume disease (21). These two definitions are also used in the guidelines on prostate cancer of the European Association of Urology (10). In this review the definition of OMPC is leaned on the mentioned low-risk and low volume criteria in the hormone-sensitive situation (either de novo or recurrent disease).
Moreover, the influence of improved detection rates for metastases through newer imaging techniques such as 68Ga-PSMA-, 18F-PSMA- and 18-F-flucliclovine – PET/CT on the definition of OMPC remains unclear. Based on these modalities OMPC might be defined differently in the future, e.g., as not only the number of lesions but also the lesion size or the standardized uptake value (SUV) could be taken into account.
ADT-based combination: a new standard
Androgen deprivation therapy (ADT) represented the standard of care for hormone-sensitive metastatic prostate cancer (mHSPC) for about 50 years (10). In the past decade several studies showed a significant improvement of survival for ADT-based combination therapies, e.g., with docetaxel or new androgen receptor-targeted agents (ARTA).
The randomized phase 3 trials CHAARTED (22), GETUG-AFU 15 (23) and STAMPEDE (24) investigated the effect of adding docetaxel to ADT. The effect was shown to be most evident in men with de novo metastatic high volume disease in the first two trials, while a post-hoc analysis of the STAMPEDE collaborators revealed an equivalent benefit no matter the metastatic burden. A recent systematic review and meta-analysis on the benefit of docetaxel including CHAARTED, STAMPEDE arm C and the GETUG trial showed an improved survival with an HR of 0.77 and an absolute improvement in 4-year survival of 9% (21,23,25,26). Also the other clinical endpoints progression free survival [HR 0.62 (CHAARTED)] and time to castration resistance [HR 0.61 (CHAARTED)] were significantly improved by adding docetaxel (21).
The LATITUDE trial (27) and arm G of STAMPEDE (28) investigated the effect of adding abiraterone acetate to ADT in mHSPC. LATITUDE only included high-risk mHSPC, while STAMPEDE also investigated patients with low volume disease, high risk localized disease and patients with nodal recurrence after radical prostatectomy. Both trials observed significant improvement in OS with a HR of 0.62 [LATITUDE (27)] and 0.61 [STAMPEDE, metastatic subgroup (28)]. A post-hoc analysis from STAMPEDE showed significant improvement of OS and failure free survival (FFS) for patients with low-risk mHSPC receiving ADT + abiraterone compared with ADT alone with hazard ratios (HR) for OS and FFS of 0.66 and 0.24, respectively (29). They also showed an improvement in survival of 6% (83% vs. 77%) at three years compared with ADT alone in low-volume disease according to the CHAARTED-criteria (HR 0.64) (21,29). Similar to the results on docetaxel all secondary objectives (PFS, time to radiographic progression, time to pain, time to chemotherapy) favoured the combination with abiraterone.
New androgen receptor (AR) antagonists were evaluated in three large RCTs: ENZAMET (30), ARCHES (31)and TITAN (32). Enzalutamide and apalutamide significantly improved OS and radiographic PFS while all trials had sufficient numbers of low volume disease. Moreover, patients with prior local treatment and recurrent disease represented 25%, 40% and 16% in ARCHES, ENZAMET and TITAN. The 3-year survival rate increased by 8% (80% vs. 72%) for the enzalutamide arm (HR for OS 0.67) and by 10% for the 2-year survival rate for the apalutamide group (HR for OS 0.67) compared to the standard of care (30,32). By choosing radiographic progression free survival as the primary endpoint in ARCHES (31) the median follow-up was shorter compared to ENZAMET (30) (19 vs. 34 months),which should be considered when comparing both trials. A relevant difference of TITAN to the other RCTs was, that patient inclusion criteria consisted consisted of at least one metastatic lesion on bone scan with no regard to visceral or nodal spread. Table 1 summarizes the findings of the mentioned RCTs.
