Advances in ureteroscopy
Introduction
Ureteroscopy (URS) is a well-established diagnostic and therapeutic modality in urological practice. Advances in technology and surgical techniques have broadened the range of urologic conditions that can be addressed by URS including: renal and ureteric calculi, urothelial carcinoma (UC) and ureteral strictures. The use of URS for the treatment of stones is increasing relative to shockwave lithotripsy (SWL) (1). In this article we aim to summarise the pertinent developments in the field of URS.
Discussion
Ureteroscopes can be classified as rigid, semi-rigid, or flexible. Rigid ureteroscopes use a non-flexible optical lens system. The most significant advance in the field of endourology is the recent development of flexible ureteroscopes. These scopes are smaller than their rigid and semi-rigid counterparts and have increased capability for deflection and instrumentation. Semi-rigid ureteroscopes are usually housed in a pliable metallic sheath, whereas flexible ureteroscopes do not have a rigid outer layer. This manoeuvrability allows instrumentation of the entire urinary tract including upper ureters and pelvic calyxes. Development of instrumentation has included the addition of working channels, narrower shaft diameters, greater distal tip active deflection and secondary deflection (2).
Flexible ureteroscopes
Fibre-optic flexible ureteroscopes were primarily developed due to concerns with the rigid ureteroscope causing damage to the urothelium when accessing the upper ureter.
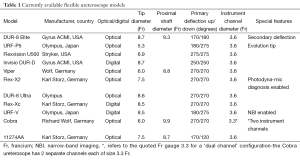
The deflection capacity (flexion of the tip from a straight to an angled position) in digital ureteroscopes varies in each model (Table 1). Primary deflection is the initial degree of deflection achieved from a neutral straight position of the scope tip, whereby secondary deflection is a further degree of deflection in relation to an already curved or ‘flexed’ ureteroscope tip. Secondary deflection is necessary in up to 29% of cases, particular lower pole calculi (3). The DUR®-8 Elite ureteroscope (Gyrus ACMI, USA) is the only model that offers secondary deflection. Secondary deflection of 130° up or down allows the surgeon to achieve a total deflection angle up to 270° (4). The wide range of deflection capabilities and ‘S’ shape allows an experienced urologist to access virtually any area of the intrarenal collecting system (5).
Full table
Other ureteroscope advances include a laser-resistant chip composed of a proprietary LaseriteTM (5), minimization of distal tip [<6 francium (Fr)] and a tapered ‘evolution’ tip to facilitate ureteral cannulation, as seen in the Olympus URF-P5 flexible ureteroscope (Olympus, USA). Some limitations of fibre-optic based ureteroscopes include: damage to optic fibres leading to reduced image quality, overall ‘grainy’ picture and potential water infiltration onto optical lens.
Digital imaging
The recent development of digital ureteroscopic imaging has led to higher quality ureteric and renal pelvis imaging compared to traditional fibre-optic ureteroscopes (4). Digital ureteroscopes transmit images from a digital sensor on the tip to a proximal point via a single wire, with processing occurring at a proximal sensor. This new generation of “chip on the tip” digital ureteroscopes avoid the use of fibre-optics for the transmission of images. Light can be provided from a distal LED source or transmitted via the scope from a proximal source. Digital ureteroscopes offer high-definition imaging, autofocus capabilities and digital magnification. As a result the moiré (honeycomb) effect is eliminated with digital scopes, overall improved image quality and up to 2.5 times larger image on a standard monitor compared to fibre-optic ureteroscopes (6). Digital video URS eliminates the need to attach a camera allowing for less cables, quicker set-up and less weight, which is advantageous in long cases (5).
