
The clinical research of 1,470 nm laser in percutaneous nephrolithotomy
Introduction
Urinary calculus is a disease with a high incidence among urological diseases, and renal calculus is the main birthplace of urinary calculus. Kidney stone is a kind of stone formed by some components of urine in the kidney, which leads to some diseases with urinary symptoms. The formation process of kidney stones is caused by some factors, such as the increase of concentration or the decrease of solubility of stone-forming substances in urine, supersaturation, precipitation of crystals, local growth and accumulation, and finally formation of stones. Kidney stones should be differentiated from ureteral stones, bladder stones and urethral stones. According to the location of pain, hematuria, signs of renal percussion pain and imaging examination, the diagnosis can be made clearly. For the treatment of kidney stones, percutaneous nephrolithotomy (PCNL) is a standard minimally invasive operation. Compared with open surgery, it has the advantages of less trauma, quick recovery, and high cure rate (1,2). It is challenging dealing with puncture channel bleeding and calyceal neck bleeding during PCNL operation, which often requires an indwelling nephrostomy tube to stop bleeding after the operation. Indwelling nephrostomy tube increases the incidence of postoperative waist pain and discomfort and postoperative infection and prolongs the hospital stay (3-5). To control bleeding and improve patients' postoperative comfort, scholars at home and abroad have attempted to use cylindrical balloon tubes to create a fistula or absorbable hemostatic material to fill the channel (6-8), and use post-operation plasma/vaporization electrodes to stop bleeding in the skin and kidney channel (9). From March 2016 to September 2019, our team used the characteristics of the 1,470 nm laser to stop bleeding in 20 of 42 PCNL patients and observed various indexes of its application effect during and after the operation. We aimed to improve the safety of PCNL and the postoperative comfort of patients in our hospital. Its effect is remarkable, and its safety is high, reported as follows.
We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/tau-20-1224).
Methods
General information
From March 2016 to September 2019, 42 patients with renal calculi were selected as PCNL. All patients were diagnosed by urinary B-ultrasound or Computed Tomography (CT) before the operation, and some complicated kidney stones were examined by magnetic resonance urography (MRU) or three-dimensional imaging before the operation. This study received ethical approval from the ethics committee of clinical medical research, drugs, instruments, and new technologies in the Second Affiliated Hospital of Wannan Medical College (No. WYEFYLS201601).
Inclusion criteria: (I) the diameter of a single stone is between 1.5 and 3.0 cm, and multiple unilateral kidney stones or stones at the ureteropelvic junction with hydronephrosis are apparent; (II) no previous history of open kidney surgery; (III) can fully understand and cooperate, informed consent of the operation and sign. Exclusion criteria: (I) cast, staghorn kidney stone or complex kidney stone with a maximum diameter greater than 3.0 cm and high CT value; (II) renal infection or urinary tract malformation; (III) complicated with severe circulatory diseases and abnormal coagulation function; (IV) poor general condition before the operation, disagreeing with participants. All surgical patients signed informed consent, which was examined and approved by the Medical Ethics Committee of our hospital. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
We divided the patients with an indwelling nephrostomy tube and a double J tube into the traditional operation group. Only double J tubes were indwelled without nephrostomy, which was treated by laser surgery. Twenty cases without nephrostomy after PCNL were randomly selected as laser surgery groups. Twenty-two patients with the same number of puncture passages and similar stone volumes were selected as the traditional operation group. There was no significant difference between the two groups in gender, age, BMI index, diameter, and location of kidney stones (P>0.05, see Table 1), which was comparable.
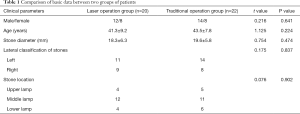
Full table
The patients were divided into the traditional operation group after the operation and the double J tube. The double J tube without renal fistulas was used as the laser operation group. Twenty cases without renal fistulas after PCNL operation were randomly selected as the laser operation group. The 22 patients who had the same number of puncture channels and a similar volume of stones were the traditional operation group. The two groups had no significant difference in gender, age, BMI index, diameter, and location of renal calculus (P>0.05, see Table 1).