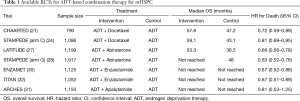
Full table
It is of important note that all aforementioned trials mainly included patients with de novo metastatic disease. Derived from these results ADT-based combination therapy with docetaxel, abiraterone or new AR antagonists was defined as the new standard for patients with mHSPC and should be offered to all patients presenting with both, de novo or recurrent OMPC, although current data is most evident for de novo mHSPC (10).
Which ADT-based combination is the best?
There remains a dilemma which regimen should be preferred for patients presenting with OMPC in the hormone-sensitive situation while, to date, published data indicates almost similar efficacy for all substances and a prospective head-to-head comparison of any of the recommended treatment options is still missing. Hence, the decision relies on the duration of treatment, adverse effects and the patients’ comorbidities. Docetaxel is usually administered every 3 weeks for 6 (up to 10) cycles, whereas abiraterone (plus prednisone), enzalutamide and apalutamide are recommended daily until disease progression or necessarity of change of antineoplastic therapy with a median time on treatment of approximately 33 (abiraterone) and 30 months (enzalutamide) (21,31,33). The median time of PFS for apalutamide was still not reached, but in our opinion will be most likely in the same range of 2.5 years as efficacy results were quite similar to abiraterone and enzalutamide (32).
Adverse events in combination with patients’ comorbidities and consecutive contraindications might play the most important role in the decision-making process. Docetaxel was found to be associated with a higher incidence of acute Common Toxicity Criteria of Adverse Events (CTCAE) grade 3/4 (29.6% in CHAARTED and 52% in STAMPEDE) as well as abiraterone (63% in LATITUDE and 47% in STAMPEDE) compared to the ADT alone group (47% in LATITUDE and 33% in STAMPEDE) (21,26-28). To name as an example febrile neutropenia occurred in 15% of the patients in STAMPEDE (26). In contrast, apalutamide showed almost equivalent rates of CTCAE grade 3/4 events (42.2% in TITAN) compared to the control group (40.8% in TITAN) (32). Enzalutamide had indistinct results for adverse events in ARCHES and ENZAMET, as CTCAE grade 3/4 events were recorded for 24.3% in ARCHES (control group 25.6%) and 57% in ENZAMET (control group 43%). This fact could be explained by the differing study design as in ENZAMET 45% of patients in the interventional group were treated with docetaxel simultaneously, whereas ARCHES used enzalutamide only in the interventional arm (30,31). Hence, the combination of docetaxel and enzalutamide does not represent a therapeutic standard, as combined toxicity might limit the treatment.
Nevertheless, across the available agents the toxicity profile is quite different. Abiraterone plus prednisone mainly causes hypertension, hypokalemia, cardiovascular disorders and elevated liver enzymes, whereas enzalutamide is known for side effects related to the central nervous system (incl. seizures), vascular disorders (incl. myocardial ischemia) and fractures (partly due to an increased rate of falls) (34). The TITAN trial detected dermal rash, fracture and hypothyroidism as most relevant adverse effects of apalutamide (32). In contrast, docetaxel can cause fatigue, bone marrow suppression and neurotoxicity. The aforementioned trials all reported quality of life (QOL) data separately with different assessments such as the Functional Assessment of Cancer Therapy – Prostate (FACT-P), FACT-taxane, Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F) or the Brief Pain Inventory – Short Form (BPI-SF) scores during the trial. FACT-P for enzalutamide and apalutamide remained almost stable and similar to the control group over time (31,32). A meta-analysis of abiraterone vs. docetaxel favoured abiraterone in terms of QOL outcomes and radiographic PFS (35).
In summary, as comparative data is still missing, the decision of which option should be chosen remains an individual decision regarding patients preferences and comorbodities. Based on the available data to date, abiraterone should be chosen over docetaxel, if patients are feasible. As apalutamide seems to have less severe adverse events, it represents a good alternative for multimorbide patients.
