Ejaculatory physiology and pathophysiology: assessment and treatment in male infertility
Introduction
Before the advent of intracytoplasmic sperm injection (ICSI) and the development of surgical sperm retrieval, ejaculation was an absolute essential step in human reproduction. With advances in technology and a focus on a gamete-centric reproductive approach, ejaculatory disorders their treatments continue to be understudied and undertreated in favor of more invasive technologies. In fact, over 200 years after John Hunter first described the anatomic organs that contributed to semen, we still know surprisingly little about ejaculatory physiology and pathophysiology (1).
Ejaculatory disorders are very common, but are also very commonly misdiagnosed or disregarded (2). Accurate diagnosis of ejaculatory disorders is essential in the evaluation of the infertile male to avoid unnecessary treatment and expense associated with surgical sperm retrieval. Retrograde ejaculation and failure of emission comprise a constellation of disorders with common consequences, but unique and varied pathophysiology and therapeutic strategies. In this review we cover normal ejaculatory physiology, pathophysiology, as well as medical and surgical treatments for these conditions.
Physiology of ejaculation
Ejaculation involves the forcible ejection of seminal fluid from the urethral meatus, which accompanies sexual climax and orgasm. Ejaculation, however, is not be confused with orgasm. Orgasm is a central nervous system phenomenon and is a distinct entity from ejaculation characterized by sensations experienced at the peak of sexual arousal. Orgasm is a purely cerebral and emotional cortical occurrence, though in normal male physiology, orgasm coincides with ejaculation. But nonetheless, even in the published literature and among experts, there seems to oftentimes be confusion between these two terms. In this review, we will discuss ejaculation, which is comprised of two separate phases: emission and expulsion.
Emission
Emission is a physiologic process involving the distal epididymis, the vas deferens, the seminal vesicles, the prostate gland, the prostatic urethra, and the bladder neck. The initial step in emission is closure of the bladder neck mediated by innervation from the sympathetic nervous system. This is followed by deposition and admixture of seminal vesicle, prostatic, vas deferens, and Cowper’s glands secretions into the prostatic urethra. The seminal vesicle secretions are basic and contain fructose, which provides energy for sperm motility. In addition, semenogelin is secreted by the seminal vesicles, which is responsible for coagulation of semen after ejaculation. The spermatozoa come from the vas deferens contribution to the ejaculate. The prostatic secretions are acidic and contain serine proteases (such as PSA) that help liquefy the coagulated semen in the female reproductive tract. In all, the seminal vesicles contribute 65-75% of the ejaculate volume, the prostate contributes roughly 25-30%, vasal fluid supplies 5-10%, and finally bulbourethral glands contribute less than 1% of the total ejaculate volume (Table 1) (3,4).
The neural control of emission originates from the thoracolumbar spine at T10-L2, and coordinates the actions of emission. The sympathetic efferent fibers coalesce into the lumbar sympathetic trunk ganglia, and then proceed posterior to the vena cava into the interaortocaval space on the right and lateral to the aorta on the left. Continuing inferiorly, the sympathetic efferent fibers from the right and left merge to form the superior hypogastric plexus anterior to L5 and the sacrum. Postganglionic fibers travel to their target organs: bladder neck, prostate, seminal vesicles, and vas deferens to mediate sympathetic control of the emission phase of ejaculation, and thus far a specific role for the parasympathetic nervous system has not been elucidated (6,7).
Expulsion
Following emission, expulsion occurs and involves the coordinated rhythmic action of the bladder neck, external urethral sphincter, urethra, and bulbospongiosus and pelvic striated muscle to propel semen through the urethra and out the meatus. Expulsion is mediated by the somatic nervous system; the external urethral sphincter relaxes, followed by clonic contractions of the prostate, bulbocavernosus muscle, ischiocavernosus, levator ani, and transverse perineal muscles (8-10).