Surgical methods
There are no surgical contraindications in the preoperative evaluation of the two groups of patients, all of whom are under general anesthesia. After adequate anesthesia, the cystolithotomy position is taken, disinfected, and draped. First, the 5F ureteral catheter is retrogradely placed on the affected side with a hard ureteroscope, and the distal end connects to a self-constructed artificial pressure device to form artificial hydronephrosis. The 16F urinary catheter supports catheterization, and the ureteral catheter is fixed on the catheter. Change the prone position, pad the abdomen high, lower the head and lower the feet, and fully expand the intercostal space. Disinfect again, spread the towel, position the target calices for puncture under the guidance of color Doppler B-mode ultrasound, observe the puncture depth after a successful puncture, retain the guide-wire, cut the skin to the dermis, expand it from 6F to 20F along the guide-wire with the dilator in turn, and retain the 20F working sheath. The nephoscopy was placed in the working sheath to search for stones, and ultrasonic/pneumatic ballistic lithotripsy was performed with the EMS system.
Traditional operation group: after the operation, an 18F nephrostomy tube was placed in the working sheath, the stoma was sutured and fixed, and the nephrostomy tube was closed for 2 hours and then opened according to the bleeding situation.
Laser operation group: If it is found the unclear operation field affects the lithotripsy due to bleeding during the operation, a 1,470 nm laser will be used to stop bleeding at once. After the stone is removed, the 5F double J tube is retained, the 1,470 nm optical fiber (straight out and side out) is replaced, and the electrocoagulation power is set at 40 W. To avoid the oscillation of the optical fiber, we put the optical fiber into the self-produced metal control rod, with the head end exposed slightly and the tail end fixed. At first, the active bleeding points of renal pelvis and calyces were treated with electrocoagulation to stop bleeding, then retreated to the inner edge of the cutaneous renal channel, rotated, and retreated the skinning sheath, and immediately treated with electrocoagulation to stop bleeding until the renal capsule. Withdraw from the nephoscopy and peel the sheath. Water that was clear flowed out of the channel, followed by a suture of the muscular layer, subcutaneous layer, and skin.
On the second day after the operation, B-ultrasound was reexamined in both groups to determine the perirenal condition and the position of double J tubes. After reexamining urinary CT or B-ultrasound in the 3rd week after the operation, it was found there was no apparent residual stone, and then the double J tube was pulled out, and the residual stone with a diameter less than 3 mm was meaningless. In the catheterization group, the nephrostomy fistula was pulled out after reexamination on the third day after the operation.
Observation and comparison of various indicators
The stone clearance rate, the incidence of postoperative complications (urinary extravasation, intrarenal infection, channel bleeding, channel pain, postoperative hematuria), operation time, intraoperative blood loss, medical expenses, average postoperative hospital stay, and other data were observed and compared between the two groups.
Statistical analysis
Statistical methods were analyzed by SPSS 21.0 software, the measurement data were expressed by mean, standard deviation, t-test made the comparison, and the comparison of counting data was made by c2 test, P<0.05 was statistically significant.
Results
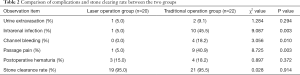
Comparison of postoperative complications and stone clearance rate between the two groups
There was no significant difference in stone clearance rate, urine extravasation, and postoperative hematuria between the two groups (P>0.05). However, the incidence of intrarenal infection, channel pain, and channel bleeding in the laser surgery group were lower than those in the traditional surgery group, and the difference was statistically significant (P<0.05, see Table 2).
Full table
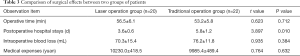
Comparison of clinical indexes between two groups of patients
There was no significant difference in operation time, blood loss, and medical expenses between the two groups (P>0.05). However, the average postoperative hospital stay in the laser surgery group was shorter than that in the traditional surgery group, and the difference was statistically significant (P<0.05, see Table 3).