There are several ongoing phase 3 trials addressing the mHSPC setting, of which results are expected in the next 5 years {SWOG-1216 [NCT01809691], PEACE-1 [NCT01957436], STAMPEDE arm J [NCT00268476], ARASENS [NCT02799602]}. These will possably establish new standards in the treatment of OMPC, although, to our knowledge, currently no ongoing RCT investigates the efficacy of the available agents in a head-to-head comparative design.
Therapy of the primary tumor
We know from other tumor entities, such as metastatic breast cancer, ovarian cancer or renal cell carcinoma, that overall survival (OS) of selected patients improves from cytoreductive surgery (36-38). Early preclinical investigations in animal models revealed a similar survival benefit for surgical extraction or radiotherapy of the primary tumor with reduced angiogenesis in distant lesions, arising to a hypothesis of an abscopal effect (effect away from target) of local therapy (39,40). This hypothesis was later underlined by several studies, which found that the primary tumor can also influence the development of a ‚premetastatic niches‘ (4,41-43). The primary tumor might induce the preparation of these for metastases receptive microenvironments by recruiting bone marrow-derived cells via cytokine secretion (4,41-43).
Several retrospective studies first revealed a comparable effect in patients with metastatic prostate cancer. Rusthoven et al. evaluated the National Cancer Database in the USA with a systematic a priori defined statistical analysis. They showed in univariate and multivariate analysis an improved OS (53 vs. 29 months) for patients treated with radiotherapy (RT) additionally to ADT versus patients with ADT alone. Moreover, a propensitiy score analysis including 537 patients redemonstrated similar results for the RT group (44). Interestingly patients with very high risk cancer (Gleason score 9-10 or T4-stage) had significantly worse benefit of local treatment of the primary (P=0.009) (44).
A retrospective study of the Surveillance Epidemiology and End Results database (SEER) showed equivalent results with improvement of survival and cancer specific mortality for patients with local treatment, either RP or brachytherapy with a favorizing tendency for the surgical approach. 5-year OS was significantly higher in patients undergoing RP (67.4%) or brachytherapy (52.6%) versus no local therapy (22.5%) (45).
Retrospectively analyzed data from the Munich cancer registry (46), the Swedish prostate cancer database (47) and the National Cancer Database (48) indicated similar results for de novo mHSPC.
Two recently published RCTs addressed the RT of the primary tumor in de novo mHSPC and reshaped the treatment guidelines. Table 2 illustrates the results of both trials.
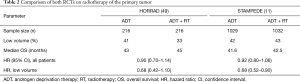
Full table
The HORRAD trial included 432 patients with primary bone metastases randomized into ADT alone or ADT + RT to the primary tumor of the prostate (50). In this trial there was no significant benefit for the RT arm in terms of OS, but the majority of the eligible patients had a high metastatic burden: 63% had >5 bone metastases and the median PSA prior to randomization was 145 ng/mL. Patients with less than 5 bone metastases showed a trend favoring RT (HR 0.68, P>0.05) (50). In the same year data from the multi-arm-multi-stage trial of STAMPEDE (arm H) were published, which randomized 2061 patients with de novo mHSPC into standard of care (including docetaxel by the end of 2015) ± RT (11). The RT arm showed no beneficial effect for the whole study population, whereas a significant advantage was shown for selected patients with low metastatic burden defined as less than four bone metastases in the axial skeleton and no visceral metastases according to the CHAARTED criteria. The patients had a median initial PSA of 97 ng/mL and a median follow-up of 37 months.The 3-year survival rate was improved by 8% from 73% to 81% in the RT—group vs. the control group (HR 0.68, P=0.007) for patients with low burden (11). Nevertheless, only 18% of included patients received one of the current standards of a chemohormonal therapy and RT excluded lymph nodes in the pelvis. This should be taken into account, although RT is strongly recommended for patients with de novo OMPC.
As RT appeared to be of crucial benefit for de novo PCA with low metastatic burden the question arises if surgical treatment can not only improve survival in the same way but also avoid local complications due to local progression of the tumor. Retrospective data on the surgical approach underline this hypothesis (45-47,51,52).
