Adolescent varicocele: limited indications for treatment during puberty and adolescence
Introduction
There is no doubt about a link between the presence of a varicocele and fertility, but the exact association is unknown. The hypotheses for a possible association are based on studies regarding temperature, volume and growth of the testis and the semen analysis. However, these are only proxies and in the end, it is the chance of paternity rather than size of testis or semen analysis that is the best end-point to judge fertility. The exact etiology of varicocele also remains uncertain, but most hypotheses suggest that it is relates to the anatomy of testicular vascularisation. Anatomical differences between left and right venous return at the level of the testicular vein are used to explain the presence of dilated veins of the plexus pampiniformis mainly on the left side. On the right side, the testicular vein drains straight into the vena cava at a sharp angle. On the left side on the other hand, the testicular vein drains into the left renal vein at an almost 90° angle. This anatomic difference seems to allow varicoceles to develop, primarily on the left side.
The incidence of varicocele is clearly age-dependent. Before the age of 10, less than 1% of boys will present with a varicocele. From then on the incidence increases with age to reach a 15-20% incidence in boys of about 14-15 years old. This 15-20% incidence is comparable to the general adult population (1). However, there is a higher prevalence of varicocele (20-40%) in men who request investigation of fertility problems (2).
Controversial data exist on the effect of varicocele grade on semen quality. Recently, Al-Ali et al. showed that oligozoospermia was present in twice as many patients with grade III varicocele compared to patients with varicocele grade I or II. They also stated that sperm density significantly decreased with increasing grade of varicocele (3). However, Diamond et al. and Shiraishi et al. reported no significant difference between varicocele grade and semen quality (4,5).
The correct diagnosis of a varicocele
The diagnosis of varicocele is made while examining the patient in standing and supine positions and is generally categorized into three grades according to Dubin and Amlar. The Dubin and Amlar criteria are: grade I, not visible in supine position, palpable only with a Valsalva maneuver in a standing position; grade II, not visible in supine position, palpable in the standing position without a Valsalva maneuver; grade III, visible through the scrotum in the standing position without a Valsalva maneuver. The diagnosis and categorization is subjective. In a study by Hargreave et al., two researchers independently examined the same patients and found a prevalence of varicocele of 19% and 31%, respectively (6). Agreement in the diagnosis occurred in only 56% of patients. Therefore an important point to remember in reviewing the literature is that the incidence/prevalence of varicocele is affected by the examiner’s bias. Men attending infertility clinics undergo a more extensive physical examination and special attention is given to the presence of a varicocele. It becomes obvious that in infertile men, small grade varicoceles will be recorded, whereas in the general population, which usually acts as the control group, it likely will not be.
The importance of the diagnosis of testis volume and growth
In managing patients with a varicocele, the testis volume is important as it has been shown in some studies to correlate with semen quality. The testis volume determination on physical examination is invariably subjective and also very examiner-dependent. As semen parameters are not measurable in most adolescents with a varicocele, the effect of a varicocele on testicular size and the correlation between size and semen quality is very important. Because of the normal variability, it is accepted from previous studies that a 10% size variance between testes without associated abnormalities such as presence of a varicocele is to be considered as normal (7). Diamond et al. showed that a sonographically derived volume differential greater than 10% between normal and affected testes in Tanner V adolescents with varicoceles, correlates with a significantly decreased sperm concentration and total motile sperm count (5). Skoog et al. have pointed out that the growth of the testis is more important than the volume on itself. In his study, it was stated that the loss of testicular volume is accompanied by a decrease in the sperm count and the authors advocate for the early diagnosis of the disease as this is important for the prevention of sperm impairment and infertility (8). Although testicular volume is a measurable parameter in teens (in comparison with semen analysis), there is some controversy on how to measure it. Most recommend that this be evaluated by ultrasound (9).
Will screening and treatment in pubertal boys change their ultimate paternity chance later in life?
To our knowledge, Belgium is the only country worldwide where the diagnosis of a varicocele is included in the medical screening of high school—secondary school boys between 12-18 yrs of age. Since 1987, all children that are found by a school doctor to have a varicocele have received an information flyer concentrating on the fertility issues linked to varicocele. The flyer urges the parents to seek advice and treatment for their sons’ varicocele. Unfortunately this screening was not systematically documented (nor was the follow-up of these patients).
