
Contemporary outcomes following robotic prostatectomy for locally advanced and metastatic prostate cancer
Introduction
Current guideline-based approaches to the management of prostate cancer are first centered on appropriate risk stratification based upon biopsy, physical exam, and imaging evaluation (1). Subsequent patient assignment to these categories serves as a tool for the clinician in determining an appropriate management strategy. Findings suggestive of non-organ confined prostate cancer, cancers with multiple high risk features, or those with evidence of nodal or metastatic involvement present a challenging clinical dilemma, as these patients are less likely to receive a curative benefit from single modality treatment than with organ confined disease alone. Various predictive models have demonstrated the presence of these characteristics as signifying an increased risk of recurrence and are supported by guideline recommendations to consider the use of adjuvant therapies post-operatively (1-3). Current National Comprehensive Cancer Network (NCCN) guidelines define locally advanced prostate cancers (or very high risk) as those with at least one of the following features; pT3b-T4 disease, primary grade group 5 pathology, or 4 or more positive cores of grade group 4–5 (1). While the majority of new prostate cancer diagnoses represent lower stage disease, data suggests that as many as 10% or more of patients may have locally advanced disease at presentation, with higher incidence if those patients with T3a pathology are also considered (4-7). The paradigm shift instituted by the 2012 United States Preventive Services Task Force regarding routine prostate screening has already demonstrated trends toward decreased biopsy rates, PSA testing incidence, and a decreased proportion of patients managed with definitive local treatment (LT) (8). Unfortunately, data also suggests this has led to an increase in PSA at the time of referral, the incidence of high risk disease, and in some cases metastatic disease (2,8-10).
For those patients with very high risk disease, primary treatment recommendations include the initiation of androgen deprivation therapy (ADT) with either external beam radiation therapy (EBRT) alone or EBRT and brachytherapy (1). In a smaller subset of patients, radical prostatectomy (RP) may also be considered along with bilateral pelvic lymph node dissection (PLND). This treatment is typically reserved for younger and healthier patients who many perceive could have the greatest benefit from resection. Given the aforementioned emerging data suggesting higher incidences of advanced disease, there is a legitimate expectation that more men might be appropriate candidates for surgical resection. Outcomes in these patient groups are less defined due to the heterogeneity of reporting, small sample sizes, and varying definitions of outcome measures. The purpose of this review is to provide an updated review of outcomes measures from several different broad vantage points; survival outcomes, functional considerations, and surgical/technical aspects. The main focus will be on those patients with locally advanced prostate cancers, with additional comments as appropriate on those patients with clinical or biopsy proven nodal disease, or metastatic disease. Comments will also be made regarding ongoing clinical trials.
Survival outcomes
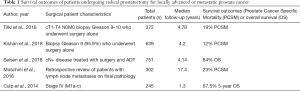
A primary consideration of offering radical surgery to patients with very high risk disease is the potential for durable freedom from recurrence or decreased mortality rates when compared to other options. Tilki et al. provided a comparative analysis between patients receiving MaxRP (defined as RP with adjuvant EBRT, ADT, or both vs. those patients receiving MaxRT (defined as EBRT, brachytherapy, and ADT). In the surgical cohort of 559 patients, 372 (66.5%) were treated with RP alone while the remaining patients received MaxRP or other forms of adjuvant therapy (11). Of patients undergoing RP with or without adjuvant therapy, a total of 409 (73.2%) had pathologic T3b disease or higher, with 296 (52.9%) having N1 pathology. Of the 372 men treated with RP alone, 71 (19%) were dead at a median follow-up of 4.78 years. In regard to prostate cancer specific mortality (PCSM) or all-cause mortality (ACM), patients who underwent RP alone fared worse compared to those undergoing maxRT (HR =2.80; 95% CI, 1.26–6.22, P=0.01 for PCSM and HR =1.65, 95% CI, 0.94–2.91, P=0.08 for ACM) (11). However, this was not noted in patients who received adjuvant therapy, whether through radiation therapy (RT) or maxRP. When maxRP was compared to maxRT, there were no significant survival differences appreciated, suggesting each as potential appropriate treatment strategies. The findings of this study support the likelihood that RP alone may not be a durable treatment strategy in this cohort, but may serve as a reasonable consideration for the initiation of local therapy in select patients with the understanding of the need for additional therapies pending final pathology, PSA kinetics, and other factors.