The first digital ureteroscope was the Invisio® DUR®-D (Olympus) which was introduced in 2006. All digital ureteroscopes currently available are summarised in Table 1. Although the new digital technology is more expensive than the traditional fibre-optics, they have been reported to be more durable and require less frequent repairs (7). In addition, the elimination of the need for fibre-optics allows for larger working channels in these new digital ureteroscopes (8). However, these all-in-one digital scopes are often larger than fibre-optic scopes (9). A randomised control trial (RCT) by Bach et al. (10) compared the Invisio® DUR®-D (Gyrus ACMI, USA) digital scope to the DUR®-8 Elite (Gyrus ACMI, USA) fibre-optic flexible ureteroscope and the use of ureteral access sheaths. The use of ureteral access sheaths was significantly higher (P<0.005) for the digital scope DUR®-D (25%) compared to the fibre-optic DUR®-8 (7.5%). This study quoted differing sizes compared to the manufacturer brochure: 6.75 instead of 8.7 Fr and 8.7 instead of 9.3 Fr for the DUR®-8 and DUR®-D scopes respectively (11).
Shah et al. (12) compared the Invisio® DUR®-D to the URF-V (Olympus, Japan) digital ureteroscope in a prospective RCT. Overall the URF-V scope offered better maneuverability. A smaller fibre-optic ureteroscope was required in 11% and 7% of cases for the URF-V and DUR®-D scopes respectively. Multescu et al. (13) compared the URF-V digital to the Storz 11274AA fibre-optic flexible ureteroscope in 44 diagnostic retrograde procedures. The URF-V digital ureteroscope displayed superior maneuverability, durability and visibility.
Advanced imaging
Endourology has seen a number of technical advances in imaging to aid with the diagnosis of upper tract UC. Conventional white-light imaging is sufficient for the diagnosis of medium to large upper tract UC lesions however, visualising smaller lesions can be difficult. Narrow-band imaging (NBI) and photodynamic diagnosis (PDD) are imaging advances that aid in the diagnosis of upper tract UC.
NBI is an optical image enhancement technique which filters white light into two narrow bandwidths, 415 nm (blue) and 540 nm (green), which are strongly absorbed by haemoglobin. This enhances the contrast between mucosal surfaces and micro-vascular structures in real-time, without the use of dyes (14). In the presence of UC, which is highly vascular in nature, NBI increases the colour contrast between superficial tumours and normal mucosa. Currently the only scope with NBI capability is the URF-V (Olympus, Japan) digital ureteroscope and has been shown to improve tumour detection rates by 23% compared to white-light imaging (15).
PDD is an optical enhancement for URS utilising fluorescence, which enhances the contrast between benign and malignant tissue The urinary tract tissues is photosensitised by the administration of an agent either delta-aminolevulinic acid (ALA) or its derivative, hexaminolevulinate (HAL, Hexvix). These prodrugs initiate a series of biochemical reactions that results in an end-product (photoactive porphyrins) that accumulates and emits red fluorescence (693 nm) in malignant tissues in the presence of blue light (380-470 nm) (14,16). Normal bladder mucosa appears blue-green allowing the surgeon to identify potentially malignant tissue. A prospective pilot study for detecting upper tract UC using PDD and the administration oral 5-ALA supported it as a feasible and useful technique with additional advantages of detecting lesions not seen on conventional white-light URS (17).
Guidewires and ureteral access sheaths
Alongside a wide variety of endoscopic instruments that have been introduced to treat renal stones, there are many different guidewires commercially available. In essence the guidewire remains a useful tool in navigating past an impacted calculus and maintaining a “safety-line” to the renal pelvis during URS. Despite debate about the necessity of this safety technique (18,19) the general consensus is that a safety guidewire should be still used in all cases (8).
There are many different guidewires with differing properties that gives each one their own unique advantages. The Glidewire® by Boston Scientific (USA) aka a ‘slippery’ guidewire is extremely flexible and therefore relatively atraumatic but often has a tendency to bend if faced with an obstruction (9). The Amplatz Super Stiff™ guidewire (Boston Scientific, USA) is more resistant to bending and can be used to pass instruments successfully (20).
