
Age ≤40 is an independent predictor of anastomotic urethroplasty and successful repair of bulbar urethral strictures
Introduction
Urethral stricture disease is a heterogenous entity that can afflict men at any stage of life (1,2). Endoscopic management has traditionally been the mainstay of urethral stricture treatment due to ease of urethral dilation, but multiple studies have demonstrated that urethral dilation is neither clinically nor cost-effective (3-5). Additionally, self-dilation to maintain urethral patency has been associated with poor quality of life, especially in younger men (6). Since the superiority of urethroplasty relative to dilation in the management of urethral stricture disease is now well-established (3), understanding factors that contribute to urethroplasty success or failure is a topic of active research.
Many studies have evaluated urethroplasty outcomes in the context of stricture characteristics, such as location and length, and underlying patient co-morbidities. Several have recently investigated advanced age as a predictor of urethroplasty outcomes for both anastomotic and substitution repairs. The Trauma and Urologic Reconstructive Network of Surgeons (TURNS) recently found similar outcomes from urethroplasty regardless of age, with greater than 90% success amongst older patients at one year (7). We have previously reported outcomes for older men undergoing urethroplasty and found that at 5 years, greater than 70% remained stricture-free (8). Together, these findings support that urethroplasty can be performed safely and effectively in elderly men with appropriate patient and procedural selection.
We hypothesize that younger men fare better than older patients following urethral reconstruction in our tertiary referral practice. We postulate that this may be due more favorable tissue characteristics, such as increased androgen induced vascularity. Additionally, we suspect that younger men tend to have different stricture etiology compared to older men, creating a distinct milieu for reconstruction. We surmise that younger men present for reconstruction more efficiently and with fewer prior endoscopic interventions compared to older men, simplifying their eventual repair. In this study, we set out to evaluate outcomes in our younger patients undergoing urethroplasty and identifying factors which may influence outcomes from reconstruction.
Methods
After institutional review board approval, we performed a retrospective medical record review of all patients who underwent urethroplasty at our tertiary referral center by a single reconstructive urologist from 2007 to 2017. Patients who had bulbar urethral stricture disease were identified and age-stratified into cohorts ≤40 and >40 years old. Demographic, clinical, operative, and outcomes data were analyzed by urethroplasty database and electronic medical record (EMR) review. Urethroplasty success was defined by functional emptying and lack of need for further endoscopic or open re-operative management. Parameters correlated with urethroplasty failure were included in multivariate logistic regression models.
Statistical analysis
The Wilcoxon rank sum test was used to determine differences in success rates between the two age groups. A multivariable logistic regression model was used to test for significant predictors of urethroplasty failure. All analyses were carried out using JMP™ by SAS (Cary, NC, USA).
Results
Clinical Characteristics
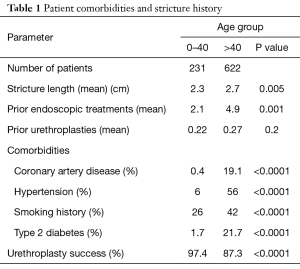
Over the study period, 853 men who underwent bulbar urethroplasty were identified. Of these men, 231 (27.1%) were age 40 or younger and 622 (72.9%) were older than 40. The overall median age was 53.1 years old, with median ages 29.6 years and 60.2 years in the younger and older groups, respectively. Younger men presented with fewer co-morbidities that predispose to poor vascularity and tissue healing compared to older men (Table 1) [Diabetes (1.7% vs. 21.7%, P<0.0001), coronary artery disease (0.4% vs. 19.1%, P<0.0001), and erectile dysfunction (11.5% vs. 29.2%, P<0.0001)].
Full table
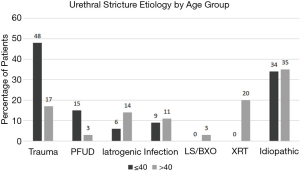
There was no significant difference in the number of prior urethroplasty procedures between the two groups (Table 1). However, older men presented for reconstruction with a significantly greater number of prior endoscopic treatments (2.1 vs. 4.9, P=0.001) and had a longer mean stricture length compared to younger men (2.7 vs. 2.3 cm, P=0.005). Traumatic etiology was more commonly found in the younger group, whereas older men were more likely to have iatrogenic strictures (Figure 1). Excision and primary anastomosis were the most commonly used reconstructive technique in both groups but was utilized less frequently in older men (77% in >40 group vs. 87% ≤40 group, P=0.0009).