Feasibility and safety was evaluated by Sooriakumaran et al. in an multi-institutional analysis in 106 patients. Although data was collected in a nontrial setting, reported continence rates after RP was 64.4% and total complications at 90 days after surgery were 20.8%, similar to reported data in a large meta-analysis on RP (53,54).
Heidenreich et al. compared ADT vs. ADT + cytoreductive radical prostatectomy (cRP) including23 highly selected patients with good response to neoadjuvant ADT and a low metastatic burden (51). They showed a benefit in median cancer specific survival and PFS of 47 and 38.6 months in the cRP group vs. 40 and 26.5 months in the ADT only group. No major complications were observed, minor complications occurred in 23.7% of patients and 91.3% were continent (51). Another multiinstitutional retrospective trial with 113 OMPC-patients underlined these results and confirmed the preoperative PSA as a strong predictor for biochemical PFS as well as the postoperative PSA-nadir for OS. Best results were found for a preoperative PSA serum concentration less than 1.0 ng/mL (P=0.0004) after neoadjuvant ADT and a PSA-nadir of less than 0.1 ng/mL (P=0.0003) (52). In this study Clavien-Dindo grade IIIa and IIIb complications were reported in only 5.3% without any grade IV or V complications, demonstrating the feasibility and safety (52). Not surprisingly, rates of local complications (e.g., bladder outlet obstruction, ureteric obstruction or pelvic pain) due to local tumor progression were decreased after cRP (20%) compared to RT (46.7%) or ADT alone (54.3%) (55).
Jang et al. demonstrated similar results for patients with OMPC treated with robot-assisted radical prostatectomy (RARP). Seventy-nine men with five or fewer bone metastases and no visceral metastases were retrospectively analyzed of whom 41 received ADT alone and 38 additional cytoreductive RARP. Patients in the interventional group had no urinary tract complications due to disease progression compared to 26.8% in the ADT group. Surgically treated patients showed improved PFS (75 vs. 28 months, P=0.008) and cancer specific survival (median not reached vs. 40 months, P=0.002) compared to the ADT-alone group (56).
To date there are no prospective data on performing surgery in men with OMPC. The prospective g-RAMPP trial was initiated in 2015 but stopped after the results of STAMPEDE were published because of ethically not justifiable withhold of local treatment (NCT02454543). The results of this trial are still pending. Other running trials are studying the benefit of RT and cRP vs. various systemic therapies (ClinicalTrials.gov: NCT01751438, NCT02020070, NCT02138721 and PEACE-1 NCT03678025) and the results are expected in the next years to clearly clarify the role of local therapy. As these are pending we believe that cRP can be offered to highly selected patients at experienced centres after interdisciplinary decision.
An interesting novel approach is investigated in a recently started three-arm controlled trial (NCT03763253), which randomises patients into standard of care (ADT with or without chemohormonal therapy), minimally invasive ablative therapy (SOC with high intensity focused ultrasound) or radical therapy (SOC with cRP or RT). To our knowledge this is the first trial to evaluate the benefit of focal treatment for patients with OMPC. As results are not expected before 2024 currently focal treatment for OMPC should be performed only in an experimental setting.
Metastasis-directed therapy
In addition to local therapy metastasis-directed therapy (MDT) is currently also a matter of debate. Besides the treatment of local symptoms the rationale behind MDT is based on the findings of Gundem et al., who found that not only the primary tumor but also distinct metastases can be the source for new metastases (6).
Quite recently, data from the ORIOLE trial evaluated the effect of MDT in recurrent OMPC after prior definitive treatment of the primary tumor with surgery or radiotherapy (57). Fifty-four men with 3 or less extracranial metastases were randomized in a 2:1 ratio to receive stereotactic ablative radiotherapy (SABR) vs. observation. They demonstrated good local control of the treated metastases as well as improvement in median PFS [not reached vs. 5.8 months (control group), HR 0.30, P=0.002]. Moreover, SABR of all PSMA-PET/CT avid lesions decreased the risk of new lesions at 6 months from 63% to 16% (P=0.006), although this was an observational finding as only visible metastases on conventional imaging were treated (57). These results corroborate the findings of Ost et al. who randomized patients with recurrent OMPC and three or fewer metastases on choline PET/CT and showed an increase of ADT-free survival from 13 to 21 months in the MDT group with a stronger effect in patients with a rapid PSA doubling time of less than 3 months (HR 0.38, P=0.06) (12).