The neuroanatomic control of expulsion is dependent on a reflex arc in the spinal cord. These neural pathways are arranged in reflex circuits responsible for mediating expulsion by eliciting bulbospongiosus contraction, relaxation of the external sphincter, and coordinated contractions of the prostate and seminal vesicles (11). The sensory input involves the perineal branch of the pudendal nerve receiving signals from two diverging sets of nerve fibers (one along the dorsolateral aspect of the penis innervating the shaft and glans and the second from the ventrolateral portion of the penis innervating the urethra). The sensory axons of the afferent pernineal nerve then synapse on the pudendal motor neurons in the nucleus of Onuf as well as on to spinal interneurons that communicate with the thoracolumbar spinal cord (T10-L2) to trigger emission. The efferent portion of the circuit exits the spinal cord via the perineal nerve to terminate on muscle fibers of the bulbospongiosus muscle for somatic reflex control of these muscles leading to ejaculation (12).
Neurotransmitters
Although the exact mechanisms have yet to be elucidated, a brief review of the role that neurotransmitters play in ejaculatory physiology is worthwhile as psychotropic medications are commonly implicated in a variety of ejaculatory complaints.
Serotonin
Overall, it is thought that serotonin exerts an inhibitory effect on ejaculation in humans. In animal studies, serotonin seems to have inhibitory effects in the CNS, while excitatory effects predominate in the PNS (13,14). There are a variety of serotonin receptors divided into seven different classes, 5-HT1-7, located ubiquitously across the central and peripheral nervous systems. Of these, receptors 5-HT1A, 5-HT1B, and 5-HT2C are most strongly linked to ejaculatory function. Serotonin receptors have been identified in the expected locations such as the brain stem, hypothalamus, and spinal cord, as well as ejaculatory structures including the prostate, seminal vesicles, vas deferens, and urethra (15-17). Although first discovered as an incidental observation, serotonin reuptake inhibitors (SSRI) commonly used in the medical treatment of premature ejaculation, clinically demonstrate the inhibitory effect of serotonin (18,19).
Dopamine
Animal models have confirmed the excitatory role dopamine plays in sexual behavior and ejaculation, a phenomenon first observed in Parkinson’s patients treated with L-DOPA (20,21). Not only did Parkinson’s patients experience resolution of their motor symptoms, but also reported hypersexuality with more frequent masturbation, sexual hallucinations, and increased nocturnal erections (20). Specifically, a rat study demonstrated the D2 receptor mediates the excitatory effects of dopamine: in the presence of a D2 receptor antagonist, a known dopamine and serotonin receptor agonist lost its stimulatory effects on ejaculation (21). These biochemical findings further correlate with clinical findings of ejaculatory delay in patients treated with dopaminergic antagonists for schizophrenia or anxiety (22,23). Dopamine antagonists such as haloperidol, thioridazine, and sulpiride have been found to delay ejaculation (24-26).
Pathophysiology
Retrograde ejaculation and failure of emission are the two disorders of ejaculatory function which result in anejaculation and infertility. While all three have a common pathway of anejaculation, the disorders leading to these conditions comprise a heterogeneous group of conditions with differing etiologies and therapies. A full history and physical as well as necessary hormonal evaluation may lead to the correct diagnosis.
Evaluation
History is essential in the evaluation of disorders of ejaculation. A focused history about ability to achieve orgasm versus anejaculation will determine if it is caused by anorgasmia. Patients should be asked about situational factors, which may be affecting ejaculation. Also, nocturnal emissions should be questioned. A detailed pharmacologic, sexual, medical, and surgical history will all aid in the correct diagnosis. Sign and symptoms of hypogonadism (i.e., low energy, low libido), erectile dysfunction, diabetes (i.e., polyuria), psychiatric illness (i.e., depression), and neurological disease (i.e., sensory abnormalities, bowel or bladder dysfunction) may aid in the diagnosis of ejaculatory dysfunction.
A thorough history of a patient with an ejaculatory complaint, with special attention to chronicity, answers the question of congenital versus acquired ejaculatory dysfunction. Important considerations include the patient’s ability to achieve climactic satisfaction and the presence of any situational variability. These questions may establish a disorder of sexual desire or arousal, and steer away from a disorder driven by ejaculatory pathophysiology.