Full table
Discussion
Nowadays, PCNL is still an indispensable way to treat upper urinary tract stones (10). However, the significant risk of PCNL is the bleeding of the cutaneous renal channel or mucous membrane of the renal pelvis and calyceal, which not only increases the difficulty of lithotripsy and stone removal but also prolongs the operation time and increases the postoperative complications. To achieve the goals of compressing the skin and kidney channel to stop bleeding, draining urine to prevent infection, and removing residual stones in the second stage (11), most patients still have nephrostomy tubes after PCNL. With the retention of a nephrostomy fistula, most patients have apparent discomfort, which also increases the possibility of bleeding, infection, and other complications (12).
In recent years, with the improvement of medical instruments and PCNL technology, various new surgical instruments have been widely used in this operation, the primary purpose of which is to improve the safety and effectiveness of the operation, reduce postoperative complications and increase patients' comfort. Among them, it has been one of the contents of discussion on whether the conventional indwelling nephrostomy tube is needed after PCNL operation. Some scholars have adopted completely tubeless (no nephrostomy tube, double J tube), but the author hypothesizes the precondition of tubeless is complete hemostasis during operation or no visible bleeding on the wound surface of the tunnel. Although there are several hemostatic methods in PCNL, the effect is not satisfactory, especially for beginners. Since the development of 1,470 nm laser technology in our hospital, it has been found it has several advantages. Its advantages are initially reflected in the vaporization cutting of soft tissues, including prostatic hyperplasia and bladder tumors. The laser has the advantages of small thermal damage to soft tissues and strong controllability. It can accurately control the depth and range of tissues by using contact electrocoagulation, thus achieving the effect of rapid hemostasis (13). According to the above characteristics of the 1,470 nm laser, the author assumes PCNL is also effective in hemostasis of renal pelvis and calyceal hemorrhage, especially cutaneous renal channel hemorrhage, rarely reported in domestic literature. Through this study, the characteristics and practical scope of the laser are further confirmed, and an innovative method is also supplied for PCNL to stop bleeding through the skin and kidney channel.
Color Doppler B-ultrasound successfully punctured all patients in this study group, the channel was established satisfactorily, the operation process was smooth, the rate of stone removal was high after the operation, there was no pleural effusion, no other organ injury, no major bleeding and other complications during the operation. There were 4 cases (13.6%) of bleeding in the traditional operation group after the operation, the amount of bleeding was 800–1,400 mL, with an average of (1,142±80) ml. After symptomatic treatment for 2 days, there were still 2 cases of intermittent massive bleeding, which got better after emergency selective renal arteriography embolization. The causes of persistent bleeding after operation may be the tearing of renal pelvis or calyces, perforation of mucous membranes, rupture of small renal vessels, among many others. However, the intermittent bleeding after operation may be complicated with renal arteriovenous fistula or pseudoaneurysm (14). However, none of the patients in the laser surgery group had massive postoperative bleeding. These results may be caused by using a 1,470 nm laser to coagulate and stop bleeding at the bleeding points of the renal pelvis, calyceal neck, and cutaneous renal channel during operation. These procedures were done to achieve a clear operation field, reduce postoperative bleeding, and avoid postoperative bleeding due to friction of the nephrostomy fistula. Its principle is the same as a 1,470 nm laser in prostatectomy. Due to the small sample size, it is necessary to expand the sample size further to support this view.
Some scholars have found the rate of stone clearance is similar between completely and partially without tubes (only double J tubes are reserved), and the incidence of postoperative urinary fistula, hematuria, and renal colic is low (15), which is like the results of this study. There is no significant difference in postoperative complications between the two groups, but the incidence of postoperative infection in the tube group 6 (27.3%) is significantly higher than that in the non-tube group 1 (5.0%). The comparison between the two groups is statistically significant. Some scholars believe the puncture channel of the non-tube PCNL is closed in time after the operation, which reduces the contact between the renal environment and the outside world and reduces the risk of retrograde infection after nephrostomy (16). The incidence of postoperative pain in 9 cases (40.9%) of the managed group was significantly higher than that in 1 case (5.0%) of the non-managed group, which was consistent with the research results of some scholars (17,18). This study found although there was a significant difference in the postoperative hospital stay between the two groups (P<0.05), there was no significant difference in the operation time and intraoperative blood loss, which was consistent with the research results of Chung (19). We hypothesize that several factors influence operation time, including the skill of the operator, the cooperation degree of the team, the instruments used, among many others.
