Epidemiology of urethral strictures
Introduction
As urethral stricture causes progressive narrowing of the urethral lumen, symptoms and signs of urinary obstruction arise. Patients experience weak stream, straining to urinate, incomplete emptying, post-void dribbling, urinary retention, and recurrent urinary tract infections. The symptoms resemble those of other causes of bladder outlet obstruction such as benign prostatic hyperplasia. The presence of obstructed ejaculation also points to urethral stricture and is a cause of infertility. Urethral stricture needs to be ruled out in patients presenting with Fournier’s gangrene, especially when there is urinary extravasation, and in young patients with recurrent epididymitis or prostatitis. In cases of meatal stenosis, the urinary stream will be splayed or deviated. On examination, associated spongiofibrosis may be palpated periurethrally.
Understanding the epidemiology of urethral strictures helps to identify risk factors for disease occurrence or progression, which may be amenable to preventive measures resulting in reduced disease severity and health care expenditure. This article provides a comprehensive review of the epidemiology of urethral stricture disease including incidence and prevalence, etiology, and epidemiology. A critical review was performed using the Medline database from 1990—present with the search terms “epidemiology”, “urethral stricture”, and “trauma”. We identified additional articles through citation examination.
Incidence
Urethral stricture is a relatively common disease in men with an associated prevalence of 229-627 per 100,000 males, or 0.6% of the at risk population, who are typically older men (1). Santucci et al. (1) analyzed urethral stricture disease in ten public and private data sets in the United States. They concluded that urethral stricture disease is common in the elderly population with a marked increase after 55 years of age. Data from Medicare and Medicaid Services (for patients older than 65 years) confirmed an increased incidence of stricture disease at 9.0/100,000 for 2001 compared to 5.8/100,000 in patients younger than 65 years. In addition, outpatient hospital visits for Medicare patients was 21/100,000 in 2001, which is half the number of urolithiasis visits in the same population, emphasizing the importance of this disease in the elderly population. The hospitalization rate for urethral stricture disease is nowadays lower than before as the Healthcare Cost and Utilization Project data revealed a hospitalization rate at 3.8/100,000 in 2000 (which is 50% less than in 1994). With regards to outpatient procedures, the National Survey of Ambulatory Surgery data for the annualized rate of ambulatory surgery center visits pooled from 1994 to 1996 was found to be 60/100,000. In patients with urethral stricture disease older than 60 years, 6.5% underwent retrograde urethrography (RUG) studies. Urethral dilation remains a very common outpatient procedure among Medicare beneficiaries, and even though it was reduced by half in 2001 at 19,658/100,000 compared to 1992, it was still double the number of ureteroscopies performed in the same population. Patients with urethral stricture are considered a vulnerable population as they experienced high rates of UTIs (41%) and incontinence (11%) as sequelae of the disease (1,2). However, multiple data sets they examined suggest that the rate of urethral stricture hospitalization and treatments decreased with time potentially due to a hypothetically decreased incidence/prevalence of the disease and/or increased success of strictures treatment. Some of the data sets indicate that Black Americans are at a higher risk of urethral stricture disease than White Americans, with sample numbers too low to draw accurate conclusions for Asian, Hispanic, and Native American patients (1).
In addition, Santucci et al. demonstrated the high health care cost for treatment of urethral stricture disease. The total annual expenditure for stricture disease was 191 million dollars in 2000 with 69% of costs paid for ambulatory surgery visits. Individual healthcare expenditure for an insured male with urethral stricture disease was almost 3-fold higher compared to males without stricture disease ($10,472 vs. $3,713) (1). Other reports estimated a decreased lifetime treatment cost for urethral stricture disease in the U.S. if a patient received immediate urethral reconstruction, $16,444, compared with receiving repeat urethrotomies, $17,747 (3).
Recently, Palminteri et al. (4) evaluated urethral stricture characteristics in Italy using data from 1,439 male patients that were referred to specialized genitourinary reconstructive centers. The mean age of urethral stricture presentation was 45.1 years (range, 2-84 years). The mean length of stricture was 4.2 cm with the vast majority of strictures occurring in the anterior urethra (92.2%), in particular the bulbar urethra (46.9%). Of note, patients with bulbar strictures tended to be younger than patients with strictures in all the other parts of the urethra. The majority of patients, 73.6%, received some form of surgical intervention for their stricture disease prior to presentation to the referral center. Most of these patients (32.1%) had already undergone more than one procedure, and 23.2% had undergone urethrotomy alone. Of these patients, 97.4% required urethroplasty for management of their stricture disease, and only 2.6% underwent urethrotomy.
