
A systematic review of decision aids for gender affirming therapy
Introduction
While on their journey to gender congruence, transgender and gender diverse (TGD) persons are often faced with many complex hormonal and surgical medical decisions (1-3). Decisions throughout the gender affirmation process are potentially made more complex by a variety of factors. These include a lack of access to medical resources (4), the decreasing age of individuals seeking procedures (5), the high prevalence of co-morbidities in gender diverse populations (6), the unknown long-term outcomes of hormonal and high-risk surgical interventions, the lack of provider understanding (7), and, in the case of the US, not all gender affirming therapies are available in each state, and variation exists regarding insurance coverage for various options (8). For the purposes of this review, gender affirming therapies refers to the broad range of options (both surgical and hormonal) that are available to TGD persons.
For example, adolescents and young adults experiencing gender dysphoria would have to consider the long-term developmental, psychological, urinary and sexual function, and fertility implications of hormonal and surgical therapy (9). The long-term risks extend beyond the immediate or short-term physical impact. Each procedure, performed at different stages over time, carries functional and subsequent emotional risks, which have not been clearly defined by medical experts (10). In the US, the out-of-pocket fees can be substantial depending on where the individual is seeking care, and their insurance coverage. For example, a recent study showed that fewer insurance policies cover feminizing breast surgery in comparison to masculinizing chest surgery. Further, not all insurers cover nipple reconstruction procedures for those who choose masculinizing chest surgery (11).
Given the early stage of research in this field, many clinicians are not yet aware of the relevant trans-related health issues that need to be considered (4,12-14). The median reported time dedicated to teaching trans-related content in 132 medical schools across the US and Canada was 5 hours (15). A survey reported that 22% of obstetrics and gynecology (Ob-Gyn) residents felt “competent to provide trans-relevant services” (Bukowski K, 2017, unpublished data). Over 90% of residents desire more training on trans-sensitivity protocols (Bukowski K, 2017, unpublished data), and almost all directors of accredited Ob-Gyn programs seek trans educational interventions to aid their residency programs (16). The knowledge deficit, exacerbated by insufficient training, often contributes to a misinterpretation of preferences when gender affirmation therapy is considered. In these scenarios, decision support using the best available evidence to compare options could help individuals make higher quality decisions.
Given the complex and preference-sensitive nature of decisions around gender affirming therapies, it follows that transgender persons would have a high degree of decisional conflict (17). This may be due to the task of selecting treatment options that may involve immediate and long-term risks (1). A 2015 Transgender Survey highlighted the psychological distress reported by respondents who identify as TGD (18). It follows that this distress may be related, in part, to the uncertainty regarding which gender affirming therapy best aligns with the individual’s preferences.
To address complex medical decision-making in transgender care, researchers have advocated for a healthcare model that engages patients in their care by discussing relevant treatment options and eliciting their preferences. This model can be called shared decision-making (19,20). Shared decision-making can “empower patients to be active in their care” (21) which leads to a mitigation of biases that perpetuate disparities in TGD care (22). The shared decision-making approach improves patient-clinician communication, that in turn fosters a level of trust potentially reducing perceived TGD-related stigma and vulnerability (23,24). Alpert et al. posit that TGD individuals desire a collaborative partnership with their clinicians in the decision-making process (25).
Interventions known as patient decision aids have been developed to facilitate a shared decision-making process (26). These tools present the evidence-based pros and cons of relevant treatment options in a comparative format, so people can make decisions that align with their preferences (26). Their use is associated with a number of positive patient outcomes, some of which include a reduction in decisional conflict and an increase in knowledge, awareness of options, and shared decision making (27,28). Considering the limited knowledge on TGD-related care, the lack of informed patient-clinician communication, and the power dynamic that exists within clinical encounters that compounds feelings of vulnerability for a stigmatized population, patient decision aids may be able to narrow these gaps. It is unclear what tools, if any, are available to help in TGD medical decision-making.
The purpose of this study is to: (I) search for and determine the quality of any existing patient decision aids developed for people experiencing gender dysphoria or considering gender affirming treatment options; and (II) the outcomes associated with their use. We present the following article in accordance with the PRISMA checklist (29). Available at: http://dx.doi.org/10.21037/tau-20-1000.
