
Temporal trends of kidney cancer incidence and mortality from 1990 to 2016 and projections to 2030
Introduction
Kidney cancer accounts for a large proportion of urologic caner and leads to large amount of people’s death (1). In the context of a growing and aging global population, kidney cancer is considered to be growing both in incidence among older individuals and men (2). It has become a threat to the health of people in most countries. Worldwide, kidney cancer is the sixth most frequently diagnosed cancer in men and the tenth most common cancer in women, accounting for an estimated 73,820 new cases and 14,770 deaths in 2019 (3). It can be seen that the burden of disease caused by kidney cancer is very worthy of attention.
Due to the international variations in morbidity and mortality of urologic cancer, people are increasingly interested in the burden of urinary cancer (4-7). As growing demands for relative knowledge about kidney cancer, epidemiology researches are urgently needed as inference to make health decisions. However, prior studies lacked analysis of temporal trends in morbidity and mortality in kidney cancer, as well as analysis of morbidity and mortality by sex, age, SDI and region. Decision makers are supposed to provide effective policies on kidney cancer prevention, screening and treatment and sensible allocation of health care resources. But necessary data to develop health policies for kidney cancer worldwide, including epidemiology of kidney cancer and future trends of incidence and mortality rates, are not widely available.
Description of temporal trends in incidence and mortality of kidney cancer is essential for its future prevention and control. In this study, we aim to present these over-time trends from 1990 to 2016 by age, sex, region, and SDI, and then, based on the large amount data of kidney cancer incidence and deaths, we forecast the future trends of incidence and mortality worldwide to 2030. Finally, we point out countries and regions with high incidence of kidney cancer in the future and provide epidemiology reference for future prevention and control of kidney cancer. Paying attention to incidence characteristics of kidney cancer is essential for providing detailed information on kidney cancer prevention and screening.
Methods
We extracted the kidney cancer incidence and mortality data from the Global Burden of Disease Study (GBD) database (ghdx.healthdata.org). Detailed analytical methods for estimating the incidence, mortality, disability-adjusted life-years (DALYs) have been reported previously (8-13). The present study and detailed approach are in line with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) (14). Explanations of the estimation process and all materials as well as data involved in the methodology can be found in the numerous tables in the Supplementary materials (Tables S1-S7 and tables online: http://cdn.amegroups.cn/static/application/bf0515116d9e2a9f90889619ab2e5cce/tau.2020.02.23-1.pdf; http://cdn.amegroups.cn/static/application/9f3529822bfb26286fdf162547922d15/tau.2020.02.23-2.pdf) (9,15-17). International Classification of Diseases 10 (ICD-10) codes mapped to the GBD cause list for kidney cancer incidence and mortality are C64-C64.2, C64.9-C65.9, Z80.51, Z85.52-Z85.54 and C64-C65.9, D30.0-D30.1, D41.0-D41.1, respectively. For the year 2016, we assessed national kidney cancer burden for 195 countries and territories. All rates are reported per 100,000 person-years. The age-standardized rates were calculated according to the GBD world population standard (1). Uncertainty intervals (UIs) were also reported for all estimates.

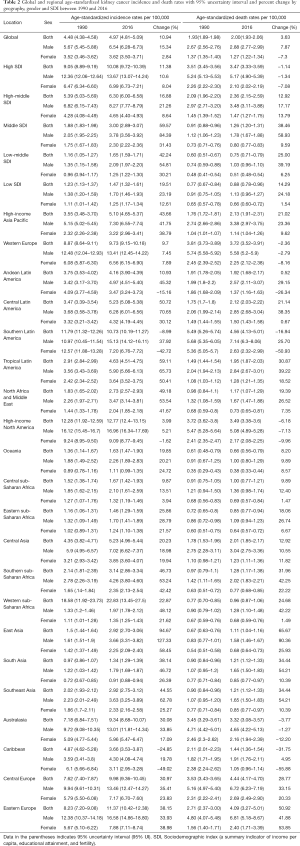
Full table
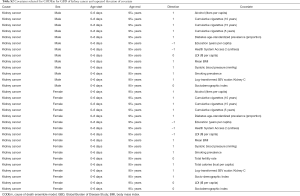
Full table
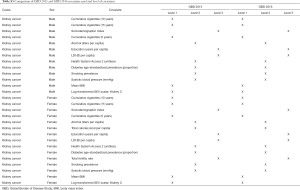
Full table

Full table

Full table

Full table
Full table
Data for the death rates of kidney cancer were obtained from vital registration systems and cancer registries. Cancer incidence data are used to simulate mortality in places where do not contain cancer mortality data by multiplying the incidence by mortality-to-incidence ratio which is separately modeled. These mortality estimates are classified as mortality data from the other sources and are used in a cause of death ensemble model (CODEm) (9,13). Cancer incidence rates were estimated by dividing the final cancer-specific mortality estimates by the mortality-to-incidence ratio. As in the GBD 2015, we estimated the impact of population ageing, population growth, and change in age-specific rates on the change of incident cases from 2006 to 2016 (8). Results were stratified by using sociodemographic index (SDI) countries. SDI is a comprehensive indicator which includes fertility, education and income. It has been proved that SDI has a good correlation with health outcomes (Supplementary materials) (8). All the data was analyzed by R software (x64 version 3.5.1), SAS (version 9.3) and SPSS (version 22.0).