A development in this field is the introduction and adoption of hybrid guidewires that offer both the flexibility of a hydrophilic wire at the tip and a stiff body to maintain rigidity (9). Two examples of hybrid wires currently on the market include the Sensor™ (Boston Scientific, USA) and U-Nite™ (Bard Medical, USA) wires. A systematic evaluation by Sarkissian and colleagues (21) concluded that the Sensor™ wire has a greater friction force and should be the choice for a safety wire amongst hybrid wires. The hydrophilic tip of the Sensor™ wire is more flexible compared to the U-Nite™ and is likely a better choice for bypassing an obstructing ureteric calculus. The rounder tip of the U-Nite™ wire is less likely to cause ureteral mucosal tunnelling (9).
The use of ureteral access sheaths in URS allow for lower irrigation pressures and therefore reduced ureter rupture risk, reduced operating time and improved scope longevity (22). Digital ureteroscopes often require the use of a ureteric access sheath. Ng et al. (23) found that the size of ureteric access sheaths (10 to 16 Fr) had minimal impact on irrigation flow whilst the working channel was occupied. They also demonstrated that better flow dynamics could be achieved by using a concurrent ureteral access catheter (4 or 5 Fr) alongside a normal ureteral access sheath purely for irrigation inflow.
Two studies favour the 12/14 Fr Cook Flexor® access sheath (Cook Urological, USA) with regards to placement, instrument passage, stone extraction, a low failure rate and less propensity to buckle whilst in situ (24,25).
Intracorporeal lithotripsy
In current practice lasers are the most popular devices for intracorporeal lithotripsy. Other lithotripters that are available include electrohydraulic (EHL), pneumatic and ultrasonic. The Holmium: yttrium-aluminium-garnet (YAG) is the gold-standard for laser lithotripsy during URS, which is effective against all stone composites and produces smaller fragment sizes (26). This laser energy has superior complication and stone-free rates compared to EHL or pneumatic lithotripsy (9). Results from several studies using the Holmium: YAG laser reported stone-free rates for ureteric stones (upper, mid and distal) ranged from 89-100% and 77-99% in the kidney (27-30). A meta-analysis by Aboumarzouk et al. (31) looked at stones >2 cm treated by flexible URS and laser lithotripsy and this technique was effective for large stones. This technique had a stone-free rate of 96% from stones 2-3 cm and 85% for those >3 cm, with a minor complication rate of 14% and 15% respectively. Major complication rate was 11.5% for stones >3 cm with no major complications for stones 2-3 cm.
Laser lithotripsy requires a laser fibre through a working channel on a rigid or flexible ureteroscope. The size and type (single versus reusable) of fibre can affect deflection capabilities, irrigation flow and potential for scope damage (8). The sizes of laser fibres vary from small (150 to 300 µm) to medium (300 to 400 µm). In general, a smaller fibre is more flexible and less traumatic to scopes, but have more degradation and are slower at defragmenting compared to larger fibres (9). It is estimated that a Holmium: YAG laser fibre of 365 µm can cause a loss in deflection of 24° to 45°, and for a 200 µm fibre this loss is smaller at around 9° to 19° (32). It is generally recommended that a medium to large fibre (≥300 µm) is reserved when using a rigid ureteroscope and during flexible URS a smaller fibre (≤200 µm) is used to preserve scope deflection and therefore access to upper tracts (32,33).
One limitation of lasers is the potential for ureteroscope damage from the introduction of the laser fibre, particularly in a deflected scope, or activation of the laser whilst the tip is within the working channel. There are a few products that aim to prevent scope damage during laser lithotripsy that include: endoscope protection system (EPS) (Gyrus ACMI, USA, Massachusetts), Flexguard™ (Lisa Laser Products, Germany) and the TracTip fibre (Boston Scientific, USA). The EPS is available with the DUR®-D flexible ureteroscope and immediately terminates the Holmium: YAG laser energy upon the fibre being retracted into the ureteroscope (9). This device is successful in vitro but in vivo results of successful laser termination rates range from 50% to 100% (34,35), therefore further studies and evaluation is needed to evaluate the efficacy of EPS. Flexguard™ is a protective laser sheath with mixed results showing that it offers protection to ureteroscopes from laser fibre damage after 40 to 50 uses but led to a loss in deflection capability (36). The TracTip fibre is small (200 µm) and round tipped therefore can be advanced even during scope deflection.