A complete physical exam with special attention to signs of hypogonadism (atrophic testes, undeveloped phallus), thyroid disorders, other endocrinopathies (gynecomastia), abnormal penile sensation (abnormalities in penile or scrotal development) and signs of diabetic neuropathy (impaired peripheral sensation, obesity) can provide important guidance towards the correct diagnosis. When appropriate, laboratory evaluations of FSH, testosterone, HbA1c, TSH and prolactin levels can further inform on the etiology of the patient’s condition. Post-orgasm urinalysis may also be useful in identifying whether retrograde ejaculation is present.
Retrograde ejaculation
Retrograde ejaculation is the flow of semen into the bladder due to an incompletely closed bladder neck. In two large series of azoospermic men, retrograde ejaculation was the observed cause in 18%, although as a source of infertility it was only implicated in 0.7% (19,20). Additionally, it has been noted the incidence is likely rising as a consequence increasing rates of diabetes, use of α-receptor antagonists, and bladder neck surgery for malignancies (21). This diagnosis is easily confirmed with identification of sperm in a post-masturbatory voided sample. A variety of mechanical, neurologic, and pharmacologic etiologies are responsible for retrograde ejaculation.
Etiology
Surgical injury
Instrumentation and surgery is the most common cause of an incompetent bladder neck, with a majority of men experiencing retrograde ejaculation after transurethral resection of the prostate (27). Lower rates of men experience this side effect when their prostate disease is treated with transurethral microwave therapy or transurethral incision of the prostate, which may argue for these options to be considered in younger men or those with good baseline sexual function (28,29). But no procedure on the prostate is without risk of retrograde ejaculation and men considering surgery who still desire children should be adequately counseled regarding the side-effects of these procedures.
Surgical injury to the nerves influencing ejaculatory function also carry the risk of retrograde ejaculation with the most common being retroperitoneal surgeries, colorectal surgery, and spine surgery (30,31). Development of nerve-sparing retroperitoneal lymph node dissection (RPLND) techniques and templates have made this mainstay of testicular cancer therapy less damaging to patients’ ejaculatory function (32).
Diabetic complications
Retrograde ejaculation is both common and under-recognized in diabetic men, with one series reporting a prevalence of 32% (33). Chronic uncontrolled diabetes results in an autonomic neuropathy that disrupts the sympathetic output to the bladder neck, impairing its ability to close during ejaculation. Similar to erectile complaints, patient reported ejaculatory problems should heighten the clinician’s concern for additional vascular or neurologic pathology.
Pharmacologic disruptors
Pharmacologic treatment for a variety of conditions can induce retrograde ejaculation in men, with the most common offenders being alpha-receptor antagonists for lower urinary tract symptoms, other sympatholytics for hypertension, antidepressants, and antipsychotics. However, investigators have recently proposed that perhaps the ejaculatory disorder induced in men taking alpha antagonists may be due to a contractility of the seminal vesicles, not retrograde ejaculation caused by disrupted closure of the bladder neck. In the laboratory they demonstrated a high prevalence of alpha-1 receptor subtypes in the seminal vesicles, and correspondingly from the clinical side, showed healthy men taking tamsulosin had lower volume ejaculate than controls and no sperm was present in their post-ejaculate void (34). Fascinatingly, this may imply that alpha-blockers may have more reproductive effects than previously recognized and not simply affect the bladder neck, though more studies are needed to confirm this interesting finding.
Treatment
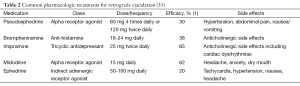
The goal for treatment of patients with RE is to restore antegrade ejaculation of semen for attempts at natural conception as well as collection of sperm for assisted reproductive techniques. When possible, the offending medication should be discontinued if the benefit of resolved retrograde ejaculation outweighs the benefit the medication provides. In cases of neuropathy-induced, iatrogenic, or idiopathic retrograde ejaculation, sympathomimetic drugs have had the most, albeit modest, success. The mechanism of sympathomimetic action is to improve bladder neck contraction during the expulsive phase of ejaculation. These include ephedrine sulfate, imipramine hydrochloride, midodrine hydrochloride, brompheniramine maleate, and pseudoephedrine hydrochloride (Table 2) [for review, see (35)]. Imipramine is the preferred agent with high success rates in patients who have undergone retroperitoneal sympathetic denervation (36). A recent review of the literature reports treatment with sympathomimetics resulted in restoration of antegrade ejaculation in only 28% of subjects (37).