A 2018 study by Kishan et al. performed a multi-institutional retrospective review evaluating optimal treatment strategies for patients with Gleason 9-10 prostate adenocarcinoma. The study aimed to compare those patients receiving RP, EBRT, or EBRT + BT. The majority of men classified as high risk in the prostatectomy group had a biopsy Gleason score of 9 (613 patients, 95.9%). Of 639 patients treated with RP, 45 (7%) had clinical T3b disease or higher (12). It is important to note that the study identified those patients who underwent surgery were younger than those undergoing radiation therapy, had lower initial PSA levels, and had a significantly higher proportion of cT1-T2 lesions (P<0.01) (12). Looking broadly at survival outcomes in these patients, the adjusted 5-year PCSM rates were 12% (95% CI, 8–17%) for RP, 13% (95% CI, 8–19%) for EBRT, and 3% (95% CI, 1–5%) for EBRT + BT. Adjusted 5-year incidence rates of distant metastasis were 24% (95% CI, 19–30%) for RP, 24% (95% CI, 20–28%) for EBRT, and 8% (95% CI, 5–11%) for EBRT + BT. When looking at competing risk analysis, the 5-year incidence rates of PCSM were 10% (95% CI, 7–12%) for RP, 11% (95% CI, 8–14%) for EBRT, and 3% (95% CI, 1–4%) for EBRT + BT. However, it should also be noted that a proportion of patients treated with surgery were managed with neoadjuvant or adjuvant therapies. 19% of patients received neoadjuvant therapy (typically ADT) while 8.7% received adjuvant radiotherapy and 11.3% received adjuvant systemic therapy (12). 288 patients (45.1%) had pT3b disease or higher while 358 (56%) had other adverse features including positive surgical margins or nodal disease. This study did not specifically delineate outcomes between those surgical patients who were managed with combination therapy vs. those with surgery alone. It would be logical to infer that those with the higher pathological disease or with adverse features would be the most likely candidates, but this is not clear. Given the multi-institutional nature of this study, some patients were managed based upon institution-specific protocols that may not have necessarily followed this line of thinking. Nevertheless, key conclusions that can be drawn from this is the potential for durable benefit of surgery in select patients, while conceding that a proportion will likely require combination therapy, and may still not receive optimal outcomes compared to radiation therapies, particularly EBRT + BT in this study.
There is a larger abundance of studies comparing multimodal approaches that nonetheless provide useful information applicable to single modality strategies. Jang et al. evaluated patients with locally advanced (cT3-T4N0M0) or regionally advanced (cT3T4N1M0) disease using SEER-Medicare data to compare outcomes associated with RP + XRT or XRT + ADT. The primary study endpoints included PCSM and OS according to stage, Gleason score, and treatment received, while also evaluating treatment-related complications (13). A total of 13,856 men were evaluated over this time period, with approximately 20.8% (2,884 patients) undergoing RP alone. Unfortunately, there is limited data beyond a descriptive standpoint in these patients, and they are likely to have come from a less contemporary era of management pre-dating the multimodal approach adoption. Demonstrating consistency with other studies, it was noted that men with more comorbidities, older men, unmarried men, and those diagnosed in more contemporary eras were more likely to receive multimodal therapy via radiation and ADT vs. RP and radiation (13). Higher clinical stage 3 patients were more likely to undergo RP with radiation irrespective of nodal involvement, while those patients with clinical stage 4 disease were more likely to undergo XRT and ADT. From a survival standpoint, patients who received RP with radiation therapy were found to be less likely to die of prostate cancer as well as any other cause in comparison to those treated with radiation and ADT. Ten-year disease specific survival for men undergoing RP plus radiation and men undergoing radiation and ADT favored surgery at all stages; 88.9% vs. 74.2% for T3a/bN0M0 disease, (survival difference, 14.7%; 95% CI, 11.4–17.2%), 75.7% vs. 58.6% for T3a/bN1M0 disease, (survival difference, 17.1%, 95% CI, -0.8–34.2%), and 72% vs. 60.5% for T4N0M0 disease, (survival difference, 11.6%, 95% CI, 0.8–16.9%) (13). Similar findings were noted when considering overall survival as well. However, it was also appreciated that patients undergoing RP with radiation were found to have increased rates of erectile dysfunction and urinary incontinence when compared to the XRT with ADT group. The findings of this study were important in outlining the potential benefits of surgical intervention in these patient cohorts, particularly in those younger and less comorbid patients and pointed out the need for surgical arms in future prospective analyses. While the potential disadvantages of surgery are known, these findings support the theoretical benefits of surgery including tumor volume control, optimal local control and more accurate staging of prostatectomy and nodal specimens to allow for more optimal stratification and selection of adjuvant therapies (13). These findings were also consistent with data outlined by Feldman et al. in a 2017 retrospective review that evaluated 2,935 elderly (>65) patients who underwent RP vs. EBRT for locally advanced prostate cancer. EBRT in this cohort was also associated with a higher overall and PCSM rates when compared to surgery (HR 1.41, 95% CI, 1.09–1.82 and HR 2.35, 95% CI, 1.85–2.98) (14). Additionally, surgery patients were noted to have higher rates of urinary and sexual toxicities than those undergoing EBRT.