Urethroplasty outcomes
Operative success—defined as functional voiding without the need for additional intervention—in our overall cohort was 88.9%. When stratified into two age groups, younger men had significantly better urethroplasty success (97.4%) compared to older men (87.3%, P<0.0001) over a median follow-up of 52.4 months (Table 1).
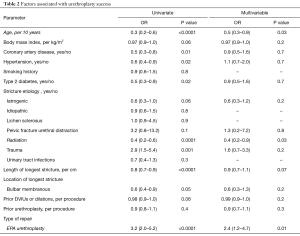
On logistic regression analysis, multiple parameters were evaluated as possible predictors of urethroplasty success. On multivariate analysis, younger age was a significant predictor of urethroplasty success. Other factors associated with success following urethroplasty include usage of EPA and absence of pelvic radiation (Table 2).
Full table
Discussion
In this study we present our cumulative decade long tertiary referral center experience with bulbar urethroplasty, focusing on outcomes among younger patients undergoing urethral reconstruction. We found that men under 40 years old had improved outcomes after urethroplasty compared to older men despite the finding that younger men more commonly presented with traumatic strictures (as opposed to iatrogenic or radiation-induced strictures seen in older men). Finally, we found that anastomotic urethroplasty predicted better outcomes compared with substitution techniques.
Older men in our study were treated with a greater number of repeated endoscopic procedures for urethral stricture compared to younger men before presenting for definitive reconstruction. Endoscopic management has traditionally been the mainstay of urethral stricture treatment due to ease of urethral dilation or urethrotomy. However, in 2016, the American Urological Association published treatment guidelines for the management of urethral stricture disease, which recommended against repeated endoscopic procedures for stricture disease (9). Men undergoing repeated urethrotomy are not only subject to failure rates as high as 80% but also develop worsened stricture disease (4). We previously reported that men who had undergone more than two transurethral treatments for bulbar strictures presented with longer strictures (mean 3.68 vs. 2.20 cm, P=0.001) and were more likely to require substitution urethroplasty (OR 5.1, 95% CI 1.9–14.2) (3). In the present study, older men were found to have significantly longer strictures, likely because of this greater history of endoscopic intervention. Furthermore, younger men probably had more favorable tissue characteristics due, in part, to less trauma from transurethral procedures than older patients, likely contributing to improved urethroplasty outcomes.
In recent years, several groups have evaluated outcomes of urethroplasty in older men. In 2017, the TURNS group reported on their multi-institutional experience with urethroplasty in men over 60 (7). In a one-year follow-up period, they found no significant difference in outcomes between older and younger men undergoing urethroplasty. However, this study excluded patients with a history of radiation, potentially improving the apparent rate of urethroplasty success in the older population.
Older men have a higher rate of co-morbidities which may predispose to poor reconstructive outcomes. Diabetes and coronary artery disease have well-demonstrated adverse effects on both peripheral vasculature and erectile function (10,11). Recent histopathologic findings from men undergoing urethral stricture repair suggest that hypogonadal men have impaired periurethral vascularity resulting from loss of androgen receptor expression (8,12). A number of studies have demonstrated changes in serum testosterone levels with advancing age, with an annual decline of 1–2 (13,14). By the age of 60, approximately 30–40% of men are hypogonadal based on serum assays (15). While serum testosterone levels were not assessed in our study, it is likely that the older cohort (median age 60.2 years) had a higher prevalence of low serum testosterone compared to the younger men (median age 29.6 years); however, this should be assessed more completely in future research as this was a limitation of our study.
In our series, younger men had a lower prevalence of radiation-induced strictures compared to their older counterparts. Radiation induces vascular damage and fibrosis of the urethra and corpus spongiosum which results in more complex stricture disease and reconstruction (16,17). Pelvic radiation often results in obliterative strictures in the bulbomembranous urethra and are best repaired in anastomotic fashion (18). In our recent evaluation of a decade of experience in managing radiation-induced strictures, we found recurrence in 36.6% of patients (19). This failure rate is significantly higher than the expected for anastomotic urethroplasty, underscoring the important role of stricture etiology in urethroplasty outcomes.