Methods
We conducted a systematic review to identify studies that describe the development or evaluation of patient decision aids, and an online search of Google and relevant conferences to find any tools that have not been published in the academic literature. The protocol of our systematic review was published at Open Science Framework (30).
Inclusion criteria
For inclusion in our systematic review to identify studies that detail the development or evaluation of a patient decision aid for gender dysphoria or gender affirming treatment options, we used the population, intervention, control, outcomes, study design (PICOS) method (31). Our population of interest was persons experiencing gender dysphoria due to “distress resulting from a marked incongruence between the assigned gender and experienced gender” (32) or self-identify as TGD because their gender identity does not correspond with their phenotypic sex (33). We did not include persons with differences of sex development for whom chromosomal, gonadal, or anatomic sex development is atypical or ambiguous and have to decide on genital surgery (34). For our intervention, we employed the Stacey et al. definition of a patient decision aid to include “evidence-based tools designed to help patients make specific and deliberated choices among healthcare options. In general, they explicitly state the decision being considered, provide evidence-based information about the health condition, the management options and associated benefits and harms, and help patients to recognize the values-sensitive nature of the decision and to clarify their values” (27). A control group was not required, but in the case of a randomized trial, the comparator would be usual care, the absence of a patient decision aid, or another type of decision support intervention (i.e., pamphlet, booklet, leaflet). We included all primary or secondary outcomes and we included any type of study design.
We applied the same population and intervention criteria to our brief online search of Google and relevant conferences to find patient decision aids for gender dysphoria or gender affirming treatment options that have not been published in the academic literature.
Data sources and search strategy
To search for published studies of gender dysphoria or gender affirming treatment patient decision aids, two information scientists (PJ Bagley and HB Blunt) developed and adapted an electronic search strategy for each of the following databases: Medline, CINAHL, Web of Science, Cochrane, EMBASE, and PsycINFO. The search was performed on February 12, 2020. Two key concepts—decision support intervention/patient decision aid and transgender—informed our keywords and medical subject headings (MeSH) terms. See Figure S1 for the search strategy used for each database. We did not impose any restrictions on language or date of publication.
To identify tools that have been developed but not published in the academic literature, we searched relevant conferences such as International Shared Decision Making, Society for Medical Decision Making, and the International Conference on Communication in Healthcare. We also used a combination of terms in the Google search engine such as “transgender patient decision aid”, “transgender decision support”, “transgender shared decision making”, “transgender patient-centered care” and reviewed the first 50 hits for each search to identify any tools or studies that met our inclusion criteria.
Study and patient decision aid selection
Two researchers (P Scalia and KM Tighe) reviewed the titles and abstracts of all articles and identified the studies that required full-text review based on our inclusion criteria. The same two researchers independently reviewed the full-text and came to consensus on the final list of included studies. Studies chosen for full-text review were also screened by a reconstructive urologist who provides TGD care (RA Moses). The same two researchers met to review the abstracts published by the relevant conferences and the Google links that were identified using the combination of search terms outlined in the “data sources and search strategy” section.
Data extraction
We extracted the following data from included studies: author, publication date, country where the study was conducted, study design, setting, sample size and characteristics (i.e., age, sex), mode of delivery and format of the patient decision aid and the options presented, and any primary and secondary outcomes associated with the intervention. For any tools found in the Google or conference search, we extracted the format and the therapy options presented.
Analysis
To assess the quality of the patient decision aid and the reporting of evaluations of the tool, two researchers independently used two checklists. The 44-item International Patient Decision Aid Standards instrument (IPDASi) criteria were used to assess the quality of the decision aid, and we recorded the presence or absence of each item on the qualifying criteria of the checklist with a score of 1 (present) or 0 (absent) (35). Each certification and quality criteria of IPDASi were rated on a Likert scale of 1 (strongly disagree) to 4 (strongly agree) (35). For studies reporting an evaluation of a relevant patient decision aid we used the 26-item Standards for UNiversal reporting of patient Decision Aid Evaluations (SUNDAE) checklist to assess the quality of the reporting (36). Any disagreements with ratings were resolved by a third researcher, G Elwyn. We narratively synthesized any outcomes associated with the included patient decision aid(s).