Results
Over-time trends of incident cases of kidney cancer from 1990 to 2016
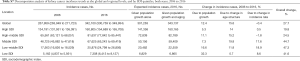
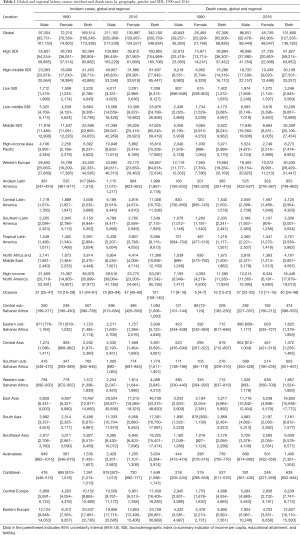
Globally, kidney cancer incident cases increased by nearly 102% from 1990 (169,514; 95% UI, 166,246–173,338) to 2016 (342,100; 95% UI, 330,759–349,934). For SDI countries, in terms of absolute numbers, the highest kidney cancer incidence rates occurred in high SDI countries (160,805, 95% UI, 154,689–165,708), followed by high-middle SDI countries (81,637; 95% UI, 77,842–85,447), middle SDI countries (67,625; 95% UI, 65,243–69,419), low-middle SDI countries (25,876; 95% UI, 24,799–26,806), and low SDI countries (7,308; 95% UI, 6,413–8,127) in both sexes. Among regions, the three highest kidney cancer incident rates were observed in Eastern Europe (68,857; 95% UI, 64,818–72,034), high-income North America (63,291; 95% UI, 61,542–65,156), and East Asia (46,739; 95% UI, 43,375–48,820). In 2016, kidney cancer was more common in men, with 211,102 incident cases compared to women, with 130,997 cases (Table 1).
Full table
Over-time trends of deaths of kidney cancer from 1990 to 2016
Globally, there were 131,800 (95% UI, 127,335–136,185) deaths from kidney cancer in 2016, nearly 2.0-fold the number in 1990 (67,306; 95% UI, 65,806–68,836). Death rates changed by 3.63% from 1990 to 2016 at a global level. Among SDI countries, the highest burden of kidney cancer deaths occurred in high SDI countries (61,827; 95% UI, 59,214–63,852), followed by high-middle SDI countries (30,159; 95% UI, 27,501–33,257), middle SDI countries (26,309; 95% UI, 25,106–27,454), low-middle SDI countries (10,209; 95% UI, 9,667–10,688), and low SDI countries (3,246; 95% UI, 2,845–3,569) in both sexes. In terms of regions, Western Europe (30,035; 95% UI, 28,249–31,447) had the highest number of kidney cancer deaths in both sexes. High-income North America (18,446; 95% UI, 17,879-19,013) ranked second for kidney cancer deaths. East Asia (16,955; 95% UI, 15,938–17,772) experienced the third highest number of kidney cancer deaths in both sexes. In 2016, mortality of kidney cancer was much higher in men compared to women, with the death cases number of 86,051 and 45,749, respectively (Table 1).
Over-time trends of kidney cancer in age-standardized incidence rate (ASIR) from 1990 to 2016
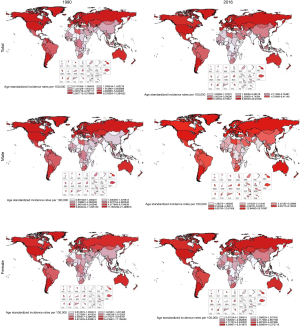
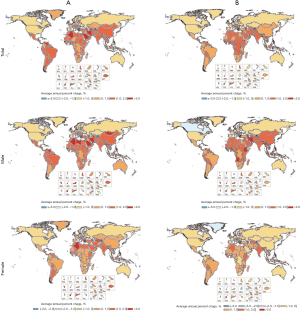
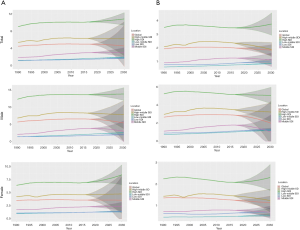
Globally, ASIR changed by 10.94% from 1990 to 2016. High SDI countries had the highest ASIR in 2016, followed by high-middle SDI and middle SDI countries. The change pattern of ASIR between 1990 and 2016 reveals a significant increase of over 100% in East Asia (3.66; 95% UI, 3.31–3.82) in males and (2.92; 95% UI, 2.70–3.06) in both sexes. Concomitantly, some regions with high incidence rates such as Central Latin America (50.72% for both sexes, and 70.65% for males), tropical Latin America (59.11% for both sexes, 65.73% for males, and 50.41% for females), and North Africa and the Middle East (53.54% for males) experienced an increase of over 50% in ASIR. The highest male-to-female ratio for ASIR could be found in East Asia at 2.9 while Andean Latin America had the lowest male-to-female ratio at 0.9. Globally, the age-standard kidney cancer incidence rate (per 100,000 people) in 2016 among men [6.54 (6.28–6.73)] was 1.8 times higher than among women [3.62 (3.50–3.71)]. ASIRs for both sexes increased significantly from 1990 to 2016, with the greatest increases among men (Table 2, Figures 1,2).