In the laser surgery group, one patient showed moderate to severe hydronephrosis by CT before the operation. After obtaining the consent of the client during operation, the nephrostomy was not kept after the operation. The patient had a good prognosis and no related complications. The author believes not all patients need to stop bleeding or indwelling nephrostomy in PCNL surgery, which has an excellent relationship with the selection of puncture points, surgical skills, clinical experience, renal parenchyma thickness, stone location, and other factors. However, the 1470 nm laser has a visible hemostatic effect for patients with apparent bleeding in the skin and kidney channel, more thorough than other methods.
To reduce the risk of bleeding and improve operation efficiency, the author improved some instruments in PNCL. (I) Selection of skin and kidney channel: instead of the previous standard channel, i.e., the metal nested 24F working channel, the 20F skinning sheath is used, which has the advantage of elasticity and shape variability and the tearing rate of the calyceal neck when nephroscope swings during operation are significantly lower than the standard channel metal sheath (20). Also, it is more convenient to take out stones by using foreign body forceps under nephroscope, and even if the shape of stones is irregular, stones can be taken out by changing the shape of the skinning sheath, which significantly improves the efficiency of stone cleaning. (II) To prevent the 1,470 nm semiconductor laser fiber from swinging excessively in the nephroscope, we put the fiber out of the self-made metal rod, fixed the distal end of the fiber with sterile transparent paste, leaked the proximal end of the fiber (straight bundle fiber 0.3 cm, side bundle fiber 0.8–1.0 cm). Then, we rotated and unsheathed it, and found that arterial bleeding was given non-contact electrocoagulation. This effectively reduced the risk of channel bleeding and postoperative venous fistula bleeding. (III) 1,470 nm laser electrocoagulation can also be used to stop bleeding due to friction, bleeding between stones, and renal pelvis/calyceal mucosa, calyceal neck fissure, among many others. Through the above improvements, the operation time is shortened, the risk of bleeding is reduced, and the operation safety is improved.
Together, this study found that the use of 1,470 nm laser in PCNL surgery can reduce intraoperative and postoperative bleeding, reduce the risk of surgery, improve the effectiveness of surgery, and provide an innovative method for postoperative management. The hemostatic effect is better for the inconspicuous hydronephrosis, because the renal parenchyma is thick and the blood vessels are not easy to retract. If the puncture channel bleeds, it is satisfactory to use 1470 laser to stop bleeding. If the bleeding in the false channel occurs when the straight-out laser is used to stop bleeding, the side-out laser should be used to stop bleeding. For channel bleeding with heavy accumulated water, the pressure of perfusion water should be reduced when stopping bleeding, so as to prevent water from seeping out to the periphery of kidney. Indwelling nephrostomy fistula after hemostasis. We now use high-definition B-ultrasound to visually locate the puncture in kidney puncture, which can avoid the main blood vessels, not only reduce the chance of damaging blood vessels during puncture, but also reduce the kidney damage caused by multiple punctures. Therefore, the application of this laser in PCNL is safe, effective, and feasible, and it is worth popularizing. With the improvement of PCN operation technology and medical equipment, the risk rate of PCN operation will be reduced, the safety of operation will be improved, and the postoperative comfort of patients will be better.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (grant number 81601806).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/tau-20-1224
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tau-20-1224
