
Pelvic fracture urethral injuries associated with rectal injury: a review of acute and definitive urologic and bowel management with long term outcomes
Introduction
Compound pelvic fractures are described as a pelvic fracture that is associated with a laceration of skin of the external genitalia, perineal, buttock, or are associated with a tear into the vagina or rectum. Pertinent to a urologist is the combination of a pelvic fracture, urethral disruption and rectal injury, where either a longitudinal tear through the bladder neck, prostatic or proximal urethra extends posteriorly into the rectum or when the posterior urethral disruption injury occurs simultaneous with a rectal injury. These concurrent urethral—rectal injuries are rare, occurring in approximately 3–5%, of all pelvic fracture urethral injuries (PFUI) (1-4). The recommended management of these combined wounds is by either a primary sutured repair of all injuries, suprapubic cystostomy and delayed repair or alternatively by approximation of the bladder neck laceration (BNL), and catheter realignment of the urethra. The concurrent rectal injuries are recommended to undergo a distal rectal and pelvic washout, pelvic drain placement and primary rectal repair if possible along with proximal enteric diversion. It is recommended that these procedures be performed during the acute post injury time period (4-7). Current treatment recommendations are by consensus opinion and are based on a paucity of clinical information (3,5-7). Indeed, to date we were unable to identify a publication that specifically looked at management and outcomes of patients with PFUI with concomitant bladder neck lacerations associated with rectal or anal injury. The purpose of this paper is to outline the urologic management and long-term sequela in this unique patient population. It is our hope that by defining the management plans we employed and critically looking at our outcomes, that we may improve the treatment and urologic prognosis of this complex patient population.
Methods
This a retrospective cohort study of a prospectively maintained database all male patients with pelvic fractures associated with a simultaneous urethral and rectal injury over a 28-year time period, 1990–2018. This research was performed with approval of the Mayo Clinic Internal Review Board (IRB 06-002981) and informed consent was obtained from all patients. Management of their urethral and rectal injuries, complications and outcome were recorded. The follow-up interval is defined by the length of follow-up after definitive urologic reconstruction.
Evaluation for erectile dysfunction criteria is based on the sexual history inventory for men (IIEF-5). Scoring has been performed routinely since 1997, at the 3-month post injury visit and at each yearly follow-up clinic visit. Erectile dysfunction was classified as severe (<7), moderate (8-11), mild-moderate (12-16), mild (17-21) and no erectile dysfunction (22-25). The score used for this paper is the value given at the last clinic visit (8).
Statistical analysis used the chi-square test or Fishers exact two tailed test where indicated, with P values <0.05 considered significant.
Results
A total of 18 patients presented with a simultaneous PFUI and rectal injury during this 25-year time span.
Review of mechanism of injury and GI and GU management
The patients’ specifics regarding, patient (pt) age at time of injury, mechanism of injury, presence of concurrent bladder neck lacerations (BNL), associated injuries or medical illnesses that impacted urologic care, initial and definitive urologic management, definitive bowel management, complications arising from surgical intervention and length of follow-up are noted in the Table 1.

Full table
Bowel management
Initial management of the bowel injury was by distal rectal and pelvic washout, diverting ileostomy or colostomy, pelvic drain placement, and primary rectal repair if possible. All of our patients underwent this approach within the first 24 hours following the traumatic event. Permanent enteric stomas are present in 72% (13/18). The decision to maintain an enteric stoma as a permanent fecal diversion was based upon the extent of the initial rectal injury precluding fecal continence in 33% (6/18) and/or the concurrent presence of a denervated rectal sphincter secondary to neural injuries in 17% (3/18). It is noteworthy, that 50% (9/18) of the patients underwent take down of the enteric stoma, 44% (4/9) developed uncontrollable chronic fecal incontinence per perineum and went on to permanent colostomy formation. Currently, 28% (5/18) are continent of stool per rectum. Of those fecally continent patients, 40% (2/5) developed early rectourethral fistula requiring delayed repair utilizing a York Mason technique.