Instruments for stone retrieval
Baskets ideally should be durable, flexible, easily deployed, atraumatic and have low resistance properties in order to preserve adequate irrigation flow during URS. There are several baskets on the market, with the newer, often smaller (<1.5 Fr) nitinol (nickel titanium) baskets replacing stainless steel (9). This new metal alloy allows for increased flexibility and memory, and smaller diameter has less impact on irrigation flow. Current baskets on the market vary in design from the simple Cook NCircle® nitinol basket (Cook Inc. USA) to the more complex configuration such as Sur-Catch (ACMI). Other models include the OptiFlex™ (Boston Scientific, USA) and the Halo™ (Sacred Heart Medical, USA) baskets (37). Ex vivo studies conclude that smaller diameter baskets (<1.5 Fr), such as the OptiFlex™ (1.3 Fr) have less detrimental effect on irrigation flow and ureteroscope deflection (38). Porcine studies have shown no advantage in complex wire configuration in stone retrieval (39). The Escape™ basket (Boston Scientific, USA) is unique in design as it allows the surgeon to grasp and simultaneously laser a stone, with a 200 µm holmium laser fibre transmitted through the inner channel within the basket wiring (9).
Devices to prevent stone migration
During URS, proximal migration of a stone or fragments can be an issue. This is particularly problematic during lithotripsy and is influenced by many factors including irrigation pressure, location of the stone and degree of proximal hydronephrosis. There are numerous specific devices available which aim to prevent this occurrence. In general this technique is recommended after primary lithotripsy has been performed and a stone fragment is too large to be removed via basket (8). In addition, many anti-retropulsion devices have to be deployed alongside the ureteroscope, whilst the working channel is occupied by a lithotripsy fibre (e.g., laser), and therefore can be problematic in a narrow ureter (9).
The Stone Cone™ (Boston Scientific, USA) is made from an inner coiled nitinol wire covered with an outer radio-opaque 3 Fr polytetrafluroethylene cover, which aims to prevent the migration of fragments larger than 2 to 3 mm (8). It is available in two sizes: 7 or 10 mm. Eisner et al. (40) analyzed a case-series of 133 ureteroscopies over 3 years and reported only two patients with stone fragments larger than 2 mm following the use of the Stone Cone™ device. This device is resistant to EHL and pneumatic lithotripsy, however, one limitation is that it can be damaged by the Holmium laser.
The Cook NTrap® device (Cook, USA) is a 2.6 Fr deployable nitinol mesh. In a meta-analysis including 456 patients by Ding et al. (41) they showed a significant advantage in the NTrap® cohort versus controls in terms of stone-free rates (odds ratio OR =3.08, P=0.003). The incidence of stone migration was also significantly lower using the NTrap® (OR =0.23, P=0.0006) but operative time was not prolonged compared to controls (P=0.62). A comparison study by Lee et al. (42) compared the NTrap® and Stone Cone™ in an in vitro model but found no difference between either device. The Accordion® (Percutaneous System, USA) is a 2.9 Fr urethane film ureteral occlusion device, which has also been found to be an effective anti-migration device compared to controls (P=0.0064) (43). Fogarty balloons used for ureteral occlusion during lithotripsy have been found to be ineffective (44).
Recently a temporary ureteral occlusion gel BackStop™ (Boston Scientific, USA) has become available which is thermosensitive and can be dissolved easily by an induced temperature change (45). Rane et al. (46) performed a RCT including 68 patients to evaluate the effectiveness of BackStop™ ureteral occlusion gel and found a significantly reduced rate of retropulsion of stone fragments using the gel compared to control (P=0.0002).