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-20-1224). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All surgical patients signed informed consent, which was examined and approved by the Medical Ethics Committee of our hospital. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Knoll T, Daels F, Desai J, et al. Percutaneous nephrolithotomy: technique. World J Urol 2017;35:1361-8. [Crossref] [PubMed]
- Scotland K, Lange D. The link between antibiotic exposure and kidney stone disease. Ann Transl Med 2018;6:371. [Crossref] [PubMed]
- ElSheemy MS, Elmarakbi AA, Hytham M, et al. Mini vs standard percutaneous nephrolithotomy for renal stones: a comparative study. Urolithiasis 2019;47:207-14. [Crossref] [PubMed]
- Xun Y, Wang Q, Hu H, et al. Tubeless versus standard percutaneous nephrolithotomy: an update meta-analysis. BMC Urol 2017;17:102. [Crossref] [PubMed]
- Nalbant I, Ozturk U, Sener NC, et al. The comparison of standard and tubeless percutaneous nephrolithotomy procedures. Int Braz J Urol 2012;38:795-800. [Crossref] [PubMed]
- Nagele U, Schilling D, Anastasiadis AG, et al. Closing the tract of mini-percutaneous nephrolithotomy with gelatine matrix hemostatic sealant can replace nephrostomy tube placement. Urology 2006;68:489-93. [Crossref] [PubMed]
- Noller MW, Baughman SM, Morey AF, et al. Fibrin sealant enables tubeless percutaneous stone surgery. J Urol 2004;172:166-9. [Crossref] [PubMed]
- Koo KC, Park SU, Jang HS, et al. Tubeless percutaneous nephrolithotomy with non-absorbable hemostatic sealant (Quikclot®) versus nephrostomy tube placement: a propensity score-matched analysis. Urolithiasis 2015;43:527-33. [Crossref] [PubMed]
- Jou YC, Cheng MC, Sheen JH. Cauterization of access tract for nephrostomy tube-free percutaneous nephrolithotomy. J Endourol 2004;18:547-9. [Crossref] [PubMed]
- Ghani KR, Andonian S, Bultitude M, et al. Percutaneous nephrolithotomy: update, trends, and future directions. Eur Urol 2016;70:382-96. [Crossref] [PubMed]
- Bearelly P, Lis C, Trussler J, et al. Nephrostomy tube placement prior to percutaneous nephrolithotomy does not impact outcomes. Can J Urol 2018;25:9497-502. [PubMed]
- Garofalo M, Pultrone CV, Schiavina R, et al. Tubeless procedure reduces hospitalization and pain after percutaneous nephrolithotomy: results of a multivariable analysis. Urolithiasis 2013;41:347-53. [Crossref] [PubMed]
- Giglio NC, Hutchens TC, Perkins WC, et al. Rapid sealing and cutting of porcine blood vessels, ex vivo, using a high-power, 1470-nm diode laser. J Biomed Opt 2014;19:38002. [Crossref] [PubMed]
- Adhikari MB, Karna S, Kasaju A. Safety and efficacy of bilateral simultaneous percutaneous nephrolithotomy. J Nepal Health Res Counc 2019;17:114-8. [Crossref] [PubMed]
- Agrawal MS, Sharma M, Agarwal K. Tubeless Percutaneous Nephrolithotomy Using Antegrade Tether: A Randomized Study. J Endourol 2014;28:644-8. [Crossref] [PubMed]
- S Merinov D, Gurbanov SS, Artemov AV, et al. Prevention of bleeding during tubeless percutaneous nephrolithotomy. Urologiia 2019.38-43. [PubMed]
- Tirtayasa PMW, Yuri P, Birowo P, et al. Safety of tubeless or totally tubeless drainage and nephrostomy tube as a drainage following percutaneous nephrolithotomy: a comprehensive review. Asian J Surg 2017;40:419-23. [Crossref] [PubMed]
- Zhang LJ, Ye XJ, Huang XB, et al. Comparison of tubeless-percutaneous nephrolithotomy and ureteroscopic lithotripsy in treatment of upper-ureteral calculi sized ≥1.5 cm. Beijing Da Xue Xue Bao Yi Xue Ban 2015;47:170-4. [PubMed]
- Chung HS, Jung SI, Yu HS, et al. Modified totally tubeless percutaneous nephrolithotomy: Is it an effective and safe treatment option for renal and upper ureteral stones. Wideochir Inne Tech Maloinwazyjne 2016;11:240-6. [Crossref] [PubMed]
- Cui Z, Gao Y, Yang W, et al. Therapeutic effects of visual standard channel combined with F4.8 visual puncture super-mini percutaneous nephrolithotomy on multiple renal calculi. Pak J Med Sci 2018;34:110-4. [Crossref] [PubMed]
(English Language Editor: J. Chapnick)