Urologic management
The type of initial urologic surgery performed varied, dependent upon the presence of concurrent BNL. Indeed, 50% (9/18) had a concurrent BNL. In individuals with a BNL where all bladder neck and urethral tissues appeared viable, a primary sutured repair of the BNL and sutured urethral anastomosis was performed (N=4 pts). These patients at the completion of their procedure had a large bore suprapubic tube, urethral catheter and pelvic drain left in situ. In patients where viability of both the bladder neck tissues and proximal urethra appeared to be in jeopardy, we attempted to perform a water tight approximation of the bladder neck, leaving a large bore suprapubic tube and pelvic drain in situ (N=3). In patients, where the bladder neck tissues appeared viable, but a significant portion of the tissue was friable and suture approximation was not possible, we reconstructed the bladder neck, left a large bore suprapubic tube, realigned the urethra and placed a urethral catheter and pelvic drain (N=2). All initial bladder neck and urethral repairs were performed within five days of the traumatic event, i.e., following clinical stabilization of the patient. The initial attempt at a urologic reconstruction was performed prior to the permanent orthopedic stabilization.
In patients where a complete urethral obliterative stricture developed, delayed urethral reconstruction occurred at a minimum of three months post injury. The urethral repair used surgical principles based upon the perineal-abdominal progressive approach as described by Turner-Warwick (9).
The presence of a concurrent BNL is significantly related both to the development of septic pelvic complications and our inability to gain continent urethral voiding post injury. Specifically, despite our attempts to repair or approximate the bladder neck 56% (5/9) of the patients developed a chronic pelvic urinoma associated with life threatening pelvic sepsis. All five were managed by placement of bilateral percutaneous nephrostomy tubes for proximal urinary diversion and appropriate antibiotic therapy. Despite upper tract drainage 40% (2/5) developed necrotizing fasciitis and pelvic, pubic rami osteomyelitis. These two patients required multiple repetitive pelvic debridement procedures, pubic bone resection and prolonged antibiotic therapy. The association of a BNL to pelvic sepsis was significant, 56% (5/9) vs. 0% (0/8), P=0.012. In our patients with a history of a BNL, only 22% (2/9) are currently voiding per urethra, one patient with diaper dependent incontinence and one with stress incontinence. No patient (0/5) with BNL associated with persistent urine extravasation at the bladder neck and a history of pelvic sepsis is voiding per urethra.
In the nine patients without a BNL, a total of 33% (3/9) of these pts did not undergo further attempt at repair and are being managed by chronic suprapubic tube drainage. No reconstructive efforts were made in these individuals due to associated spinal cord injury (2 pts) or due to chronic alcoholism associated with a concomitant closed head injury and mental disability (1 pt). Two/thirds (67%; 6/9) are currently voiding per urethra, 50% (3/6) are continent and voiding per urethra without long term sequale, 17% (1/6) has stress incontinence post repair, and 33% (2/6) developed recurrent urethral strictures post urethroplasty. One of these individuals was treated with a single DVIU and has retrained urethral patency at four years post treatment, one is on daily intermittent catheterization to maintain patency, both are continent of urine.
In essence, 0% (0/9) of patients with a BNL are continent voiding per urethra compared to 44% (4/9) of patients without a BNL, this is not significant P=0.5.
Concurrent neurologic injury
Concurrent spinal cord injuries (4 pts) or traumatic brain injury (1 pt) were present in 28% (5/18). Two of these patients both with a simultaneous bladder neck injury elected to have a continent abdominal stoma as their long term management and are doing well at 11 and 12 years post definitive repair. Three patients without a bladder neck injury had neural injuries, spinal cord injuries (2 pts) and severe closed head injury (1 pt), all elected to be managed by a long term indwelling suprapubic tube. All have been offered alternative treatment options but have refused additional surgery. None of our five patients that had a concurrent neurologic injury (four spinal cord injuries and one closed head injury) underwent a urethroplasty.
Erectile dysfunction
Erectile dysfunction was assessed both prior to and following definitive urologic reconstruction. We did not find any alterations in erectile function following definitive repair and therefore only report the current SHIM score status. Only 11% (2/18) have erectile capability, both with mild erectile dysfunction (SHIM scores of 18 and 21). The remaining 89% (16/18) of patients have severe erectile dysfunction (SHIM score <7). It should be noted that 78% (14/18) of our patients had one or both hypogastric arteries angiographically embolized to prevent exsanguination as part of their initial management. Attempts to manage the erectile dysfunction in patients with severe erectile dysfunction (SHIM <7) were not successful with oral agents, two patients (13%; 2/16) are managed with injectable therapy and two (13%; 2/16) have had an artificial penile prosthesis placed. In essence, permanent erectile dysfunction, for which the pts have not pursued additional therapy, is present in 67% (12/18).