New techniques
Lower pole kidney stones can be difficult to access and treat with URS. Anatomically the lower pole infundibulopelvic angle, which averages 140° (from ureter to lower pole), restricts deflection of flexible ureteroscopes. In addition, the use of a laser fibre within the working channel further impedes scope flexibility. Ghani et al. (47) describe a surgical technique whereby evacuating the collecting system with a syringe can draw the stone closer to the scope and maximise angle of deflection. They also describe a nitinol basket deployment technique whereby a smaller calibre basket is used to reposition the stone into a middle or upper calyx, requiring a smaller degree of scope deflection and a larger laser fibre (e.g., 365 µm) can be used for fragmentation.
Bostanci et al. (48) describe a double wire technique for difficult ureteroscopic access in order to prevent the impact on patient quality of life (QoL) and potential anaesthetic risk from a secondary URS procedure. Anatomical variation, ureteral oedema, muscular spasm or prostatic hyperplasia can distort the vesicoureteric junction. They describe a method using a secondary guidewire through the ureterscope’s working channel, which is inserted into the ureter alongside the safety wire. This facilitates dilatation of the vesicoureteric junction and safe passage of the ureteroscope.
Special considerations
Urolithiasis is the second most common cause of abdominal pain in pregnancy and affects 0.5% of pregnancies, with 80-90% of patients in their 2nd or 3rd trimester (49). Clinical guidelines from the European Association of Urology suggest that URS is reserved for failed conservative management or temporising measures (e.g., JJ uteral stent or nephrostomy) and only performed in specialist centres (50). A systematic review of the literature by Laing et al. (49) analysed 116 URS procedures and reported a complete stone clearance rate of 86%. Clavien complications (grades I to III) occurred in nine patients. The most significant was a ureteral perforation (Clavien III) and premature uterine contraction (Clavien II). URS in pregnancy is an effective and potential first-line treatment for urolithiasis in pregnancy but should be reserved to high volume centres.
Conclusions
Over recent years we have witnessed many advances in URS. The most significant advance is the development of flexible ureteroscopes, which have revolutionised access to the upper urinary tract and therefore the treatment of proximal and intrarenal calculi. Digital ureteroscopes and imaging allow for better quality visualisation. There are many instruments available to assist with lithotripsy, including baskets, ureteric access sheaths and anti-retropulsion devices. Laser lithotripsy still remains the most popular method for stone fragmentation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Scales CD Jr. Practice patterns in the management of urinary lithiasis. Curr Urol Rep 2013;14:154-7. [PubMed]
- Basillote JB, Lee DI, Eichel L, et al. Ureteroscopes: flexible, rigid, and semirigid. Urol Clin North Am 2004;31:21-32. [PubMed]
- Haberman K, Ortiz-Alvarado O, Chotikawanich E, et al. A dual-channel flexible ureteroscope: evaluation of deflection, flow, illumination, and optics. J Endourol 2011;25:1411-4. [PubMed]
- Rosa M, Usai P, Miano R, et al. Recent finding and new technologies in nephrolitiasis: a review of the recent literature. BMC Urol 2013;13:10. [PubMed]
- Beiko DT, Denstedt JD. Advances in ureterorenoscopy. Urol Clin North Am 2007;34:397-408. [PubMed]
- Haleblian GE, Springhart WP, Maloney ME, et al. Digital video ureteroscope: a new paradigm in ureteroscopy. J Endourol 2005;19:a80.
- Traxer O, Dubosq F, Jamali K, et al. New-generation flexible ureterorenoscopes are more durable than previous ones. Urology 2006;68:276-9. [PubMed]
- Khanna R, Monga M. Instrumentation in endourology. Ther Adv Urol 2011;3:119-26. [PubMed]
- Borofsky MS, Shah O. Advances in ureteroscopy. Urol Clin North Am 2013;40:67-78. [PubMed]
- Bach C, Nesar S, Kumar P, et al. The new digital flexible ureteroscopes: ‘size does matter’--increased ureteric access sheath use! Urol Int 2012;89:408-11. [PubMed]
- Gyrus-ACMI. Urology & Gynaecology Division: Product Catalog2007: Available online: http://www.surmedicalchile.cl/catalogos_pdf/acsi_uro_gyn_2007_product_catalog.pdf
- Shah K, Monga M, Knudsen BE. Prospective randomized trial comparing two flexible digital ureteroscopes: Gyrus ACMI/Olympus Invisio DUR-D and Olympus URF-V (abstract no. 2118). J Urol 2010;183:e823.