Results
Study characteristics
A total of 762 studies were identified in our systematic review. Our brief online search of Google and relevant conferences did yield educational resources for persons seeking gender affirming treatment, but none met the definition of a patient decision aid. After reviewing the study titles and abstracts we excluded 749 studies. Full-text review was conducted for 13 studies and we determined that only one study met our inclusion criteria (see Figure 1 for details).
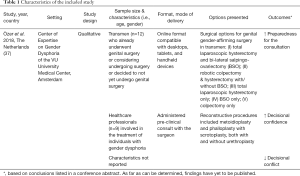
Özer et al. developed an online, pre-encounter patient decision aid for transmasculine genital gender-affirming surgery (GAS) for individuals assigned female at birth (37). The decision aid was developed in the Netherlands through a series of focus groups with healthcare professionals and transgender men at the Center of Expertise on Gender Dysphoria in Amsterdam. Transgender men had either previously undergone transmasculine genital surgery, were considering the surgery, or remained undecided. The tool is available in Dutch and English and provides general information on the following treatment options: (I) total laparoscopic hysterectomy and bi-lateral salpingo-ovariectomy (BSO); (II) robotic colpectomy & hysterectomy with/without BSO; (III) total laparoscopic hysterectomy only; (IV) BSO only; (V) colpectomy only. Reconstructive procedures included metoidioplasty and phalloplasty with scrotoplasty, both with and without urethroplasty. Numerical risk data was omitted from the patient decision aid due to the lack of quality, reliable evidence. The patient decision aid is available at https://keuzehulp-operaties-transmannen.nl/en (see Table 1 for details).
Full table
Quality of the decision aid(s)
The tool for GAS for transgender men met all six qualifying IPDASi criteria to be considered a patient decision aid. Of the ten certification criteria, three were not applicable. The absence of citations for the selected evidence, production or publication date, and information on the evidence update policy led to a combined score of 17/28 for the remaining seven certification criteria. For the quality criteria, raters provided a score of 57/112 (5 criteria were not applicable). The lack of outcome probabilities in the patient decision aid impacted the quality criteria score (see Table S1 for details).
Outcomes associated with the decision aid(s)
As far as can be determined, the outcomes associated with the genital GAS decision aid for transgender men have not yet been published. Due to the absence of published evaluations of this decision aid, the SUNDAE checklist was not applicable. However, a recent conference abstract indicates that this tool “helped transgender men feel more prepared for the consult, reduced decisional conflict and increased decisional confidence” (Mokken S, 2019, unpublished data).
Discussion
Only one intervention that meets the criteria of a patient decision aid has been published in the literature, and although it scores well against the quality standards, it has not yet been evaluated in the context of a study or randomized trial. The patient decision aid for GAS for transgender men provides evidence-based information on five surgical and two reconstructive procedures. The developers of the tool were unable to quantify the long-term risks associated with each procedure for transgender men, but pros and cons were presented for five domains: treatment and result, quality of life, social environment, sexuality, and belief. Although evidence from a formal evaluation has not yet been published, a conference abstract reported that the patient decision aid for GAS for transgender men increased confidence and preparedness for a clinical conversation while reducing decisional conflict.
The strengths of our systematic review include: the following of best practice and the PRISMA reporting guidelines, the collaboration of information scientists (PJ Bagley and HB Blunt), patient decision aid experts and a reconstructive urologist (RA Moses) who provides TGD surgical care to develop and adapt a comprehensive search strategy, searching Google and relevant conferences to identify tools that have not been published in the academic literature, and the use of two independent raters to determine the quality of the tool using the iPDASi criteria. In regard to limitations of our review, many studies do not provide sufficient details on the patient decision aid. Thus, it challenging to determine patient decision aid eligibility for inclusion in our systematic review. Second, it is possible that we did not capture all the possible search terms for the concept of “decision aids”. The lack of description to enable us to determine patient decision aid eligibility and the possibility that the list of search terms for the decision aid concept was not comprehensive makes it possible that we omitted some studies that otherwise would meet our inclusion criteria.