Discussion
Compound pelvic fractures definition, incidence, and significance
Compound pelvic fractures are described as a pelvic fracture where the urethra and rectum are injured will occur in approximately three- five percent of adult PFUI and in approximately 12–15% of PFUI in childhood (2,3,6,7,10). The four–five-fold increased risk of these combined injuries in children is presumed to be a consequence of the excessive force necessary to fracture the more pliable pediatric pelvic ring. The increased force necessary to produce a pelvic fracture in a child resulting in a higher incidence of concurrent injuries (6,7,10). The mortality following a compound pelvic fracture is significant. Indeed, in the 1980’s a 50% mortality incidence was routinely reported, with two thirds of the mortality directly related to uncontrollable hemorrhage and one third related to the late onset of pelvic sepsis secondary to either an enteric or urinary source (6,7,11-14). Over the past three decades improved methods to control pelvic hemorrhaging with protocols based on early angiographic embolization, pelvic packing, and temporary pelvic stabilization, significantly decreased the risk of exsanguination. A reduction in the risk of death from sepsis is attributed to the use of early fecal and urinary diversion, serial wound debridement, presacral wound drainage and wound vacuum placement. With the advent of improved radiological and surgical intervention, the post traumatic mortality from compound pelvic fractures decreased to 25% in the 1990’s, with current reports revealing mortality rates of 5% (6,7,11-14).
In 1991, we came to the realization that there was a paucity of information on this complex patient population upon which the urologist could base a treatment plan (2,11,12,15). We therefore elected to maintain a prospective database of this specific patient population, with the express purpose of cataloging the treatment methods employed, assess our outcomes and hopefully improve the patients’ quality of care. The purpose of this paper is to review our outcomes and recommend alterations in patient care based upon our findings.
Initial treatment of compound pelvic fracture with rectal involvement
In patients with a compound pelvic facture, the initial goal is prevention of exsanguination with the aggressive use of intravenous fluid, blood products, clotting factors, pressure dressings, embolization of all arterial bleeding sites, and temporary pelvic stabilization (6,7). Once the patient is hemodynamically stable, individuals with transmural rectal or anal lacerations will undergo a distal rectal washout and proximal diverting ileostomy or colostomy followed by a through debridement of nonviable tissue and primary rectal repair if possible (6,7,13,14,16). Once the rectal injury is addressed, surgical treatment of urogenital injuries, placement of pelvic drains, surgical stabilization of the pelvic fracture, by either external, open or combined techniques and finally wound vacuum placement will follow (3,6,7,13,14,16). As noted previously open pelvic fractures; are associated with a high mortality rate secondary to infection. To reduce this risk, patients will frequently be repetitively returned to the operative room for wound irrigation and debridement during the early post traumatic period. Due to the patients labile clinical course it is not unusual to have the urologic injuries addressed in a delayed fashion; however, they will typically be addressed by the fifth post-injury day (16).
Acute treatment of the pelvic fracture urethral injury (PFUI)
The immediate goal of the urologist when treating a complete urethral disruption associated with a rectal injury is to prevent the sequela of pelvic sepsis and osteomyelitis. This will be done by attempting to establish a mechanism for urinary continence and/or by proximal urinary diversion (2,15,16). In this regard it is noteworthy that 50% (9/18) of our patients had a concurrent BNL. The impact of this finding cannot be overstated, indeed, multiple publications have documented that a concurrent BNL is the most common cause of urinary incontinence following PFUI (1-3,10,15-18). It is also noteworthy that a ruptured or traumatically lacerated bladder neck and/or prostate will not close spontaneously, and is highly associated with urinary extravasation, pelvic cavitation, sepsis and osteomyelitis (2,15,19). Due to these findings it is recommended that any patient found to have a concurrent BNL in conjunction with a complete urethral disruption injury should undergo an urgent repair of the bladder neck with strong consideration for either a concurrent sutured primary repair of the urethral injury or urethral realignment (1,3,15-17). Although we attempted to maintain this principle of care, 56% (5/9) of our patients with a BNL developed a pelvic urinoma with subsequent abscess formation and pelvic sepsis. It is noteworthy that in all cases where pelvic sepsis occurred, proximal urinary diversions with bilateral nephrostomy tubes were eventually necessary to control urine extravasation and pelvic infection. Retrospectively, we recommend that in patients with concurrent rectal and bladder neck lacerations, the surgeon approximate the bladder neck and place either externalized ureteral stents and/or consider preemptive bilateral percutaneous nephrostomy tube placement. See Figure 1 for algorithm. Hopefully these maneuvers will optimize proximal urinary drainage, reducing the risk of urinary extravasation and pelvic sepsis. We currently concur with the opinion of other authors who have found no benefit to primary sutured urethral repair or urethral realignment in patients with a PFUI (20-23). Indeed, we are concerned that the urethral catheter balloon when left in situ at the time of urethral repair or realignment may place undue tension on an already tenuous and compromised bladder neck, exacerbating the risk of bladder neck repair dehiscence (20-23).