Conclusions
Bulbar strictures in younger men have higher urethroplasty success rates compared to urethral reconstruction in men over the age of 40. Bulbar strictures in this younger population are likely to be traumatic in origin and more amenable to anastomotic reconstruction.
Acknowledgments
None.
Footnote
Conflicts of Interest: Dr. Allen F. Morey receives honoraria for being a guest lecturer/meeting participant for Boston Scientific and Coloplast Corp. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of The University of Texas Southwestern Medical Center at Dallas. (ID: 102012-021).
References
- Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol 2007;177:1667-74. [Crossref] [PubMed]
- Lumen N, Hoebeke P, Willemsen P, et al. Etiology of urethral stricture disease in the 21st century. J Urol 2009;182:983-7. [Crossref] [PubMed]
- Hudak SJ, Atkinson TH, Morey AF. Repeat transurethral manipulation of bulbar urethral strictures is associated with increased stricture complexity and prolonged disease duration. J Urol 2012;187:1691-5. [Crossref] [PubMed]
- Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: long-term followup. J Urol 1996;156:73-5. [Crossref] [PubMed]
- Lacy JM, Cavallini M, Bylund JR, et al. Trends in the management of male urethral stricture disease in the veteran population. Urology 2014;84:1506-9. [Crossref] [PubMed]
- Lubahn JD, Zhao LC, Scott JF, et al. Poor quality of life in patients with urethral stricture treated with intermittent self-dilation. J Urol 2014;191:143-7. [Crossref] [PubMed]
- Levy M, Gor RA, Vanni AJ, et al. The Impact of Age on Urethroplasty Success. Urology 2017;107:232-8. [Crossref] [PubMed]
- Viers BR, Pagliara TJ, Rew CA, et al. Urethral Reconstruction in Aging Male Patients. Urology 2018;113:209-214. [Crossref] [PubMed]
- Wessells H, Angermeier KW, Elliott S, et al. Male Urethral Stricture: American Urological Association Guideline. J Urol 2017;197:182-90. [Crossref] [PubMed]
- Feldman HA, Johannes CB, Derby CA, et al. Erectile dysfunction and coronary risk factors: prospective results from the Massachusetts male aging study. Prev Med 2000;30:328-38. [Crossref] [PubMed]
- Ruutu M, Alfthan O, Heikkinen L, et al. "Epidemic" of acute urethral stricture after open-heart surgery. Lancet 1982;1:218. [Crossref] [PubMed]
- Hofer MD, Kapur P, Cordon BH, et al. Low Testosterone Levels Result in Decreased Periurethral Vascularity via an Androgen Receptor-mediated Process: Pilot Study in Urethral Stricture Tissue. Urology 2017;105:175-80. [Crossref] [PubMed]
- Wang C, Nieschlag E, Swerdloff R, et al. ISA, ISSAM, EAU, EAA and ASA recommendations: investigation, treatment and monitoring of late-onset hypogonadism in males. Int J Impot Res 2009;21:1-8. [Crossref] [PubMed]
- Feldman HA, Longcope C, Derby CA, et al. Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab 2002;87:589-98. [Crossref] [PubMed]
- Khera M, Broderick GA, Carson CC 3rd, et al. Adult-Onset Hypogonadism. Mayo Clin Proc 2016;91:908-26. [Crossref] [PubMed]
- Awad MA, Gaither TW, Osterberg EC, et al. Prostate cancer radiation and urethral strictures: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis 2018;21:168-74. [Crossref] [PubMed]
- Matta R, Chapple CR, Fisch M, et al. Pelvic Complications After Prostate Cancer Radiation Therapy and Their Management: An International Collaborative Narrative Review. Eur Urol 2019;75:464-76. [Crossref] [PubMed]
- Fuchs JS, Hofer MD, Sheth KR, et al. Improving Outcomes of Bulbomembranous Urethroplasty for Radiation-induced Urethral Strictures in Post-Urolume Era. Urology 2017;99:240-5. [Crossref] [PubMed]
- Keith CG, Davenport MT, Kavoussi M, et al. Long-term outcomes of anastomotic urethroplasty for radiation-induced strictures. World J Urol 2019. [Epub ahead of print]. [Crossref] [PubMed]