A 2020 systematic review further evaluated the current evidence regarding this clinical question. This work by Moris et al. evaluated studies between January 2000 and May 2019 inclusive of high-risk localized or locally advanced prostate cancer in an attempt to comparatively evaluate primary treatment strategies (15). Primary outcomes included distant metastatic disease development, but also included PCSM, biochemical recurrence (BCR) patterns, and the need for salvage treatment. A total of 90 studies were evaluated after appropriate selection criteria were met. A total of eight studies evaluated the use of RP with the use of neoadjuvant or adjuvant therapies, with five studies comparing prostatectomy to EBRT +/- BT (15). The general findings from this analysis support RP playing a potential role in select patients with advanced disease, but stress the importance of the informed decision making process with patients to communicate the possible need for multimodal therapy for a curative goal. The authors also point out that to date, no curative primary treatment modality as part of a multimodal approach has shown superiority in terms of survival (15). A summary table is provided in Table 1.
Full table
Clinical node positive disease
Fewer studies have focused on those patients with evidence of clinically positive nodal disease or metastatic disease at it pertains to surgical intervention. Seisen et al. retrospectively evaluated patients in a population-based study with clinical node positive disease who underwent LT defined as either radiation therapy or RP followed by ADT vs. those patients receiving ADT alone. A total of 2,967 patients were identified, 751 (37.8%) of whom underwent RP. Of note, 304 (40.5%) of these surgical patients also had cT3–T4 disease while 366 (48.7%) had Gleason 8–10 biopsy specimens (16). The main endpoint in this study was death from any cause. At a median follow-up of 49.7 months, LT +/- ADT was associated with an overall mortality-free survival benefit compared to ADT alone (HR =0.31, 95% CI, 0.13–0.74, P=0.007) (16). Looking specifically at those patients undergoing RP, the 5-year OS was 84% (95% CI, 76–93%) vs. 73.2% for radiation (95% CI, 64.6–82.9%). There was no difference noted between the two treatment arms (P=0.7) (16). The authors point out important points for consideration. While they acknowledge that this approach may not be curative in of itself, it may be the first step in a multi-modal approach to provide the best individualized treatment strategies. This is supported by the fact that 20% of the patients in this study were found to be pN0 at the time of RP. This would subsequently potentially limit the need and delivery of ADT to a portion of patients, sparing them from potential toxicities (16).
Evaluating a less contemporary cohort of patients, Moschini et al. identified 50 patients from a total cohort of 302 (17%) who had clinical positive lymph nodes and underwent RP between 1988 and 2003 at the Mayo Clinic. There was a clinically significant higher volume of pathological nodes in the clinically node positive group, and 45 of these (90%) received adjuvant therapy via ADT or radiation. A benefit of this study was a robust follow-up interval of 17.4 years in which 161 total deaths were recorded, 70 from prostate cancer (17). The authors found that the total number of positive lymph nodes (HR =1.10, P=0.02) and pathologic Gleason score 8–10 (HR =2.37, P=0.04) were significant predictors of cancer specific mortality, but clinically positive node status was not (P=0.6) (17). The implication of this study contradicts less contemporary teachings advocating against the surgical intervention for patients with node positive disease, and supports the rationale that in well-selected patients surgical options may still be considered. Engel et al. demonstrated a survival benefit in patients who underwent RP with the findings of node positive disease at the time of surgery compared to those who had their surgery aborted (18). Additionally, Touijer et al. proposed the idea of a risk subclassification for patients with lymph node metastasis based upon their 2014 study that evaluated a cohort of 369 patients with node positive disease treated with surgery and lymph node dissection alone between 1988 and 2010. This was an overall younger cohort of patients (median age 62) with 322 (87%) of patients having at least cT3 disease (19). A total of 70 (18.9%) developed metastases. A higher number of positive nodes (three or more vs. one) was found to be a significant predictor of metastatic risk on multivariable analysis (HR =2.54, 95% CI, 1.38–4.69, P=0.03) (19). This was also found to be a significant predictor of BCR, which was noted in 201 patients (54%) (HR =2.61, 95% CI, 1.81–3.76, P<0.0001).
Cytoreductive prostatectomy
In the metastatic setting, cytoreductive approaches have been demonstrated as feasible options in the context of multimodal therapeutic approaches, and remains a focus of ongoing prospective trials. Studies in the preclinical setting demonstrated that after prostate resection in orthotopic mouse models implanted with prostate cancer cells, there is a demonstrable difference in the size and number of metastatic burden (20,21). Conceptually, the primary tumor has been referred to by other authors as a “premetastatic niche” as well as a source of “self-seeding” in which the tumor serves as a source of metastatic cells propagating further disease spread (21-24). In the clinical setting, subset analyses of larger studies have suggested benefits of patients who previously had undergone RP and later developed metastatic disease. This includes the 2002 study by Thompson et al. that evaluated patients in the Southwest Oncology Group (SWOG) Study 8894, evaluating the effects of previous primary treatment on men with subsequent metastatic disease. It was found that in those patients who had previously undergone RP, a significantly decreased risk of death was appreciated compared to those men who did not (HR =0.77, 95% CI, 0.53–0.89) (25).