For decision support interventions (i.e., booklets, pamphlets, brochures) that have been developed, whether they be paper-based or online, a high level of health literacy is required to understand the content, and their quality is heterogeneous (38). The recommended reading level for patient materials is sixth grade, yet according to readability analyses, the average reading level for websites providing online gender affirmation surgery information is eleventh grade (39). Vargas et al. confirmed the high readability level required for websites providing transgender therapy information and determined that six of the ten online resources for GAS identified in their search are of low quality (40). A recent 2017 systematic review also found that the “quality of patient information on phalloplasty in the Internet is substandard” (41). Paper-based booklets that provide pelvic radiotherapy information to TGD persons are also considered to contain incorrect language and assumptions about the TGD community which could cause distress (42).
Furthermore, a key element of decision aids is the provision of risk information, so the absence of long-term psychological and physical outcomes for hormonal and surgical interventions for TGD in the medical literature has implications for potential developers and users of these tools (1-3). For instance, Özer et al. cited insufficient evidence for not including numerical data on outcomes in the transmasculine genital GAS decision aid (37). However, in the absence of reliable data, a quality patient decision aid should state that insufficient evidence exists, and that more research is needed. The lack of long-term risk information makes it challenging for clinicians to counsel adolescents, young adults and their families. Qualitative work indicates that although teens have short-term concerns related to their treatment, their parents seek information on the long-term risks of decisions (1). Without tailored decision tools to support teens and young adults with unique developmental needs there is potential for post-operative regret (43). A small percentage (ranging from 0 to 6%) of TGD individuals experience regret due to poor surgical outcomes or complications (Cartwright T, 2017, unpublished data).
Patient decision aids may help TGD persons understand the risks involved for each gender affirming therapy, so they can make informed decisions. Although decision support can occur in the absence of a patient decision aid, these tools can facilitate better communication with clinicians by providing the most current, evidence-based information, so that TGD persons can share their goals and concerns to help avoid decisional regret. To date, it is unknown if any clinics that treat TGD persons during their gender affirming journey use patient decision aids. Although some decision support interventions are emerging, such as a pre-surgery “counseling aid” for transgender women to decide on their preferred type of vaginoplasty (44), and “surgery readiness class” to prepare TGD persons for gender affirming surgeries (45), our review highlights the need to develop high-quality, culturally sensitive and developmentally targeted tools that address the key decisional topics and their associated risk. Future research should focus on the development and implementation of patient decision aids to engage TGD persons in their care and help them understand the longer-term implications (i.e., physical, mental, emotional) of choosing the various gender affirming therapies to improve the quality of decision-making.
Acknowledgments
We would like to thank Dr. Ella A. Damiano, Dr. John F. Nigriny, and Dr. Stuart W. Grande for reviewing the final draft of the manuscript prior to submission.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Francisco E. Martins and Tobias S. Köhler) for the series “Controversies and Considerations of Penile Surgery” published in Translational Andrology and Urology. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at: http://dx.doi.org/10.21037/tau-20-1000
Peer Review File: Available at http://dx.doi.org/10.21037/tau-20-1000