If the goal of treatment is to harvest sperm for use with assisted reproductive techniques, then sperm can be used either from the converted antegrade ejaculate or from harvesting of post-orgasm bladder samples. Generally, before harvest of bladder samples, sodium bicarbonate (50 mg) is given 12 and 2 hours prior to collection. This alkalinization of the urine minimizes the toxic effect of acidic urine on sperm quality. The patient is asked to void (or atraumatically catheterized if unable to void) just before orgasm to minimize urine volume. After orgasm, the voided (or catheterized) urine is collected and centrifuged to be used for assisted reproductive techniques. In a systematic review, Jefferys et al., examined fifteen studies using a variety of artificial insemination techniques with the obtained sperm [intrauterine insemination (IUI), IVF, and ICSI]. Overall, pregnancy rate per cycle was 15%, with a live birth rate of 14% (37).
Failure of emission
Etiology
Failure of emission is when there is complete disruption of emission during sexual activity. Orgasm and the expulsive phase of ejaculation occur, but there is failure of deposition of the reproductive glands to deposit the necessary fluid into the prostatic urethra during stimulation. It is clinically characterized simply as anejaculation, but on investigation for retrograde ejaculation, there will be no evidence of retrograde ejaculation in post-orgasm urine. Failure of emission is defined as the lack of sperm on antegrade and retrograde semen analysis. This can be caused by peripheral neuropathy caused by diabetes as well as any spinal cord injury (SCI). Basically, we view failure of emission and retrograde ejaculation as a spectrum of ejaculatory dysfunction with failure of emission being the ultimate failure of the ejaculatory system.
Treatment
Assisted ejaculation procedures are used to harvest sperm for assisted reproduction in anorgasmic and anejaculatory men. While sperm can by surgically retrieved from any portion of the reproductive tract (testis, epididymis, vas, or seminal vesicles) and used for IVF-ICSI, in the patient with ejaculatory failure, treatment of the ejaculatory dysfunction results in much higher yields of sperm. The two most commonly used techniques are penile vibratory stimulation (PVS) and electroejaculation (EEJ). Overall, studies show that sperm can be retrieved by PVS or EEJ in 97% of SCI men (38).
Penile vibratory stimulation (PVS)
PVS refers to the use of a vibrator applied to the penis to induce ejaculation. The vibrator is generally applied to the frenular surface of the glans and the resulting ejaculated sperm can be used in assisted reproduction for those patients with psychogenic anejaculation as well as SCI above the T12 level. The success use of PVS in the SCI patient depends on an intact spinal cord ejaculatory reflex arc (sensory nerves, spinal cord S2-S4 arc, and efferent nerves) as well as lack of descending cortical inhibitory input (12). Any sperm harvested by PVS can be used in IUI, IVF, and IVF-ICSI (39). PVS is a cost effective treatment and easy procedure for patients that can be done at home with subsequent home vaginal insemination (40).
The ideal candidate for PVS has a high SCI, above T10, and highest PVS rates are seen in patients with C3-C7 injuries (41,42). Though even simple vibrators without adjustable frequency and amplitude may be effectively used, the optimal setting seems to be 1.0-2.5 mm amplitude and 100 Hz frequency (43). Even if initially unsuccessful, 20% may respond to addition of a second vibrator (44). Also, midodrine may be used as an adjunct for PVS in patients who have already failed a single round of PVS (45). Possible side effects of PVS include abrasions of the penile skin and autonomic dysreflexia in at-risk spinal cord injured men. Men at risk for autonomic dysreflexia should be treated with a prophylactic dose of nifedipine (10-20 mg) prior to the procedure. If there are signs of autonomic dysreflexia, the vibratory stimulation should be removed immediately.