Several retrospective studies include data on patients undergoing RP in the presence of metastatic disease. A 2014 study by Culp et al. evaluated SEER data to identify men diagnosed with stage IV (M1a-c) prostate cancer who were treated with RP, brachytherapy, or no surgery or radiation (NSR). Of a total of 8,185 patients, 245 were identified who underwent RP. After a median follow-up of 16 months, a total of 33 RP patients (13.5%) died (26). The 5-year OS and DSS were significantly higher in patients who underwent RP (67.4% and 75.8%, respectively vs. 22.5% and 48.7% for the NSR group, P<0.001) (26). Similar benefits were also noted in the group undergoing radiation therapy. Older patients (>70), those with PSA >20, and pelvic lymphadenopathy were demonstrated to have increased CSM and gain a more questionable benefit from local therapy. Interestingly, the authors found that the benefits of local therapy were experienced by patients irrespective of the extent of their metastatic disease. These findings were reproduced by researches in the Munich Cancer Registry (MCR) who evaluated a cohort of 1538 patients with metastatic disease, 74 (5%) of whom underwent RP. They found that the 5-year OS rate for the RP group was 55% compared to 21% in the group that did not undergo surgery (P<0.01) (27).
A 2017 study by Gandaglia evaluated a small cohort of eleven patients with oligometastatic disease (defined as 5 or fewer bone lesions at bone scan irrespective of nodal involvement). The median age of the cohort was 72 and the majority had excellent performance statuses (73% Charlson comorbidity index of 0). A majority of these patients were appreciated to have adverse features on final pathology with 10 (91%) having nodal invasion and 8 (73%) having positive margins (28). Additionally, 10 (91%) of men received adjuvant therapy. The 7-year clinical progression and CSM-free survival rates were 45% and 82%, respectively. This represents a highly selected patient cohort, the majority of which were in excellent health. However, this study lends support to the rationale for surgical benefit in these patients and the need for clinical trials.
Functional outcomes analysis
Shared decision making in prostate cancer treatment selection arguably plays a larger role than in other malignancies, due to the potential life-changing implications associated with each option. Various studies have demonstrated the implications of shared decision making applications as improving their decisional conflicts, decreasing decisional regret, and increasing overall prostate cancer knowledge (29,30). Shared decision making has also been found to preferred in patients who ultimately chose surgical intervention (31). However, the literature generally concludes that patient decision making is not often based upon one issue and instead varies widely based upon personal factors, patient values, and perceived success in cancer eradication. An extremely important area of consideration are the quality of life implications of each treatment modality. Particularly, how these may influence erectile function (EF) and urinary incontinence. In the era of robotic prostatectomy, return of potency and continence shows significant variability, dependent on numerous factors. Meta-analysis data indicates a wider range for recovery of EF and persistent incontinence at one year (54–90% vs. 4–31%, respectively) (32,33). In large studies, it would appear that the return of continence plays a more important role than potency, although this is again multi-factorial with significant variability (34,35). The obvious clinical questions inferred are whether the clinician should expect similar or potentially worse outcomes from a functional standpoint with surgical considerations in locally advanced or metastatic patients. This is more challenging when considering the majority of these patients will likely be receiving multi-modal treatment approaches, investigator variability in terms of potency or continence definitions, and regarding potency, whether nerve sparing approaches are offered (36).
Ou et al. performed a single surgeon, prospective evaluation of patients undergoing RARP defined by low, intermediate, and high risk cases. High risk cases were defined as those with cT2a or T3 disease, PSA >20 ng/mL, or Gleason 8–10 disease (37). Preservation of the neurovascular bundle was performed in 30 of 148 (20.27%) of high risk patients, with 14 (9.4%) having bilateral preservation. Of these with bilateral nerve preservation, continence (defined as no pad use), potency (defined as being able to achieve erection sufficient for intercourse with or without phosphodiesterase (PDE) medication), and BCR free rate was achieved in 92.8%, 71.4%, and 92.8% respectively (37). These findings are similar to data published by Pierorazio et al. of a cohort of 416 patients treated by a single surgeon from 1988–2005. Using similar criteria to the Ou study, a total of 47 high risk patients were identified. At one year, the cumulative continence and potency rates were reported as 93.3% and 69.6%, respectively (38). A recognized issue with this study was a lack of validated questionnaires for QOL outcomes available at the time, creating obvious limitations.