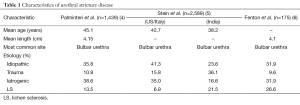
Stein et al. (5) looked retrospectively at 2,589 patients who underwent urethroplasty procedures from 2000 to 2011 in the USA, Italy, and India. Similar to the results of the previous study, men presented at a mean age of 41.4 years with similar etiologies of their stricture disease (see Table 1). Fenton et al. (6) looked retrospectively at 175 patients with anterior urethral stricture in Texas and Honduras and identified the mean stricture length at 4.1 cm, with the bulbar urethra being the most common site constituting 52% of the cases. Infection-induced strictures, including lichen sclerosis (LS), were reported as inflammatory strictures and were the third leading cause of stricture disease at 26.6% following idiopathic (31.9%) and iatrogenic causes (31.9%).
Full table
Etiology
Infection
Historically, infection urethritis was the leading cause of urethral strictures. However, with patient education and improved diagnosis and treatment methods of sexually transmitted diseases, infectious urethritis is now responsible for only a small proportion of cases (7). Currently in the developed world, most urethral strictures are iatrogenic or idiopathic with infection urethritis causing the minority of stricture (4-6). There is significant variation in the etiology of urethral stricture disease in different parts of the world as demonstrated by several single-institution studies (5,8-10). Infection was a cause of urethral strictures in only 15.2% of cases in Brazil (9), while in Nigeria it was found to be the cause of 66.5% of the cases, causing multi-location strictures 85% of the time (11).
Post-trauma
Trauma represents a very significant etiology of urethral stricture disease. Different mechanisms of trauma result in urethral strictures with straddle injury being the most common (4). Other mechanisms of traumatic injury include pelvic fracture-related urethral injury (PFUI) and iatrogenic injury secondary to instrumentation. Straddle injuries typically occur during work, bicycle riding, and sports. Different reports suggest that trauma is the cause of urethral stricture disease in 9.6-36.1% of cases (4-6).
In several small series, PFUI was reported to have a prevalence of 5-25% (12,13), however in a recent review of the National Trauma Data Bank (NTDB), the prevalence was reported at 1.54% (14). This NTDB review also showed a prolonged hospitalization with a median stay of four more days in this subset of patients. The most common mechanism of injury was motor vehicle collisions and patients were more likely to have concomitant bowel and/or reproductive organs injuries. PFUI was not found to be an independent predictor of mortality in this set of trauma patients. PFUI usually results in in a distraction defect at the bulbomembranous junction and the standard treatment is Suprapubic Catheter Placement and delayed repair. There is an increasing evidence for the benefits of primary realignment in terms of preventing stricture in a minority of patients, decreasing the gap of defect, and making the subsequent urethroplasty easier. However, this is still debatable and the superiority of one approach over the other is controversial (15).
Urethral injury in children represents a rather uncommon but difficult clinical scenario, and consensus over the best surgical approach for repair is lacking. Children tend to have more supramembranous involvement because of the confined pelvis, resulting in a more unpredictable outcome (16).
Lichen sclerosis (LS)
LS is considered a chronic inflammatory condition of unknown etiology (17). There are several theories on the etiology of LS. The most widely accepted theory involves immune dysregulation given that organ-specific antibodies and an increased incidence of other autoimmune disorders are found in patients with LS. LS can involve any cutaneous area but has a predilection for the anogenital region. Genital LS is known to be an important cause of urethral stricture. The incidence of genital LS and its involvement of the urethra is unknown, but case series demonstrate the urethral stricture rate secondary to LS to be 8-16% (7,18). LS most commonly affect Caucasian patients with a female to male ratio of 6:1 (19). LS can affect any age group. It involves the glans and foreskin only in 57% of cases, the urethral meatus in 4%, and the urethra in 20% of cases (20). LS does not involve the posterior urethra. Palminteri et al. demonstrated that LS is a cause of stricture in 13.5% of cases and is the most common cause of panurethral stricture (48.6%) (4). The mechanism of urethral involvement in LS is unclear and may be due to a direct extension of the disease or may be secondary to an obstructive voiding pattern triggered by the meatal stenosis causing progressive inflammation of the periurethral glands (21).