Full table
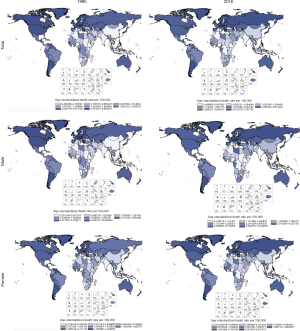
Over-time trends of kidney cancer in age-standardized death rate (ASDR) from 1990 to 2016
Among SDI countries, the highest changes in ASDR between 1990 and 2016 increased in middle SDI countries (38.46% for both sexes, 58.93% for males). Regionally, the highest changes in ASDR between 1990 and 2016 increased in East Asia, followed by Eastern Europe, South Asia, and Southeast Asia. ASDR decreased significantly in regions with high kidney cancer burdens such as Southern Latin America and the Caribbean. On a global scale, the male-to-female ratios for ASIR and ASDR rates were 1.8 and 2.3, respectively. Globally, the age-standard kidney cancer death rate (per 100,000 people) among men [2.88 (2.77–2.99)] was approximately 2.3-fold as high as among women [1.27 (1.22–1.34)]. Deaths from kidney cancer increased in both sexes and different age groups, with an annual growth rate of 3.63%. However, ASDRs for females decreased 7.30% (Table 2, Figures 2,3).
Projections of kidney cancer incidence and mortality from 2017 to 2030
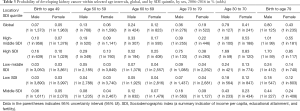
Based on the analytical period, we predicted the future trends of incidence and mortality rates of kidney cancer. As a result of these trends, by 2030, kidney cancer in both sexes are projected to increase substantially in high SDI, followed by middle SDI, low-middle SDI, and low SDI countries, while the trends in incidence rates will remain stable globally and in high-middle SDI countries. Furthermore, high SDI and low SDI countries will also have increased mortality rates from kidney cancers, while decreased mortality rates from kidney cancer will be observed in high-middle SDI countries. Globally, the trends in deaths due to kidney cancer will remain stable. The estimated risk of kidney cancer for males within the age of 30 and 70 is around 0.79% compared to 0.41% for female. Similar results can be seen in other age intervals and in SDI countries. In other words, the probability of developing kidney cancer is generally higher in male than in female (Table 3 and Figure 4).
Full table
Discussion
Globally, over-time trends of kidney cancer incidence and death rates are increasing significantly, especially in older age groups and high SDI countries where life expectancy gains are greater. Worldwide, incident cases of kidney cancer increased by nearly 102% from 1990 (169,514; 95% UI, 166,246-173,338) to 2016 (342,100; 95% UI, 330,759–349,934). Among all SDI countries and most regions, we found the similar increased over-time trends in kidney cancer incidence rates from 1990 and 2016. There were 131,800 (95% UI, 127,335–136,185) death cases from kidney cancer in 2016, nearly 2.0-fold compared to the number in 1990 (67,306; 95%UI, 65,806–68,836).
The highest ASIR in 2016 was found in high SDI countries. The highest ASDR was found in middle SDI countries, while ASDR decreased significantly in regions with high kidney cancer burdens including Southern Latin America as well as the Caribbean. The clinical outcomes of kidney cancer depend on health care expenditures as well as early precise diagnosis and treatment (13). Risk of developing kidney cancer and trends of deaths were evaluated for both sexes, and most incident and death rates were greater in males than females across all SDI countries and most regions. Overall, the burden of kidney cancer is significantly higher in males than in females.