Abdollah et al. conducted a large retrospective multi institutional study evaluating a cohort of 769 patients with high risk disease. The primary aim of this study was to assess the three-year recovery rate of urinary continence and sexual function. Continence was defined as the use of zero vs. one safety pad per day whereas sexual function was defined as a Sexual Health Inventory in Men (SHIM) score of 17 or more (39). A majority of these patients (62.1%) had pT3a or higher disease. The authors noted that at 3 years, 91.2% of men had recovered their urinary continence, which was importantly noted to have increased in each subsequent year since surgery, suggesting the potential for continued recovery of function beyond the initial one year mark (39). Regarding EF, this study is crucial in outlining important concepts. A total of 548 (71.3%) of men in this study were potent pre-operatively according to the author’s definition. Of these, 69% regained their potency at three years. Additionally, 87.7% of men in the cohort underwent some degree of nerve preservation at the time of surgery. As expected, nerve preservation and preoperative SHIM scores were found to be positively correlated with the recovery in these functions in the postoperative setting (39). This data contrasts with that of Recabal et al. who performed a retrospective review of a cohort of 584 patients with high risk features (PSA >20, cT3 or greater, biopsy Gleason grade 8–10) who underwent RP between 2006–2012. A total of 515 (88.2%), underwent some degree of nerve sparing (40). However, a much smaller number of patients (160, 31.1%), had preoperative potency and only 47% (75 patients) were able to regain their EF at two years.
In the cytoreductive prostatectomy realm, in the aforementioned Gandaglia et al. study, the authors reported a 90-day continence rate in only 3 patients (27%) along with higher overall perioperative adverse outcomes, potentially attributable to a need for extensive local and nodal dissection due to disease aggressiveness in the oligometastatic population (28). Considerations for this study should also include that 10 (91%) received some form of adjuvant therapies. Return of EF was not mentioned in this study. A 2018 study by Heidenreich et al. retrospectively evaluated a larger cohort of 113 patients with metastatic disease, limited bulky pelvic lymphadenopathy, and minimal visceral metastatic sites. Similar to the Gandaglia study, an overwhelming proportion of patients in this cohort (91, 86.5%), underwent adjuvant therapies. Interestingly, this study reported a 68.1% rate of no urinary incontinence vs. only a 14.1% rate of severe (>2 pads/day) symptoms (41). EF was also not discussed as a functional outcome in this study.
Safety and feasibility
The ability to safely perform surgical prostatectomy with an acceptable risk profile is crucial for presenting resection as a reasonable option during management selection. Multiple studies have evaluated the complication profile in their study cohort. A 2016 retrospective study by Sooriakumaran et al. evaluated a total of 106 patients with metastatic prostate cancer who underwent surgical resection to evaluate for perioperative and short term complications. 90-day overall complication rates as well as specific outcomes, readmission, and reoperation rates were evaluated, among others. The authors found that 79.2% of all patients did not experience any complications (42). However, it was also noted that the cohort experienced a higher rate of lymphocele (8.5%) and wound infection (4.7%) when compared to a cohort of patients who underwent open prostatectomy for standard indications. The authors concluded that in meticulously selected patients, surgery can be a safe and feasible option (42,43).
The previously mentioned study by Heidenreich et al. reported complications in 38 total patients (33.6%), the majority of which (27, 71%) were grade I and II based on the Clavien-Dindo classification system (41). Of these, a total of 10 patients experienced anastomotic leak while fewer experienced lymphocele (3) than in the Sooriakumaran study. A total of 6 patients (5.3%) did experience a Clavien IIIb complication, including four who required repeat laparotomy for bleeding concerns (41).
A 2019 study evaluated 36 patients with metastatic disease who underwent surgical intervention. Key points from this study were a high rate of positive surgical margins (21, 65.6%) (44). The overall 90-day complication rate was reported at 31.2%, with a rate of high-grade complications of 6.25%. The major complications reported were acute tubular necrosis requiring temporary dialysis, as well as one reported death in a patient who as discharged home on postoperative day 2 and died at home of unknown causes two days later (44). 25% of patients experienced minor complications including four patients with an anastomotic leak and one who developed a paralytic ileus.
Previously discussed indications for nerve sparing with the hope of preserving EF should be balanced against the potential for increased positive margin rates. This is reflected in the Recabal study, where 24% of patients who underwent some degree of nerve sparing experienced a positive margin (40).
A 2014 SEER based study evaluated a total of 1,512 patients who underwent prostatectomy via a robotic or open approach. The main focus of this study was to evaluate the feasibility of robotic prostatectomy in the high-risk setting (45). After propensity matching, a total of 706 patients were evaluated. The authors did not appreciate any differences in complication rates between the cohorts, but did find that the robotic cohort had a lower rate of blood transfusion and length of hospitalization compared to the open cohort, suggesting that this may be an optimal approach in the surgical management of high risk patients (45).