Rectal probe electrostimulation
If efforts to restore antegrade flow or PVS fail, then rectal probe electrostimulation or EEJ can be used. It is a generally more invasive procedure in which a rectal probe electrode is used to deliver electrical current directly to the prostate and seminal vesicles, resulting in ejaculation (see Figure 1). Patients who have SCI who are insensate below the waste can undergo this in the office setting, but men who are sensate below the waist will require general anesthesia. Prior to the procedure, the urine should be alkalinized with sodium citrate, potassium citrate, or IV bicarbonate as urine’s acidity and osmolarity is toxic to sperm. The patient is generally catheterized first to empty the bladder and 20-30 cc of sperm transport media [we use human tubal fluid (HTF) buffered with HEPES and plasmanate, pH 7.4] are then instilled into the bladder. Care should be taken to avoid urethral trauma as contact with blood can impact sperm quality. Mineral oil is preferred over water-based lubricants for the catheterization due to toxic effects on sperm (46,47).
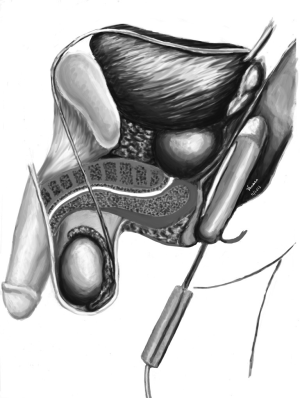
The patient is then repositioned in the lateral decubitus position and rectoscopy is performed to identify any mucosal ulceration, rectal mass, or full rectal vault that may preclude the EEJ procedure. The rectal probe is then inserted and the electrodes are oriented towards the prostate and seminal vesicles. Using a Seager Electoejaculator© a peaked sine wave pattern of electrical energy is applied to the prostate with increasing amplitude until either antegrade semen flow is seen, rectal temperature reaches 38 degrees Celsius, or the 30 volt maximum is reached. Also, with the lower end of the stimulation, we do not completely stop the current to avoid spasticity in the patient. We generally note the voltage and number of stimulations necessary to reach ejaculation in the medical record in case repeat EEJ is needed. As rectal mucosal injury is a potential complication, anoscopy is again performed. The patient is then placed supine and catheterized for the retrograde sample. The initial retrograde and antegrade sample is diluted in HTF buffered with HEPES and plasmanate, pH 7.4 and sent for immediate processing.
Autonomic dysreflexia is also a potential complication in men with spinal cord injuries above T6 undergoing EEJ. Precautions should be taken to monitor blood pressure in any procedure involving hollow visceral dilation or neurologic stimulation of the lower reproductive tract. Prophylactic nifedipine prior to electrical stimulation is also recommended in those with history of autonomic dysreflexia or at high risk for it. If it does occur, the stimulation should be immediately withdrawn.
Sperm quality
While PVS and EEJ are well defined in terms of their ability to obtain ejaculate, which form of assisted reproduction is necessary depends on a number of both male and female factors. Obviously, the quality and quantity of sperm collected determines whether it can be used for IUI or ICSI. Ohl et al. has shown an 8.7% per cycle fecundity over 653 cycles of EEJ with IUI with a median of 3 IUI cycles to reach pregnancy (48). Chung et al. reported a fertilization rate of 75% per injected oocyte and clinical pregnancy rate of 55% per fresh semen retrieval attempt when ICSI was coupled to EEJ (49).
A few points should be kept in mind when recommending assisted ejaculation procedures SCI patients. Although there are few differences in sperm quality between PVS and EEJ, both have higher DNA fragmentation rates than normal controls (50). Also, SCI patients have worse outcomes when compared to non-SCI patients with lower fertilization rates. However, sperm collected by PVS and EEJ in SCI men demonstrate similar pregnancy and live birth rates using IVF-ICSI (51). What causes this difference is still an area of active research, though recent work has indicated that the inflammatory factors may play a role in the decreased sperm quality seen in the ejaculate of SCI men (52).