- Multescu R, Geavlete B, Georgescu D, et al. Conventional fiberoptic flexible ureteroscope versus fourth generation digital flexible ureteroscope: a critical comparison. J Endourol 2010;24:17-21. [PubMed]
- Cauberg EC, de Bruin DM, Faber DJ, et al. A new generation of optical diagnostics for bladder cancer: technology, diagnostic accuracy, and future applications. Eur Urol 2009;56:287-96. [PubMed]
- Traxer O, Geavlete B, de Medina SG, et al. Narrow-band imaging digital flexible ureteroscopy in detection of upper urinary tract transitional-cell carcinoma: initial experience. J Endourol 2011;25:19-23. [PubMed]
- Jichlinski P, Jacqmin D. Photodynamic Diagnosis in Non-Muscle-Invasive Bladder Cancer. European Urology, Supplements 2008;7:529-35.
- Somani BK, Moseley H, Eljamel MS, et al. Photodynamic diagnosis (PDD) for upper urinary tract transitional cell carcinoma (UT-TCC): evolution of a new technique. Photodiagnosis Photodyn Ther 2010;7:39-43. [PubMed]
- Dickstein RJ, Kreshover JE, Babayan RK, et al. Is a safety wire necessary during routine flexible ureteroscopy? J Endourol 2010;24:1589-92. [PubMed]
- Eandi JA, Hu B, Low RK. Evaluation of the impact and need for use of a safety guidewire during ureteroscopy. J Endourol 2008;22:1653-8. [PubMed]
- Clayman M, Uribe CA, Eichel L, et al. Comparison of guide wires in urology. Which, when and why? J Urol 2004;171:2146-50. [PubMed]
- Sarkissian C, Korman E, Hendlin K, et al. Systematic evaluation of hybrid guidewires: shaft stiffness, lubricity, and tip configuration. Urology 2012;79:513-7. [PubMed]
- Weiland D, Canales BK, Monga M. Medical devices used for ureteroscopy for renal calculi. Expert Rev Med Devices 2006;3:73-80. [PubMed]
- Ng YH, Somani BK, Dennison A, et al. Irrigant flow and intrarenal pressure during flexible ureteroscopy: the effect of different access sheaths, working channel instruments, and hydrostatic pressure. J Endourol 2010;24:1915-20. [PubMed]
- Monga M, Best S, Venkatesh R, et al. Prospective randomized comparison of 2 ureteral access sheaths during flexible retrograde ureteroscopy. J Urol 2004;172:572-3. [PubMed]
- Pedro RN, Hendlin K, Durfee WK, et al. Physical characteristics of next-generation ureteral access sheaths: buckling and kinking. Urology 2007;70:440-2. [PubMed]
- Garg S, Mandal AK, Singh SK, et al. Ureteroscopic laser lithotripsy versus ballistic lithotripsy for treatment of ureteric stones: a prospective comparative study. Urol Int 2009;82:341-5. [PubMed]
- Bagley DH. Expanding role of ureteroscopy and laser lithotripsy for treatment of proximal ureteral and intrarenal calculi. Curr Opin Urol 2002;12:277-80. [PubMed]
- Sofer M, Watterson JD, Wollin TA, et al. Holmium:YAG laser lithotripsy for upper urinary tract calculi in 598 patients. J Urol 2002;167:31-4. [PubMed]
- Watterson JD, Girvan AR, Beiko DT, et al. Ureteroscopy and holmium:YAG laser lithotripsy: an emerging definitive management strategy for symptomatic ureteral calculi in pregnancy. Urology 2002;60:383-7. [PubMed]
- Watterson JD, Girvan AR, Cook AJ, et al. Safety and efficacy of holmium: YAG laser lithotripsy in patients with bleeding diatheses. J Urol 2002;168:442-5. [PubMed]
- Aboumarzouk OM, Monga M, Kata SG, et al. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol 2012;26:1257-63. [PubMed]