Future directions
RP in high risk and metastatic disease is an emerging area of focus and the subject of several ongoing clinical trials. NCT03655886 is a feasibility study randomizing patients with good performance status and radiographically confirmed metastatic prostate cancer to either undergo surgical resection or whole pelvis radiation. Aside from proving feasibility, the secondary outcome is the measurement of time until castrate-resistant disease is developed between the two arms. To be considered, patients must be ECOG 0-1 with a newly diagnosed metastatic prostate cancer based on CT or bone scan imaging. Exclusion criteria include those patients with previous pelvic radiation or surgery, symptomatic metastases (that persist after ADT initiation), and brain metastases.
A similar study recruiting out of the United States is NCT03456843 which is a randomized phase II trial evaluating the efficacy of combining RP with systemic therapy compared to systemic therapy alone. The primary outcome is failure free survival other survival parameters being considered as secondary outcomes as well as quality of life considerations. Similar to other studies, patients must have imaging or biopsy confirmed metastatic lesions and not have undergone any previous local therapy. They must have excellent performance status, be deemed resectable by a surgeon, and also not demonstrate anemia (hemoglobin less than 9 g/dL), thrombocytopenia (Platelets <80,000/mcL), or have any liver enzyme abnormalities.
SPCG-15 is a multi-institutional study based out of Europe that is evaluating surgery with or without combination radiation therapy compared to radiation therapy and ADT in patients with locally advanced prostate cancer, defined as evidence of extracapsular extension and the presence of Gleason grade pattern 4 disease. Patients cannot have the presence of lymph node metastasis or distant metastatic disease. The primary outcome measurement is cause-specific survival while secondary outcomes include metastasis free survival and questionnaire-based quality of life outcomes. Exclusion criteria for this study include patients that have PSA values greater than 100 ng/mL, a previous cancer diagnosis (except non-melanoma skin cancer), or significantly abnormal laboratory findings.
Southwest Oncology Group (SWOG) 1802 is an ongoing phase III clinical trial comparing the use of standard systemic therapy with or without the addition of definitive treatment including prostatectomy or radiation therapy in the treatment of metastatic prostate cancer. Eligible patients include those with biopsy proven adenocarcinoma of the prostate without prior local therapy and confirmed metastatic disease by conventional imaging, or confirmed on biopsy. Those with brain metastases are excluded. The comparator arm includes those patients treated with an accepted systemic therapy agent. Those patients in the experimental arm are given systemic therapy as an induction to be followed by prostatectomy within 8 weeks or radiation within 4 weeks of randomization. The primary outcome is overall survival with additional secondary outcomes to be evaluated as well.
Conclusions
While prostatectomy for advanced or metastatic prostate cancer may have been previously not considered, there is continued momentum around its use. Contemporary data supports promising outcome measures in patients treated with prostatectomy, with the understanding that this is likely most effective as part of a multimodality approach. These approaches have been demonstrated to be safe and feasible, particularly in the setting of large centers and experienced surgeons. Along these lines, with appropriate patient selection and surgical technique, quality of life can be spared. However, there are remaining challenges that have not yet been addressed. Given the heterogeneity of treatment modalities, it is difficult to accurately ascertain the benefits of surgical resection. Ongoing clinical trials are actively recruiting and the results of these should provide further insight. Quality of life considerations are also difficult to accurately measure given a lack of standard reporting and assessment measures, along with the difficult balance of obtaining optimal oncologic control while attempting to preserve a patient’s sexual and urinary function. Further studies may help to provide for better standardization in this regard. However, limited data to this point suggests an ongoing role of surgical resection in the management of advanced prostate malignancy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marc C. Smaldone and Jeffrey J. Tomaszewski) for the series “Controversies in Minimally Invasive Urologic Oncology” published in Translational Andrology and Urology. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-20-1002). The series “Controversies in Minimally Invasive Urologic Oncology” was commissioned by the editorial office without any funding or sponsorship. Dr. BFC reports other from Janssen Pharmaceuticals, other from Blue Earth Disgnostics, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Carroll PH, Mohler JL. NCCN Guidelines Updates: Prostate Cancer and Prostate Cancer Early Detection. J Natl Compr Canc Netw 2018;16:620-3. [Crossref] [PubMed]