Special considerations: anejaculation following PC-RPLND
Though much of this literature deals with SCI injury patients and patients with diabetic neuropathy, there is a subset of patients that merit special discussion. These are testis cancer patients that have undergone orchiectomy, chemotherapy, and RPLND, rendering them anejaculatory even with nerve sparing techniques. In this unique set of patients, there are disorders of ejaculation as well as threats to sperm production since they were given chemotherapy. Hsiao et al. performed a study where a structured clinical protocol was applied to 26 men seeking fertility who presented to a quaternary cancer referral center with anejaculation after post-chemotherapy RPLND. In this study, 50% of men with RE converted to antegrade ejaculation with medical therapy. No men with failure of emission had conversion to antegrade ejaculation with medication. In those with failure of emission, EEJ was successful in 91% of men, and sperm was found in 75% of these men. The rest underwent testicular sperm extraction. In conclusion, for men with anejaculation after post-chemotherapy RPLND, we recommend men with retrograde ejaculation undergo a trial of medication to convert retrograde to antegrade ejaculation. If medications fail we proceed to EEJ and if no sperm or poor quality is seen on EEJ, we go to testicular sperm extraction and assisted reproductive techniques. In those patients with failure of emission, we recommend proceed immediately to EEJ, and if inadequate or poor quality sperm is seen on EEJ, proceed directly with testicular sperm extraction in the same setting under general anesthesia (53).
Conclusions
Ejaculatory dysfunction resulting in azoospermia can be due to retrograde ejaculation or failure of emission. A careful and focused history, physical exam, and appropriate diagnostic tests will lead to the correct diagnosis. Treatment decisions are informed by etiology and patients’ goals of care, and for those men desiring fertility, there are a wide range of efficacious options to reach this objective.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hendry WF. Disorders of ejaculation. Ann R Coll Surg Engl 1999;81:352-8. [PubMed]
- Althof SE. Prevalence, characteristics and implications of premature ejaculation/rapid ejaculation. J Urol 2006;175:842-8. [PubMed]
- Polakoski KL, Syner FN, Zaneveld LJ. Biochemistry of human seminal plasma. In: Hafez ES. eds. Human semen and fertility regulation in men. St. Louis: Mosby, 1976:133-43.
- Mann T, Lutwak-Mann C. eds. Male reproductive function and semen: themes and trends in physiology, biochemistry, and investigative andrology. Berlin/New York: Springer-Verlag, 1981.
- Coffey D. What is the prostate and what is its function? In: Robaire B, Pryor JL, Trasler JM, eds. Handbook of Andrology. Lawrence, KS: Allen Press, 1995:21-4.
- Giuliano F, Clement P. Neuroanatomy and physiology of ejaculation. Annu Rev Sex Res 2005;16:190-216. [PubMed]
- Lipshultz LI, Howards SS, Niederberger CS. Infertility in the male. 4th ed. Cambridge: Cambridge University Press, 2009.