Salvage lymph node dissection (SLND) for nodal recurrent prostate cancer after radical prostatectomy also represents a specific MDT and a therapeutic alternative for OMPC with the advantage of possible postponement of systemic treatment. In the largest series of patients with SLND only 25% of men developed clinical recurrence within one year after SLND. Fossati et al. developed a novel risk stratification tool to predict the benefit of SLND in patients with nodal recurrence, which includes Gleason grade group, time from radical prostatectomy to biochemical recurrence, number and site involvement of nodal metastases, hormonal therapy at the time of imaging and PSA level at SLND (58). Porres et al. demonstrated, that the majority of patients (62.2%) remained without ADT at a median follow-up of 21 months, leading to a possible benefit of postponing hormonal therapy with less adverse effects and possibly postponed castration-resistant status for well selected patients (59).
Likewise there are several ongoing studies on MDT of which results are expected in the next few years and hopefully will adress the requirement of MDT in de novo mHSPC. Until then MDT should not be offered to patients with OMPC as a standard except from experimental settings.
Conclusion
The past decade led to many new treatment options for patients with de novo or recurrent hormone-sensitive oligometastatic prostate cancer. At the current state treatment intensification consisting of an ADT-based combination is recommended for all patients presenting with OMPC. As our understanding of the oligometastatic status is growing, the importance of local therapy to the primary tumor is significantly increasing, although data from ongoing trials need to confirm novel treatment columns. Promising results were found for metastasis-directed therapy, albeit evidence is still lacking and therefore it should only be used in an experimental setting.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Badrinath R. Konety, Daniel W. Lin) for the series “Current and Future Topics on Prostate Cancer” published in Translational Andrology and Urology. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/tau-20-1033
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-20-1033). The series “Current and Future Topics on Prostate Cancer” was commissioned by the editorial office without any funding or sponsorship. Both authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDeri
References
- Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol 1995;13:8-10. [Crossref] [PubMed]
- Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol 2011;8:378-82. [Crossref] [PubMed]
- Wuttig D, Baier B, Fuessel S, et al. Gene signatures of pulmonary metastases of renal cell carcinoma reflect the disease-free interval and the number of metastases per patient. Int J Cancer 2009;125:474-82. [Crossref] [PubMed]
- Kaplan RN, Riba RD, Zacharoulis S, et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 2005;438:820-7. [Crossref] [PubMed]
- Kaplan RN, Rafii S, Lyden D. Preparing the “soil”: The premetastatic niche. Cancer Res 2006;66:11089-93. [Crossref] [PubMed]
- Gundem G, Van Loo P, Kremeyer B, et al. The evolutionary history of lethal metastatic prostate cancer. Nature 2015;520:353-7. [Crossref] [PubMed]
- Tosoian JJ, Gorin MA, Ross AE, et al. Oligometastatic prostate cancer: Definitions, clinical outcomes, and treatment considerations. Nat Rev Urol 2017;14:15-25. [Crossref] [PubMed]