- Kuo RL, Aslan P, Zhong P, et al. Impact of holmium laser settings and fiber diameter on stone fragmentation and endoscope deflection. J Endourol 1998;12:523-7. [PubMed]
- Poon M, Beaghler M, Baldwin D. Flexible endoscope deflectability: changes using a variety of working instruments and laser fibers. J Endourol 1997;11:247-9. [PubMed]
- Sung C, Singh H, Schwartz M, et al. Evaluation of efficacy of novel optically activated digital endoscope protection system against laser energy damage. Urology 2008;72:57-60. [PubMed]
- Xavier K, Hruby GW, Kelly CR, et al. Clinical evaluation of efficacy of novel optically activated digital endoscope protection system against laser energy damage. Urology 2009;73:37-40. [PubMed]
- Herrmann TR, Bach T, Imkamp F, et al. Insertion sheaths prevent breakage of flexible ureteroscopes due to laser fiber passage: a video-endoluminal study of the working channel. J Endourol 2010;24:1747-51. [PubMed]
- Korman E, Hendlin K, Monga M. Small-diameter nitinol stone baskets: radial dilation force and dynamics of opening. J Endourol 2011;25:1537-40. [PubMed]
- Magheli A, Semins MJ, Allaf ME, et al. Critical analysis of the miniaturized stone basket: effect on deflection and flow rate. J Endourol 2012;26:275-7. [PubMed]
- Blew BD, Dagnone AJ, Fazio LM, et al. Practical comparison of four nitinol stone baskets. J Endourol 2007;21:655-8. [PubMed]
- Eisner BH, Dretler SP. Use of the Stone Cone for prevention of calculus retropulsion during holmium:YAG laser lithotripsy: case series and review of the literature. Urol Int 2009;82:356-60. [PubMed]
- Ding H, Wang Z, Du W, et al. NTrap in prevention of stone migration during ureteroscopic lithotripsy for proximal ureteral stones: a meta-analysis. J Endourol 2012;26:130-4. [PubMed]
- Lee HJ, Box GN, Abraham JB, et al. In vitro evaluation of nitinol urological retrieval coil and ureteral occlusion device: retropulsion and holmium laser fragmentation efficiency. J Urol 2008;180:969-73. [PubMed]
- Pagnani CJ, El Akkad M, Bagley DH. Prevention of stone migration with the Accordion during endoscopic ureteral lithotripsy. J Endourol 2012;26:484-8. [PubMed]
- Huffman JL, Bagley DH, Schoenberg HW, et al. Transurethral removal of large ureteral and renal pelvic calculi using ureteroscopic ultrasonic lithotripsy. J Urol 1983;130:31-4. [PubMed]
- Mirabile G, Phillips CK, Edelstein A, et al. Evaluation of a novel temperature-sensitive polymer for temporary ureteral occlusion. J Endourol 2008;22:2357-9. [PubMed]
- Rane A, Bradoo A, Rao P, et al. The use of a novel reverse thermosensitive polymer to prevent ureteral stone retropulsion during intracorporeal lithotripsy: a randomized, controlled trial. J Urol 2010;183:1417-21. [PubMed]
- Ghani KR, Bultitude M, Hegarty N, et al. Flexible ureterorenoscopy (URS) for lower pole calculi. BJU Int 2012;110:294-8. [PubMed]
- Bostanci Y, Ozden E, Atac F, et al. The double wire technique: an alternative method for difficult ureteroscopic access. Urol Res 2012;40:783-4. [PubMed]
- Laing KA, Lam TB, McClinton S, et al. Outcomes of ureteroscopy for stone disease in pregnancy: results from a systematic review of the literature. Urol Int 2012;89:380-6. [PubMed]
- Tiselius HG, Ackermann D, Alken P, et al. Guidelines on urolithiasis. Eur Urol 2001;40:362-71. [PubMed]