- Yang CC, Bradley WE. Somatic innervation of the human bulbocavernosus muscle. Clin Neurophysiol 1999;110:412-8. [PubMed]
- Gerstenberg TC, Levin RJ, Wagner G. Erection and ejaculation in man. Assessment of the electromyographic activity of the bulbocavernosus and ischiocavernosus muscles. Br J Urol 1990;65:395-402. [PubMed]
- Vaucher L, Bolyakov A, Paduch DA. Evolving techniques to evaluate ejaculatory function. Curr Opin Urol 2009;19:606-14. [PubMed]
- Yang CC, Bradley WE. Innervation of the human anterior urethra by the dorsal nerve of the penis. Muscle Nerve 1998;21:514-8. [PubMed]
- Wieder JA, Brackett NL, Lynne CM, et al. Anesthetic block of the dorsal penile nerve inhibits vibratory-induced ejaculation in men with spinal cord injuries. Urology 2000;55:915-7. [PubMed]
- Chan JS, Snoeren EM, Cuppen E, et al. The serotonin transporter plays an important role in male sexual behavior: a study in serotonin transporter knockout rats. J Sex Med 2011;8:97-108. [PubMed]
- Ishigami T, Yoshioka K, Karicheti V, et al. A Role for Peripheral 5-HT Receptors in Serotonin-Induced Facilitation of the Expulsion Phase of Ejaculation in Male Rats. J Sex Med 2013;10:2688-702. [PubMed]
- Azmitia E, Gannon P. The ultrastructural localization of serotonin immunoreactivity in myelinated and unmyelinated axons within the medial forebrain bundle of rat and monkey. J Neurosci 1983;3:2083-90. [PubMed]
- Descarries L, Beaudet A, Watkins KC. Serotonin nerve terminals in adult rat neocortex. Brain Res 1975;100:563-88. [PubMed]
- Kim SW, Paick JS. Peripheral effects of serotonin on the contractile responses of rat seminal vesicles and vasa deferentia. J Androl 2004;25:893-9. [PubMed]
- Montague DK, Jarow J, Broderick GA, et al. AUA guideline on the pharmacologic management of premature ejaculation. J Urol 2004;172:290-4. [PubMed]
- McMahon CG, Abdo C, Incrocci L, et al. Disorders of orgasm and ejaculation in men. J Sex Med 2004;1:58-65. [PubMed]
- Gessa GL, Tagliamonte A. Role of brain monoamines in male sexual behavior. Life Sci 1974;14:425-36. [PubMed]
- Clément P, Bernabé J, Kia HK, et al. D2-like receptors mediate the expulsion phase of ejaculation elicited by 8-hydroxy-2-(di-N-propylamino)tetralin in rats. J Pharmacol Exp Ther 2006;316:830-4. [PubMed]
- Compton MT, Miller AH. Sexual side effects associated with conventional and atypical antipsychotics. Psychopharmacol Bull 2001;35:89-108. [PubMed]
- Peeters M, Giuliano F. Central neurophysiology and dopaminergic control of ejaculation. Neurosci Biobehav Rev 2008;32:438-53. [PubMed]
- Baggaley M. Sexual dysfunction in schizophrenia: focus on recent evidence. Hum Psychopharmacol 2008;23:201-9. [PubMed]
- Cutler AJ. Sexual dysfunction and antipsychotic treatment. Psychoneuroendocrinology 2003;28 Suppl 1:69-82. [PubMed]
- Teusch L, Scherbaum N, Bohme H, et al. Different patterns of sexual dysfunctions associated with psychiatric disorders and psychopharmacological treatment. Results of an investigation by semistructured interview of schizophrenic and neurotic patients and methadone-substituted opiate addicts. Pharmacopsychiatry 1995;28:84-92. [PubMed]
- Rassweiler J, Teber D, Kuntz R, et al. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol 2006;50:969-79. [PubMed]
- Hoffman RM, Monga M, Elliott SP, et al. Microwave thermotherapy for benign prostatic hyperplasia. Cochrane Database Syst Rev 2012;9:CD004135. [PubMed]
- de Paula F, Donadio D, Lauretti S, et al. Transurethral incision of prostate (TUIP) and retrograde ejaculation. Arch Ital Urol Androl 1997;69:163-6. [PubMed]
- Tiusanen H, Seitsalo S, Osterman K, et al. Retrograde ejaculation after anterior interbody lumbar fusion. Eur Spine J 1995;4:339-42. [PubMed]
- Nesbakken A, Nygaard K, Bull-Njaa T, et al. Bladder and sexual dysfunction after mesorectal excision for rectal cancer. Br J Surg 2000;87:206-10. [PubMed]