- Foster CC, Weichselbaum RR, Pitroda SP. Oligometastatic prostate cancer: Reality or figment of imagination? Cancer 2019;125:340-52. [Crossref] [PubMed]
- Slaoui A, Albisinni S, Aoun F, et al. A systematic review of contemporary management of oligometastatic prostate cancer: fighting a challenge or tilting at windmills? World J Urol 2019;37:2343-53. [Crossref] [PubMed]
- Cornford P, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part II: Treatment of Relapsing, Metastatic, and Castration-Resistant Prostate Cancer. Eur Urol 2017;71:630-42. [Crossref] [PubMed]
- Parker CC, James ND, Brawley CD, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet 2018;392:2353-66. [Crossref] [PubMed]
- Ost P, Reynders D, Decaestecker K, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: A prospective, randomized, multicenter phase II trial. J Clin Oncol 2018;36:446-53. [Crossref] [PubMed]
- Tabata KI, Niibe Y, Satoh T, et al. Radiotherapy for oligometastases and oligo-recurrence of bone in prostate cancer. Pulm Med 2012;2012:541656 [Crossref] [PubMed]
- Ahmed KA, Barney BM, Davis BJ, et al. Stereotactic body radiation therapy in the treatment of oligometastatic prostate cancer. Front Oncol 2013;2:215. [Crossref] [PubMed]
- Berkovic P, De Meerleer G, Delrue L, et al. Salvage stereotactic body radiotherapy for patients with limited prostate cancer metastases: Deferring androgen deprivation therapy. Clin Genitourin Cancer 2013;11:27-32. [Crossref] [PubMed]
- Schick U, Jorcano S, Nouet P, et al. Androgen deprivation and high-dose radiotherapy for oligometastatic prostate cancer patients with less than five regional and/or distant metastases. Acta Oncol 2013;52:1622-8. [Crossref] [PubMed]
- Decaestecker K, De Meerleer G, Lambert B, et al. Repeated stereotactic body radiotherapy for oligometastatic prostate cancer recurrence. Radiat Oncol 2014;9:135. [Crossref] [PubMed]
- Ost P, Jereczek-Fossa BA, As N, Van , et al. Progression-free Survival Following Stereotactic Body Radiotherapy for Oligometastatic Prostate Cancer Treatment-naive Recurrence: A Multi-institutional Analysis. Eur Urol 2016;69:9-12. [Crossref] [PubMed]
- Gandaglia G, Karakiewicz PI, Briganti A, et al. Impact of the Site of Metastases on Survival in Patients with Metastatic Prostate Cancer. Eur Urol 2015;68:325-34. [Crossref] [PubMed]
- Fizazi K, Tran NP, Fein L, et al. Abiraterone acetate plus prednisone in patients with newly diagnosed high-risk metastatic castration-sensitive prostate cancer (LATITUDE): final overall survival analysis of a randomised, double-blind, phase 3 trial. Lancet Oncol 2019;20:686-700. [Crossref] [PubMed]
- Kyriakopoulos CE, Chen YH, Carducci MA, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer: long-term survival analysis of the randomized phase III E3805 chaarted trial. J Clin Oncol 2018;36:1080-7. [Crossref] [PubMed]
- Sweeney CJ, Chen Y-H, Carducci M, et al. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med 2015;373:737-46. [Crossref] [PubMed]
- Gravis G, Fizazi K, Joly F, et al. Androgen-deprivation therapy alone or with docetaxel in non-castrate metastatic prostate cancer (GETUG-AFU 15): A randomised, Open-label, Phase 3 trial. Lancet Oncol 2013;14:149-58. [Crossref] [PubMed]
- Clarke NW, Ali A, Ingleby FC, et al. Addition of docetaxel to hormonal therapy in low- And high-burden metastatic hormone sensitive prostate cancer: Long-term survival results from the STAMPEDE trial. Ann Oncol 2019;30:1992-2003. [Crossref] [PubMed]
- Sathianathen NJ, Philippou YA, Kuntz GM, et al. Taxane-based chemohormonal therapy for metastatic hormone-sensitive prostate cancer. Cochrane Database Syst Rev 2018;10:CD012816 [Crossref] [PubMed]