Post-prostate cancer treatment
All forms of prostate cancer interventions may be associated to with differing degrees of urethral stricture development. The reported incidence of urethral stricture after radical prostatectomy (RP) is quite variable, ranging from 2.7% to 25.7%, and usually is a bladder neck contracture (BNC) (22,23). Post-prostatectomy stricture could be related to a narrow anastomosis or lack of mucosal apposition. Urethral stricture risk was found to be higher after open RP vs. robotic RP (7.5% vs. 2.1%) (24). Independent predictors for urethral stricture development after RP include open surgery, PSA recurrence, postoperative hematuria, urinary leak, and urinary retention. Patient-related risk factors include smoking, diabetes mellitus, and renal insufficiency (25).
The urethral stricture rate after external beam radiation therapy (EBRT) is known to be to be low with a reported rate of 2% (26). After brachytherapy the risk is higher and has been reported in some series as high as 12% (27,28). High-dose brachytherapy is associated with more risk of post-treatment urethral stricture than both low-dose brachytherapy and EBRT, which implies a biologic equivalent dose (BED) related effect. Higher fractionation schedule of brachytherapy was associated with an increased risk of stricture while PSA level of <10 was associated a reduced risk of stricture (29).
Meatal stenosis post-circumcision
Circumcision is considered one of the most common surgical procedures. It can be performed at any age but is most commonly done in neonates. An important complication of circumcision is meatal stenosis. This complication has been reported in fewer than 0.2% of children who underwent the procedure at neonatal age and represents 23% of the overall complication rate of circumcision (30,31). When meatal stenosis occurs, the child usually develops symptoms of dysuria, frequency, and weak stream, but urinary obstruction is rare. In about 25% of patients with meatal stenosis the presentation is silent (32).
Table 1 provides a summary for the different characteristics and etiologies of urethral strictures. A significant portion of urethral strictures is idiopathic with a range between 23.6-41.3%. Iatrogenic strictures constitute another important cause of stricture in 16.6-38.6% of cases. Catheterization remains the most common cause, and other causes include transurethral surgery and failed hypospadias repair (4-6).
Conclusions
Urethral stricture disease is relatively common, and in many instances debilitating. The etiology of urethral stricture disease varies geographically. In general, the incidence of infection-related urethral stricture has decreased, especially in the developed world. In this review we examined the available incidence and prevalence data for urethral stricture disease. Further research is required to better delineate etiology of urethral strictures. Nearly a third of urethral stricture cases are idiopathic. Identifying cause in these cases may help to identify treatment options that could prevent disease development. Also, it is important to identify factors that could diminish iatrogenic causes. Lastly, better understanding and medical treatment of LS would lead to better control of its subsequent development and recurrence of strictures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol 2007;177:1667-74. [PubMed]
- Anger JT, Santucci R, Grossberg AL, et al. The morbidity of urethral stricture disease among male medicare beneficiaries. BMC Urol 2010;10:3. [PubMed]
- Rourke KF, Jordan GH. Primary urethral reconstruction: the cost minimized approach to the bulbous urethral stricture. J Urol 2005;173:1206-10. [PubMed]
- Palminteri E, Berdondini E, Verze P, et al. Contemporary urethral stricture characteristics in the developed world. Urology 2013;81:191-6. [PubMed]
- Stein DM, Thum DJ, Barbagli G, et al. A geographic analysis of male urethral stricture aetiology and location. BJU Int 2013;112:830-4. [PubMed]