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-20-1000). The series “Controversies and Considerations of Penile Surgery” was commissioned by the editorial office without any funding or sponsorship. GE has edited and published books that provide royalties on sales by the publishers: the books include Shared Decision Making (Oxford University Press) and Groups (Radcliffe Press). He has in the past provided consultancy for organizations including (I) Emmi Solutions LLC who developed patient decision support tools; (II) National Quality Forum on the certification of decision support tools; (III) Washington State Health Department on the certification of decision support tools; (IV) SCiMentu LLC, Amsterdam (workshops for shared decision making). He is the Founder and Director of &think LLC which owns the registered trademark for Option Grids TM patient decision aids. Founder and director of SHARPNetwork LLC, a provider of training for shared decision making. He provides advice in the domain of shared decision making and patient decision aids to (I) Access Community Health Network, Chicago Federally Qualified Medical Centers); (II) EBSCO Health Option Grids TM patient decision aids; (III) Bind Insurance; (IV) PatientWisdom Inc; (V) abridge AI Inc. GE’s academic interests are focused on shared decision making and coproduction. He owns copyright in measures of shared decision making and care integration namely collaboRATE, integRATE, consideRATE, coopeRATE, toleRATE, Observer OPTION-5 and Observer OPTION-12. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Daley T, Grossoehme D, McGuire JK, et al. “I couldn’t see a downside”: decision-making about gender-affirming therapy. J Adolesc Health 2019;65:274-9. [Crossref] [PubMed]
- Kimberly LL, Folkers KM, Friesen P, et al. Ethical Issues in Gender-Affirming Care for Youth. Pediatrics 2018;142:e20181537 [Crossref] [PubMed]
- Leibowitz SF, Lantos JD. Affirming, Balanced, and Comprehensive Care for Transgender Teenagers. Pediatrics 2019;143:e20190995 [Crossref] [PubMed]
- Lerner JE, Robles G. Perceived Barriers and Facilitators to Health Care Utilization in the United States for Transgender People: A Review of Recent Literature. J Health Care Poor Underserved 2017;28:127-52. [Crossref] [PubMed]
- Zucker KJ. Epidemiology of gender dysphoria and transgender identity. Sexual Health 2017;14:404-11. [Crossref] [PubMed]
- Downing JM, Przedworski JM. Health of transgender adults in the U.S., 2014-2016. Am J Prev Med 2018;55:336-44. [Crossref] [PubMed]
- Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med 2013;84:22-9. [Crossref] [PubMed]
- Learmonth C, Viloria R, Lambert C, et al. Barriers to insurance coverage for transgender patients. Am J Obstet Gynecol 2018;219:272.e1-272.e4. [Crossref] [PubMed]
- Chen D, Kyweluk MA, Sajwani A, et al. Factors affecting fertility decision-making among transgender adolescents and young adults. LGBT Health 2019;6:107-15. [Crossref] [PubMed]
- Frey JD, Poudrier G, Chiodo MV, et al. Research Disparities in Female-to-Male Transgender Genital Reconstruction: The Charge for High-Quality Data on Patient Reported Outcome Measures. Ann Plast Surg 2017;78:241. [Crossref] [PubMed]
- Ngaage LM, Knighton BJ, McGlone KL, et al. Health Insurance Coverage of Gender-Affirming Top Surgery in the United States. Plast Reconstr Surg 2019;144:824-33. [Crossref] [PubMed]
- Khalili J, Leung LB, Diamant AL. Finding the perfect doctor: identifying lesbian, gay, bisexual, and transgender-competent physicians. Am J Public Health 2015;105:1114-9. [Crossref] [PubMed]
- Knight RE, Shoveller JA, Carson AM, et al. Examining clinicians’ experiences providing sexual health services for LGBTQ youth: considering social and structural determinants of health in clinical practice. Health Educ Res 2014;29:662-70. [Crossref] [PubMed]
- Ziegler E, Valaitis R, Yost J, et al. “Primary care is primary care”: use of Normalization Process Theory to explore the implementation of primary care services for transgender individuals in Ontario. PLoS One 2019;14:e0215873 [Crossref] [PubMed]
- Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender–related content in undergraduate medical education. JAMA 2011;306:971-7. [Crossref] [PubMed]
- Grimstad FW, Satterwhite CL, Wieneke CL. Assessing residency program approaches to the transgender health CREOG objective. Transgend Health 2016;1:69-74. [Crossref] [PubMed]
- Jokić-Begić N, Lauri Korajlija A, Jurin T. Psychosocial adjustment to sex reassignment surgery: a qualitative examination and personal experiences of six transsexual persons in croatia. ScientificWorldJournal 2014;2014:960745 [Crossref] [PubMed]
- Herman JL, Wilson BD, Becker T. Demographic and Health Characteristics of Transgender Adults in California: Findings from the 2015-2016 California Health Interview Survey. Policy Brief UCLA Cent Health Policy Res 2017;1-10. [PubMed]