- James ND, Sydes MR, Clarke NW, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): Survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 2016;387:1163-77. [Crossref] [PubMed]
- Fizazi K, Tran N, Fein L, et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N Engl J Med 2017;377:352-60. [Crossref] [PubMed]
- James ND, de Bono JS, Spears MR, et al. Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy. N Engl J Med 2017;377:338-51. [Crossref] [PubMed]
- Hoyle AP, Ali A, James ND, et al. Abiraterone in “High-” and “Low-risk” Metastatic Hormone-sensitive Prostate Cancer(Figure presented.). Eur Urol 2019;76:719-28. [Crossref] [PubMed]
- Davis ID, Martin AJ, Stockler MR, et al. Enzalutamide with Standard First-Line Therapy in Metastatic Prostate Cancer. N Engl J Med 2019;381:121-31. [Crossref] [PubMed]
- Armstrong AJ, Szmulewitz RZ, Petrylak DP, et al. Arches: A randomized, phase III study of androgen deprivation therapy with enzalutamide or placebo in men with metastatic hormone-sensitive prostate cancer. J Clin Oncol 2019;37:2974-86. [Crossref] [PubMed]
- Taneja SS. Re: Apalutamide for metastatic, castration-sensitive prostate cancer. J Urol 2019;202:661. [Crossref] [PubMed]
- Chi KN, Protheroe A, Rodríguez-Antolín A, et al. Patient-reported outcomes following abiraterone acetate plus prednisone added to androgen deprivation therapy in patients with newly diagnosed metastatic castration-naive prostate cancer (LATITUDE): an international, randomised phase 3 trial. Lancet Oncol 2018;19:194-206. [Crossref] [PubMed]
- Tonyali S, Haberal HB, Sogutdelen E. Toxicity, Adverse Events, and Quality of Life Associated with the Treatment of Metastatic Castration-Resistant Prostate Cancer. Curr Urol 2017;10:169-73. [Crossref] [PubMed]
- Feyerabend S, Saad F, Li T, et al. Survival benefit, disease progression and quality-of-life outcomes of abiraterone acetate plus prednisone versus docetaxel in metastatic hormone-sensitive prostate cancer: A network meta-analysis. Eur J Cancer 2018;103:78-87. [Crossref] [PubMed]
- Motzer RJ, Russo P. Cytoreductive Nephrectomy — Patient Selection Is Key. N Engl J Med 2018;379:481-2. [Crossref] [PubMed]
- Headon H, Wazir U, Kasem A, et al. Surgical treatment of the primary tumour improves the overall survival in patients with metastatic breast cancer: A systematic review and meta-analysis. Mol Clin Oncol 2016;4:863-7. [Crossref] [PubMed]
- Brand AH, DiSilvestro PA, Sehouli J, et al. Cytoreductive surgery for ovarian cancer: Quality assessment. Ann Oncol 2017;28:viii25-viii29.
- Kadmon D, Heston WDW, Fair WR. Treatment of a metastatic prostate derived tumor with surgery and chemotherapy. J Urol 1982;127:1238-42. [Crossref] [PubMed]
- Hartford AC, Gohongi T, Fukumura D, et al. Irradiation of a primary tumor, unlike surgical removal, enhances angiogenesis suppression at a distal site: Potential role of host-tumor interaction. Cancer Res 2000;60:2128-31. [PubMed]
- Psaila B, Lyden D. The metastatic niche: Adapting the foreign soil. Nat. Rev. Cancer 2009;9:285-93. [Crossref] [PubMed]
- Erler JT, Bennewith KL, Cox TR, et al. Hypoxia-Induced Lysyl Oxidase Is a Critical Mediator of Bone Marrow Cell Recruitment to Form the Premetastatic Niche. Cancer Cell 2009;15:35-44. [Crossref] [PubMed]
- Hiratsuka S, Watanabe A, Aburatani H, et al. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat Cell Biol 2006;8:1369-75. [Crossref] [PubMed]