- Donohue JP, Foster RS. Retroperitoneal lymphadenectomy in staging and treatment. The development of nerve-sparing techniques. Urol Clin North Am 1998;25:461-8. [PubMed]
- Dunsmuir WD, Holmes SA. The aetiology and management of erectile, ejaculatory, and fertility problems in men with diabetes mellitus. Diabet Med 1996;13:700-8. [PubMed]
- Hisasue S, Furuya R, Itoh N, et al. Ejaculatory disorder caused by alpha-1 adrenoceptor antagonists is not retrograde ejaculation but a loss of seminal emission. Int J Urol 2006;13:1311-6. [PubMed]
- Kamischke A, Nieschlag E. Update on medical treatment of ejaculatory disorders. Int J Androl 2002;25:333-44. [PubMed]
- Nijman JM, Jager S, Boer PW, et al. The treatment of ejaculation disorders after retroperitoneal lymph node dissection. Cancer 1982;50:2967-71. [PubMed]
- Jefferys A, Siassakos D, Wardle P. The management of retrograde ejaculation: a systematic review and update. Fertil Steril 2012;97:306-12. [PubMed]
- Brackett NL, Ibrahim E, Iremashvili V, et al. Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J Urol 2010;183:2304-8. [PubMed]
- Sønksen J, Sommer P, Biering-Sørensen F, et al. Pregnancy after assisted ejaculation procedures in men with spinal cord injury. Arch Phys Med Rehabil 1997;78:1059-61. [PubMed]
- Kathiresan AS, Ibrahim E, Aballa TC, et al. Pregnancy outcomes by intravaginal and intrauterine insemination in 82 couples with male factor infertility due to spinal cord injuries. Fertil Steril 2011;96:328-31. [PubMed]
- Bird VG, Brackett NL, Lynne CM, et al. Reflexes and somatic responses as predictors of ejaculation by penile vibratory stimulation in men with spinal cord injury. Spinal Cord 2001;39:514-9. [PubMed]
- Brackett NL, Ferrell SM, Aballa TC, et al. An analysis of 653 trials of penile vibratory stimulation in men with spinal cord injury. J Urol 1998;159:1931-4. [PubMed]
- Sønksen J, Biering-Sørensen F, Kristensen JK. Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. The importance of the vibratory amplitude. Paraplegia 1994;32:651-60. [PubMed]
- Brackett NL, Kafetsoulis A, Ibrahim E, et al. Application of 2 vibrators salvages ejaculatory failures to 1 vibrator during penile vibratory stimulation in men with spinal cord injuries. J Urol 2007;177:660-3. [PubMed]
- Soler JM, Previnaire JG, Plante P, et al. Midodrine improves ejaculation in spinal cord injured men. J Urol 2007;178:2082-6. [PubMed]
- Agarwal A, Deepinder F, Cocuzza M, et al. Effect of vaginal lubricants on sperm motility and chromatin integrity: a prospective comparative study. Fertil Steril 2008;89:375-9. [PubMed]
- Anderson L, Lewis S, McClure N. The effects of coital lubricants on sperm motility in vitro. Hum Reprod 1998;13:3351-6. [PubMed]
- Ohl DA, Wolf LJ, Menge AC, et al. Electroejaculation and assisted reproductive technologies in the treatment of anejaculatory infertility. Fertil Steril 2001;76:1249-55. [PubMed]
- Chung PH, Palermo G, Schlegel PN, et al. The use of intracytoplasmic sperm injection with electroejaculates from anejaculatory men. Hum Reprod 1998;13:1854-8. [PubMed]
- Restelli AE, Bertolla RP, Spaine DM, et al. Quality and functional aspects of sperm retrieved through assisted ejaculation in men with spinal cord injury. Fertil Steril 2009;91:819-25. [PubMed]
- Kathiresan AS, Ibrahim E, Aballa TC, et al. Comparison of in vitro fertilization/intracytoplasmic sperm injection outcomes in male factor infertility patients with and without spinal cord injuries. Fertil Steril 2011;96:562-6. [PubMed]
- Zhang X, Ibrahim E, de Rivero Vaccari JP, et al. Involvement of the inflammasome in abnormal semen quality of men with spinal cord injury. Fertil Steril 2013;99:118-24. [PubMed]
- Hsiao W, Deveci S, Mulhall JP. Outcomes of the management of post-chemotherapy retroperitoneal lymph node dissection-associated anejaculation. BJU Int 2012;110:1196-200. [PubMed]