- Baig AA, Lopez FY, DeMeester RH, et al. Addressing barriers to shared decision making among Latino LGBTQ patients and healthcare providers in clinical settings. LGBT Health 2016;3:335-41. [Crossref] [PubMed]
- Peek ME, Lopez FY, Williams HS, et al. Development of a conceptual framework for understanding shared decision making among African-American LGBT patients and their clinicians. J Gen Intern Med 2016;31:677-87. [Crossref] [PubMed]
- Chin MH, Lopez FY, Nathan AG, et al. Improving shared decision making with LGBT racial and ethnic minority patients. J Gen Intern Med 2016;31:591-3. [Crossref] [PubMed]
- Foglia MB, Frederiksen-Goldsen KI. Health disparities among LGBT older adults and the role of nonconscious bias. Hastings Cent Rep 2014;44:S40-4. [Crossref] [PubMed]
- von Vogelsang AC, Milton C, Ericsson I, et al. ‘Wouldn’t it be easier if you continued to be a guy?’ - a qualitative interview study of transsexual persons’ experiences of encounters with healthcare professionals. J Clin Nurs 2016;25:3577-88. [Crossref] [PubMed]
- Redfern JS, Sinclair B. Improving health care encounters and communication with transgender patients. J Commun Healthc 2014;7:25-40. [Crossref]
- Alpert AB, Cichoskikelly EE, Fox AD. What lesbian, gay, bisexual, transgender, queer and intersex patients say doctors should know and do: a qualitative study. J Homosex 2017;64:1368-89. [Crossref] [PubMed]
- Elwyn G, Lloyd A, Joseph-Williams N, et al. Option Grids: shared decision making made easier. Patient Educ Couns 2013;90:207-12. [Crossref] [PubMed]
- Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4:CD001431 [Crossref] [PubMed]
- Scalia P, Durand MA, Berkowitz JL, et al. The impact and utility of encounter patient decision aids: systematic review, meta-analysis and narrative synthesis. Patient Educ Couns 2019;102:817-41. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [Crossref] [PubMed]
- Scalia P. A systematic review of decision aids for gender confirming therapy. Open Science Framework 2020. Available online: https://osf.io/gmvhs
- Methley AM, Campbell S, Chew-Graham C, et al. PICO, PICOS, and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014;14:579. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publisher, 2013.
- van de Grift TC, Elfering L, Bouman MB, et al. Surgical Indications and Outcomes of Mastectomy in Transmen: A Prospective Study of Technical and Self-Reported Measures. Plast Reconstr Surg 2017;140:415e-424e. [Crossref] [PubMed]
- Witchel SF. Disorders of sex development. Best Pract Res Clin Obstet Gynaecol 2018;48:90-102. [Crossref] [PubMed]
- Joseph-Williams N, Newcombe R, Politi M, et al. Toward minimum standards for certifying patient decision aids: a modified delphi consensus process. Med Decis Making 2014;34:699-710. [Crossref] [PubMed]
- Sepucha KR, Abhyankar P, Hoffman AS, et al. Standards for UNiversal reporting of patient Decision Aid Evaluation studies: the development of SUNDAE checklist. BMJ Qual Saf 2018;27:380-8. [Crossref] [PubMed]
- Özer M, Pigot GLS, Bouman MB, et al. Development of a Decision Aid for Genital Gender-Affirming Surgery in Transmen. J Sex Med 2018;15:1041-8. [Crossref] [PubMed]
- Kiwanuka E, Mehrzad R, Prsic A, et al. Online patient resources for gender affirmation surgery: an analysis of readability. Ann Plast Surg 2017;79:329-33. [Crossref] [PubMed]
- Cook JA, Sasor SE, Deldar R, et al. Complexity of online gender confirmation resources surpass patient literacy. Int J Transgend 2017;18:367-71. [Crossref]
- Vargas CR, Ricci JA, Lee M, et al. The accessibility, readability, and quality of online resources for gender affirming surgery. J Surg Res 2017;217:198-206. [Crossref] [PubMed]
- Karamitros GA, Kitsos NA, Sapountzis S. Systematic review of quality patient information on phalloplasty in the internet. Aesthetic Plast Surg 2017;41:1426-34. [Crossref] [PubMed]
- Burton H, Pilkington P, Bridge P. Evaluating the perceptions of the transgender and non-binary communities of pelvic radiotherapy side effect information booklets. Radiography 2020;26:122-6. [Crossref] [PubMed]
- Karpel L, Cordier B. Postoperative regrets after sex reassignment surgery: a case report. Sexologies 2013;22:e55-8. [Crossref]
- Garcia MM. Sexual Function After Shallow and Full-Depth Vaginoplasty: Challenges, Clinical Findings, and Treatment Strategies—Urologic Perspectives. Clin Plast Surg 2018;45:437-46. [Crossref] [PubMed]
- Poceta J, Cousins S, Wenzel C, et al. Effectiveness of a gender affirming surgery class for transgender and non-binary patients and their caregivers in an integrated healthcare setting. Int J Transgend 2019;20:81-6. [Crossref] [PubMed]