Life expectancy and population growth account for a large proportion of the increase in the incidence of kidney cancer (18). However, over-time trends of kidney cancer incidence and the difference of incident rates among variable countries may be influenced by some other elements. For instance, poor lifestyles of smoking, and obesity as well as excess body mass index (BMI: defined as 25 kg/m2 or greater) have been identified as crucial contributor of kidney cancer (19). In higher-income countries, the increase in kidney cancer incident cases may partially as a result of the increase in the occasional detection of abnormal kidney changes when performing abdominal imaging for diseases of other systems (20). Multi-factors have been found contributed to the increased mortality rates of kidney cancer, such as, tobacco smoking-related and rising obesity-attributed deaths, high BMI, hypertension, or pharmacologic control of hypertension. In these years, the role of gene-gene and gene-environmental functions and/or interactions have received increasing attention in disease development and progress.
Kidney cancer incidence and deaths will substantially increase at a global level, while decreased trends will also be found in some SDI countries and regions. By 2030, kidney cancers in both sexes are projected to increase substantially in high SDI, followed by middle SDI, low-middle SDI, and low SDI countries, while the over-time trends of kidney cancer incidence rates will remain stable globally and in high-middle SDI countries. Furthermore, high SDI and low SDI countries will also have increased mortality rates from kidney cancers, while decreased mortality rates from kidney cancer will be observed in high-middle SDI countries. Globally, the trends in deaths due to kidney cancer will remain stable. Due to the population expansion and ageing, the time trends in kidney cancer incidence and mortality is substantially increasing. Reducing the risk of developing kidney cancer is a challenge for our doctors and will require commitments of all sectors of society. The time trends presented in this study will be helpful particularly in health care resource allocation planning as a window for the future, which is a necessary condition for notification of health policy, adjust health care policy, screen guidelines accordingly, and make resource allocation decisions. What had been found in this study allow for insight into future global kidney cancer demands based on observed trends.
This study also has some limitations, data from GBD are reported by using traditional epidemiologic methods, which often have a 3-year delay main due to the data collection. The trends in kidney cancer incidence and mortality in the recent three years may be different from the results we predicted, resulting in a slight deviation in the predictions afterwards. On the other hand, our results are only predicted until 2030 and more data are required due to the need for accuracy to make longer-term predictions.
Conclusions
The incidence and mortality rate of kidney cancer have uniformly increased among different countries since 1990. By 2030, the incidence and mortality of kidney cancer will be steadily increasing globally. An epidemiology reference for policy makers is absolutely necessary to adjust health care policy, screen guidelines, and make resource allocation decisions. The appropriate allocation of limited resources is also imperative for kidney cancer prevention, screening, and treatment. The above results show that the future incidence of kidney cancer will grow continuously by 2030 especially in high SDI countries, middle SDI, low-middle SDI, and low SDI countries, where medical workers and researchers should intensively focus on the health care systems to ensure whether previously informed policies are adapted to the future incidence trend of kidney cancer in their countries.
Acknowledgments
Funding: This study was funded by the National Natural Science Foundation of China (No. 91746205), IBM Global University Programs (2018 IBM Shared University Research Award), Tianjin Technical Expert Project and Hospital Innovation & Management Research Project of Tianjin Medical University (No. 2019YG08). We thank the Global Burden of Disease Study for collection of the GBD data.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau.2020.02.23). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Akinyemiju TF, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2016: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2018;4:1553-68. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018;68:7-30. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. [Crossref] [PubMed]
- Chavan S, Bray F, Lortet-Tieulent J, et al. International variations in bladder cancer incidence and mortality. Eur Urol 2014;66:59-73. [Crossref] [PubMed]
- Znaor A, Lortet-Tieulent J, Laversanne M, et al. International variations and trends in renal cell carcinoma incidence and mortality. Eur Urol 2015;67:519-30. [Crossref] [PubMed]
- Center MM, Jemal A, Lortet-Tieulent J, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol 2012;61:1079-92. [Crossref] [PubMed]
- Antoni S, Ferlay J, Soerjomataram I, et al. Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol 2017;71:96-108. [Crossref] [PubMed]
- Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2017;3:524-48. [Crossref] [PubMed]
- GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151-210. [Crossref] [PubMed]
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1260-344. [Crossref] [PubMed]
- Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Dicker D, et al. The Global Burden of Cancer 2013. JAMA Oncol 2015;1:505-27. [Crossref] [PubMed]
- GBD 2013 Risk Factors Collaborators, Forouzanfar MH, Alexander L, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287-323.
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743-800. [Crossref] [PubMed]
- Stevens GA, Alkema L, Black RE, et al. GATHER Working Group. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. PLoS Med 2016;13:e1002056. [Crossref] [PubMed]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211-59. [Crossref] [PubMed]
- GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1345-422. [Crossref] [PubMed]
- GBD 2016 Mortality Collaborators. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1084-150. [Crossref] [PubMed]
- Renehan AG, Tyson M, Egger M, et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008;371:569-78. [Crossref] [PubMed]
- Capitanio U, Bensalah K, Bex A, et al. Epidemiology of Renal Cell Carcinoma. Eur Urol 2019;75:74-84. [Crossref] [PubMed]