- Fleshner K, Carlsson SV, Roobol MJ. The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol 2017;14:26-37. [Crossref] [PubMed]
- Stephenson AJ, Scardino PT, Eastham JA, et al. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Natl Cancer Inst 2006;98:715-7. [Crossref] [PubMed]
- Cronin KA, Lake AJ, Scott S, et al. Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics. Cancer 2018;124:2785-800. [Crossref] [PubMed]
- Lowrance WT, Elkin EB, Yee DS, et al. Locally advanced prostate cancer: a population-based study of treatment patterns. BJU Int 2012;109:1309-14. [Crossref] [PubMed]
- Thompson IM Jr, Tangen CM, Paradelo J, et al. Adjuvant radiotherapy for pathologically advanced prostate cancer: a randomized clinical trial. Jama 2006;296:2329-35. [Crossref] [PubMed]
- He J, Albertsen PC, Moore D, et al. Validation of a Contemporary Five-tiered Gleason Grade Grouping Using Population-based Data. Eur Urol 2017;71:760-3. [Crossref] [PubMed]
- Kearns JT, Holt SK, Wright JL, et al. PSA screening, prostate biopsy, and treatment of prostate cancer in the years surrounding the USPSTF recommendation against prostate cancer screening. Cancer 2018;124:2733-9. [Crossref] [PubMed]
- Eapen RS, Herlemann A, Washington SL 3rd, et al. Impact of the United States Preventive Services Task Force 'D' recommendation on prostate cancer screening and staging. Curr Opin Urol 2017;27:205-9. [Crossref] [PubMed]
- Gaylis FD, Choi JE, Hamilton Z, et al. Change in prostate cancer presentation coinciding with USPSTF screening recommendations at a community-based urology practice. Urol Oncol 2017;35:663.e1-7. [Crossref] [PubMed]
- Tilki D, Chen MH, Wu J, et al. Surgery vs. Radiotherapy in the Management of Biopsy Gleason Score 9-10 Prostate Cancer and the Risk of Mortality. JAMA Oncol 2019;5:213-20. [Crossref] [PubMed]
- Kishan AU, Cook RR, Ciezki JP, et al. Radical Prostatectomy, External Beam Radiotherapy, or External Beam Radiotherapy With Brachytherapy Boost and Disease Progression and Mortality in Patients With Gleason Score 9-10 Prostate Cancer. Jama 2018;319:896-905. [Crossref] [PubMed]
- Jang TL, Patel N, Faiena I, et al. Comparative effectiveness of radical prostatectomy with adjuvant radiotherapy versus radiotherapy plus androgen deprivation therapy for men with advanced prostate cancer. Cancer 2018;124:4010-22. [Crossref] [PubMed]
- Feldman AS, Meyer CP, Sanchez A, et al. Morbidity and Mortality of Locally Advanced Prostate Cancer: A Population Based Analysis Comparing Radical Prostatectomy versus External Beam Radiation. J Urol 2017;198:1061-8. [Crossref] [PubMed]
- Moris L, Cumberbatch MG, Van den Broeck T, et al. Benefits and Risks of Primary Treatments for High-risk Localized and Locally Advanced Prostate Cancer: An International Multidisciplinary Systematic Review. Eur Urol 2020;77:614-27. [Crossref] [PubMed]
- Seisen T, Vetterlein MW, Karabon P, et al. Efficacy of Local Treatment in Prostate Cancer Patients with Clinically Pelvic Lymph Node-positive Disease at Initial Diagnosis. Eur Urol 2018;73:452-61. [Crossref] [PubMed]
- Moschini M, Briganti A, Murphy CR, et al. Outcomes for Patients with Clinical Lymphadenopathy Treated with Radical Prostatectomy. Eur Urol 2016;69:193-6. [Crossref] [PubMed]
- Engel J, Bastian PJ, Baur H, et al. Survival benefit of radical prostatectomy in lymph node-positive patients with prostate cancer. Eur Urol 2010;57:754-61. [Crossref] [PubMed]
- Touijer KA, Mazzola CR, Sjoberg DD, et al. Long-term outcomes of patients with lymph node metastasis treated with radical prostatectomy without adjuvant androgen-deprivation therapy. Eur Urol 2014;65:20-5. [Crossref] [PubMed]
- Cifuentes FF, Valenzuela RH, Contreras HR, et al. Surgical cytoreduction of the primary tumor reduces metastatic progression in a mouse model of prostate cancer. Oncol Rep 2015;34:2837-44. [Crossref] [PubMed]
- Metcalfe MJ, Smaldone MC, Lin DW, et al. Role of radical prostatectomy in metastatic prostate cancer: A review. Urol Oncol 2017;35:125-34. [Crossref] [PubMed]
- Kaplan RN, Psaila B, Lyden D. Bone marrow cells in the 'pre-metastatic niche': within bone and beyond. Cancer Metastasis Rev 2006;25:521-9. [Crossref] [PubMed]