- Fenton AS, Morey AF, Aviles R, et al. Anterior urethral strictures: etiology and characteristics. Urology 2005;65:1055-8. [PubMed]
- Lumen N, Hoebeke P, Willemsen P, et al. Etiology of urethral stricture disease in the 21st century. J Urol 2009;182:983-7. [PubMed]
- Fall B, Sow Y, Mansouri I, et al. Etiology and current clinical characteristics of male urethral stricture disease: experience from a public teaching hospital in Senegal. Int Urol Nephrol 2011;43:969-74. [PubMed]
- Mathur R, Aggarwal G, Satsangi B, et al. Comprehensive analysis of etiology on the prognosis of urethral strictures. Int Braz J Urol 2011;37:362-9. [PubMed]
- Steenkamp JW, Heyns CF, de Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: a prospective, randomized comparison. J Urol 1997;157:98-101. [PubMed]
- Ahmed A, Kalayi GD. Urethral stricture at Ahmadu Bello University Teaching Hospital, Zaria. East Afr Med J 1998;75:582-5. [PubMed]
- Pokorny M, Pontes JE, Pierce JM Jr. Urological injuries associated with pelvic trauma. J Urol 1979;121:455-7. [PubMed]
- Coffield KS, Weems WL. Experience with management of posterior urethral injury associated with pelvic fracture. J Urol 1977;117:722-4. [PubMed]
- Bjurlin MA, Fantus RJ, Mellett MM, et al. Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Trauma 2009;67:1033-9. [PubMed]
- Leddy L, Voelzke B, Wessells H. Primary realignment of pelvic fracture urethral injuries. Urol Clin North Am 2013;40:393-401. [PubMed]
- Ranjan P, Ansari MS, Singh M, et al. Post-traumatic urethral strictures in children: what have we learned over the years? J Pediatr Urol 2012;8:234-9. [PubMed]
- Powell JJ, Wojnarowska F. Lichen sclerosus. Lancet 1999;353:1777-83. [PubMed]
- Pugliese JM, Morey AF, Peterson AC. Lichen sclerosus: review of the literature and current recommendations for management. J Urol 2007;178:2268-76. [PubMed]
- Meffert JJ, Davis BM, Grimwood RE. Lichen sclerosus. J Am Acad Dermatol 1995;32:393-416. [PubMed]
- Depasquale I, Park AJ, Bracka A. The treatment of balanitis xerotica obliterans. BJU Int 2000;86:459-65. [PubMed]
- Andrich DE, Mundy AR. What is the best technique for urethroplasty? Eur Urol 2008;54:1031-41. [PubMed]
- Park R, Martin S, Goldberg JD, et al. Anastomotic strictures following radical prostatectomy: insights into incidence, effectiveness of intervention, effect on continence, and factors predisposing to occurrence. Urology 2001;57:742-6. [PubMed]
- Kao TC, Cruess DF, Garner D, et al. Multicenter patient self-reporting questionnaire on impotence, incontinence and stricture after radical prostatectomy. J Urol 2000;163:858-64. [PubMed]
- Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA 2009;302:1557-64. [PubMed]
- Wang R, Wood DP Jr, Hollenbeck BK, et al. Risk factors and quality of life for post-prostatectomy vesicourethral anastomotic stenoses. Urology 2012;79:449-57. [PubMed]
- Zelefsky MJ, Wallner KE, Ling CC, et al. Comparison of the 5-year outcome and morbidity of three-dimensional conformal radiotherapy versus transperineal permanent iodine-125 implantation for early-stage prostatic cancer. J Clin Oncol 1999;17:517-22. [PubMed]
- Sarosdy MF. Urinary and rectal complications of contemporary permanent transperineal brachytherapy for prostate carcinoma with or without external beam radiation therapy. Cancer 2004;101:754-60. [PubMed]
- Elliott SP, Meng MV, Elkin EP, et al. Incidence of urethral stricture after primary treatment for prostate cancer: data From CaPSURE. J Urol 2007;178:529-34. [PubMed]
- Hindson BR, Millar JL, Matheson B. Urethral strictures following high-dose-rate brachytherapy for prostate cancer: analysis of risk factors. Brachytherapy 2013;12:50-5. [PubMed]
- Ceylan K, Burhan K, Yilmaz Y, et al. Severe complications of circumcision: an analysis of 48 cases. J Pediatr Urol 2007;3:32-5. [PubMed]
- American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics 2012;130:585-6. [PubMed]
- Mahmoudi H. Evaluation of meatal stenosis following neonatal circumcision. Urol J 2005;2:86-8. [PubMed]