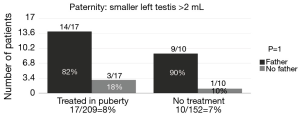
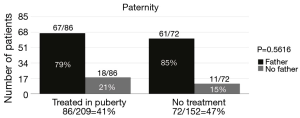
As the screening began in 1987, a significant number of patients have reached the age of 30 years, and many desired to have children. Hence, this provides an opportunity for long-term evaluation of fertility. When we saw these patients, our local policy was to inform the patient and his parents of the options and have them choose whether they to have a treatment for the varicocele or not. The treatment for varicocele that was offered was a scrotal antegrade sclerotherapy of the plexus pampiniformis (10,11). Antegrade sclerotherapy is an efficient minimally invasive surgical method for correcting varicoceles also in adolescents (12). Pintus et al. compared the different treatment modalities for varicocele and concluded that sclerotherapy was as efficient as the other treatment options with less complications (13). In our study, all patients diagnosed with a grade II or grade III varicocele during puberty, and who were now older than 30 years of age, were contacted and asked if they had attempted to have children and if they had successfully become fathers, regardless of whether they had undergone varicocele treatment. The complete data are reported elsewhere (14). Effective paternity was 85% (61/72) in the non-repaired group and 79% (67/86) in the treatment group (P>0.05) (Figure 1). In a sub-analysis of the patients with a smaller left testis preoperatively, a paternity rate of 82% (14 of 17 patients) was found in the treated group and 90% (9 of 10 patients) in those not repaired (P=1) (Figure 2). In addition, the incidence of subfertility as a couple was compared and again there was no difference between the two groups: 16 of 75 couples (21%) in the treated group and 6 of 55 couples (11%) in the untreated group were sub-fertile (P=0.16). In this subgroup, we also looked at men with a smaller left testis preoperatively and found that 4 of 17 couples (23%) in the treated group and 2 of 10 couples (20%) in the conservative group were considered to be sub-fertile (P=0.6).
Conclusions
It is clear that the absolute majority of adolescents with a varicocele will have no fertility problems and a normal paternity potential (14). As a result, our data suggest that systematic screening and treatment during puberty has no beneficial effect on the chance of paternity. Though supportive data are limited, it seems reasonable to follow adolescent boys who have a varicocele and either a smaller left testis or bilateral small testes. If the testis size remains small and/or the volume difference between left and right testis persists or increases, a varicocelectomy can be offered. Better, once these patients are 18 years old a semen analysis will help guide treatment. Overall, there are no clear accepted criteria for varicocelectomy during puberty and our data suggests that the indications are very limited.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Pfeiffer D, Berger J, Schoop C, et al. A Doppler-based study on the prevalence of varicocele in German children and adolescents. Andrologia 2006;38:13-9. [PubMed]
- The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. World Health Organization. Fertil Steril 1992;57:1289-93. [PubMed]
- Al-Ali BM, Marszalek M, Shamloul R, et al. Clinical parameters and semen analysis in 716 Austrian patients with varicocele. Urology 2010;75:1069-73. [PubMed]
- Shiraishi K, Takihara H, Matsuyama H. Elevated scrotal temperature, but not varicocele grade, reflects testicular oxidative stress-mediated apoptosis. World J Urol 2010;28:359-64. [PubMed]
- Diamond DA, Zurakowski D, Bauer SB, et al. Relationship of varicocele grade and testicular hypotrophy to semen parameters in adolescents. J Urol 2007;178:1584-8. [PubMed]
- Hargreave TB, Liakatas J. Physical examination for varicocele. Br J Urol 1991;67:328. [PubMed]
- Zachmann M, Prader A, Kind HP, et al. Testicular volume during adolescence. Cross-sectional and longitudinal studies. Helv Paediatr Acta 1974;29:61-72. [PubMed]
- Skoog SJ, Roberts KP, Goldstein M, et al. The adolescent varicocele: what's new with an old problem in young patients? Pediatrics 1997;100:112-21. [PubMed]
- Cimador M, Castagnetti M, Gattuccio I, et al. The hemodynamic approach to evaluating adolescent varicocele. Nat Rev Urol 2012;9:247-57. [PubMed]
- Tauber R, Johnsen N. Urologe A 1993;32:320-6. [Antegrade scrotal sclerotherapy for treatment of testicular varicocele. Technique and late results]. [PubMed]
- Tauber R, Pfeiffer D. Surgical atlas varicocele: Antegrade scrotal sclerotherapy. BJU Int 2006;98:1333-44. [PubMed]
- Zaupa P, Mayr J, Höllwarth ME. Antegrade scrotal sclerotherapy for treating primary varicocele in children. BJU Int 2006;97:809-12. [PubMed]
- Pintus C, Rodriguez Matas MJ, Manzoni C, et al. Varicocele in pediatric patients: comparative assessment of different therapeutic approaches. Urology 2001;57:154-7. [PubMed]
- Bogaert G, Orye C, De Win G. Pubertal screening and treatment for varicocele do not improve chance of paternity as adult. J Urol 2013;189:2298-303. [PubMed]