- Rusthoven CG, Jones BL, Flaig TW, et al. Improved survival with prostate radiation in addition to androgen deprivation therapy for men with newly diagnosed metastatic prostate cancer. J Clin Oncol 2016;34:2835-42. [Crossref] [PubMed]
- Culp SH, Schellhammer PF, Williams MB. Might men diagnosed with metastatic prostate cancer benefit from definitive treatment of the primary tumor? A SEER-based study. Eur Urol 2014;65:1058-66. [Crossref] [PubMed]
- Gratzke C, Engel J, Stief CG. Role of radical prostatectomy in metastatic prostate cancer: Data from the munich cancer registry. Eur Urol 2014;66:602-3. [Crossref] [PubMed]
- Sooriakumaran P, Nyberg T, Akre O, et al. Survival Among Men at High Risk of Disseminated Prostate Cancer Receiving Initial Locally Directed Radical Treatment or Initial Androgen Deprivation Therapy. Eur Urol 2017;72:345-51. [Crossref] [PubMed]
- Löppenberg B, Dalela D, Karabon P, et al. The Impact of Local Treatment on Overall Survival in Patients with Metastatic Prostate Cancer on Diagnosis: A National Cancer Data Base Analysis. Eur Urol 2017;72:14-9. [Crossref] [PubMed]
- Burdett S, Boevé LM, Ingleby FC, et al. Prostate Radiotherapy for Metastatic Hormone-sensitive Prostate Cancer: A STOPCAP Systematic Review and Meta-analysis. Eur Urol 2019;76:115-24. [Crossref] [PubMed]
- Boevé LMS, Hulshof MCCM, Vis AN, et al. Effect on Survival of Androgen Deprivation Therapy Alone Compared to Androgen Deprivation Therapy Combined with Concurrent Radiation Therapy to the Prostate in Patients with Primary Bone Metastatic Prostate Cancer in a Prospective Randomised Clinical Tria. Eur Urol 2019;75:410-8. [Crossref] [PubMed]
- Heidenreich A, Pfister D, Porres D. Cytoreductive radical prostatectomy in patients with prostate cancer and low volume skeletal metastases: Results of a feasibility and case-control study. J Urol 2015;193:832-8. [Crossref] [PubMed]
- Heidenreich A, Fossati N, Pfister D, et al. Cytoreductive Radical Prostatectomy in Men with Prostate Cancer and Skeletal Metastases. Eur Urol Oncol 2018;1:46-53. [Crossref] [PubMed]
- Sooriakumaran P, Karnes J, Stief C, et al. A Multi-institutional Analysis of Perioperative Outcomes in 106 Men Who Underwent Radical Prostatectomy for Distant Metastatic Prostate Cancer at Presentation. Eur Urol 2016;69:788-94. [Crossref] [PubMed]
- Tewari A, Sooriakumaran P, Bloch DA, et al. Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: A systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol 2012;62:1-15. [Crossref] [PubMed]
- Won ACM, Gurney H, Marx G, et al. Primary treatment of the prostate improves local palliation in men who ultimately develop castrate-resistant prostate cancer. BJU Int 2013;112:E250 [Crossref] [PubMed]
- Jang WS, Kim MS, Jeong WS, et al. Does robot-assisted radical prostatectomy benefit patients with prostate cancer and bone oligometastases? BJU Int 2018;121:225-31. [Crossref] [PubMed]
- Phillips R, Shi WY, Deek M, et al. Outcomes of Observation vs Stereotactic Ablative Radiation for Oligometastatic Prostate Cancer: The ORIOLE Phase 2 Randomized Clinical Trial. JAMA Oncol 2020;6:650-9. [Crossref] [PubMed]
- Fossati N, Suardi N, Gandaglia G, et al. Identifying the Optimal Candidate for Salvage Lymph Node Dissection for Nodal Recurrence of Prostate Cancer: Results from a Large, Multi-institutional Analysis. Eur Urol 2019;75:176-83. [Crossref] [PubMed]
- Porres D, Pfister D, Thissen A, et al. The role of salvage extended lymph node dissection in patients with rising PSA and PET/CT scan detected nodal recurrence of prostate cancer. Prostate Cancer Prostatic Dis 2017;20:85-92. [Crossref] [PubMed]