- Sánchez CA, Andahur EI, Valenzuela R, et al. Exosomes from bulk and stem cells from human prostate cancer have a differential microRNA content that contributes cooperatively over local and pre-metastatic niche. Oncotarget 2016;7:3993-4008. [Crossref] [PubMed]
- Comen E, Norton L, Massague J. Clinical implications of cancer self-seeding. Nat Rev Clin Oncol 2011;8:369-77. [Crossref] [PubMed]
- Thompson IM, Tangen C, Basler J, et al. Impact of previous local treatment for prostate cancer on subsequent metastatic disease. J Urol 2002;168:1008-12. [Crossref] [PubMed]
- Culp SH, Schellhammer PF, Williams MB. Might men diagnosed with metastatic prostate cancer benefit from definitive treatment of the primary tumor? A SEER-based study. Eur Urol 2014;65:1058-66. [Crossref] [PubMed]
- Gratzke C, Engel J, Stief CG. Role of radical prostatectomy in metastatic prostate cancer: data from the Munich Cancer Registry. Eur Urol 2014;66:602-3. [Crossref] [PubMed]
- Gandaglia G, Fossati N, Stabile A, et al. Radical Prostatectomy in Men with Oligometastatic Prostate Cancer: Results of a Single-institution Series with Long-term Follow-up. Eur Urol 2017;72:289-92. [Crossref] [PubMed]
- Johnson DC, Mueller DE, Deal AM, et al. Integrating Patient Preference into Treatment Decisions for Men with Prostate Cancer at the Point of Care. J Urol 2016;196:1640-4. [Crossref] [PubMed]
- van Stam MA, Pieterse AH, van der Poel HG, et al. Shared Decision Making in Prostate Cancer Care-Encouraging Every Patient to be Actively Involved in Decision Making or Ensuring the Patient Preferred Level of Involvement? J Urol 2018;200:582-9. [Crossref] [PubMed]
- Sidana A, Hernandez DJ, Feng Z, et al. Treatment decision-making for localized prostate cancer: what younger men choose and why. Prostate 2012;72:58-64. [Crossref] [PubMed]
- Ficarra V, Novara G, Ahlering TE, et al. Systematic review and meta-analysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol 2012;62:418-30. [Crossref] [PubMed]
- Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2012;62:405-17. [Crossref] [PubMed]
- Holmboe ES, Concato J. Treatment decisions for localized prostate cancer: asking men what's important. J Gen Intern Med 2000;15:694-701. [Crossref] [PubMed]
- Zeliadt SB, Ramsey SD, Penson DF, et al. Why do men choose one treatment over another?: a review of patient decision making for localized prostate cancer. Cancer 2006;106:1865-74. [Crossref] [PubMed]
- Yuh B, Artibani W, Heidenreich A, et al. The role of robot-assisted radical prostatectomy and pelvic lymph node dissection in the management of high-risk prostate cancer: a systematic review. Eur Urol 2014;65:918-27. [Crossref] [PubMed]
- Ou YC, Yang CK, Wang J, et al. The trifecta outcome in 300 consecutive cases of robotic-assisted laparoscopic radical prostatectomy according to D'Amico risk criteria. Eur J Surg Oncol 2013;39:107-13. [Crossref] [PubMed]
- Pierorazio PM, Spencer BA, McCann TR, et al. Preoperative risk stratification predicts likelihood of concurrent PSA-free survival, continence, and potency (the trifecta analysis) after radical retropubic prostatectomy. Urology 2007;70:717-22. [Crossref] [PubMed]
- Abdollah F, Dalela D, Sood A, et al. Functional outcomes of clinically high-risk prostate cancer patients treated with robot-assisted radical prostatectomy: a multi-institutional analysis. Prostate Cancer Prostatic Dis 2017;20:395-400. [Crossref] [PubMed]
- Recabal P, Assel M, Musser JE, et al. Erectile Function Recovery after Radical Prostatectomy in Men with High Risk Features. J Urol 2016;196:507-13. [Crossref] [PubMed]
- Heidenreich A, Fossati N, Pfister D, et al. Cytoreductive Radical Prostatectomy in Men with Prostate Cancer and Skeletal Metastases. Eur Urol Oncol 2018;1:46-53. [Crossref] [PubMed]
- Sooriakumaran P, Karnes J, Stief C, et al. A Multi-institutional Analysis of Perioperative Outcomes in 106 Men Who Underwent Radical Prostatectomy for Distant Metastatic Prostate Cancer at Presentation. Eur Urol 2016;69:788-94. [Crossref] [PubMed]
- Jaber Y, Reichard CA, Chapin BF. Emerging role of cytoreductive prostatectomy in patients with metastatic disease. Transl Androl Urol 2018;7:S505-13. [Crossref] [PubMed]
- Yuh BE, Kwon YS, Shinder BM, et al. Results of Phase 1 study on cytoreductive radical prostatectomy in men with newly diagnosed metastatic prostate cancer. Prostate Int 2019;7:102-7. [Crossref] [PubMed]
- Gandaglia G, Abdollah F, Hu J, et al. Is robot-assisted radical prostatectomy safe in men with high-risk prostate cancer? Assessment of perioperative outcomes, positive surgical margins, and use of additional cancer treatments. J Endourol 2014;28:784-91. [Crossref] [PubMed]