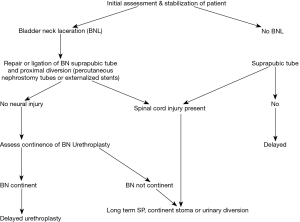
In the absence of a concurrent bladder neck laceration, we will place a suprapubic tube alone with plans for delayed urethral reconstruction, see Figure 1 for algorithm (20-23). Treatment by this methodology is expedient and associated with few urologic complications.
Associated spinal cord injury
Concurrent spinal cord injury with pelvic facture was clinically apparent in 22% (4/18) of our patients. It is noteworthy that our incidence of this complication, is approximately two/thirds of that found in a similar patient population where 33% of the patients were found to have sacral denervation that resulted in denervation of the pelvic sphincteric musculature (24). The impact of concurrent nerve damage on both urologic and colorectal outcomes cannot be overstated (3,25). In point of fact, none of our patients with spinal cord injuries have fecal or urinary continence and all are sexually impotent.
Long-term urinary and fecal incontinence
Due to the high incidence of coexisting BNL, 50% (9/18) and nerve injuries, either spinal cord or closed head injuries, 28% (5/18), the ability to gain volitional voiding and complete urinary continence per urethra was the rarity. Specifically, 22% (2/9) of our patients with a BNL are voiding per urethra, one is diaper dependent and the other has stress incontinence. In the nine patients without a BNL 67% (6/9) are voiding per urethra, one with stress incontinence, and two have required treatment for recurrent stricture disease. In essence, only 22% (4/18) or our patients are continent, volitionally voiding and free from recurrent urethral strictures, 0% (0/9) of our patients with a history of BNL compared to 44%, (4/9) patients without a bladder neck laceration.
Similarly fecal continence per perineum is rare, with either the initial traumatic injury to the rectum precluding repair and/or the presence of a denervated rectal sphincter making closure of the colostomy unreasonable. Only 28% (5/18) of our patients are fecally continent and are stooling per rectum.
Erectile dysfunction
Erectile dysfunction is almost routinely present following this constellation of injuries with only 11% (2/18) have erectile capability, both with mild erectile dysfunction (SHIM scores of 18 and 21). This finding is not surprising in view of the severe hemorrhage that was associated with these catastrophic injuries usually requiring the angiographic embolization of one if not both of the hypogastric arteries in the vast majority of the patients 78% (14/18). Unfortunately the consequences of both the neurologic and vascular damage resulted in only a minority of patients (13%; 2/16) being responsive to pharmacologic agents. Although offered the placement of a penile prosthesis, the vast majority of our patients with erectile dysfunction (75%; 12/16) refused placement stating they “had undergone enough surgery” and preferred not to pursue additional surgical intervention.
Conclusions
PFUI with simultaneous rectal lacerations have significant comorbid injuries that impact the acute urologic care, definitive surgical endeavors and long term prognosis. In an effort to reduce the incidence of post-traumatic pelvic urinoma with associated sepsis, we recommend that all patients with coexisting bladder neck lacerations undergo both primary repair or approximation of the bladder neck along with proximal urinary diversion during their initial phase of the surgical treatment.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This research was performed with approval of the Mayo Clinic Internal Review Board (IRB 06-002981) and informed consent was obtained from all patients.
References
- Martínez-Piñeiro L, Djakovic N, Plas E, et al. EAU Guideline on Urethral Trauma. Eur Urol 2010;57:791-803. [Crossref] [PubMed]
- Perry MO, Husmann DA. Urethral injuries in female subjects following pelvic fractures. J Urol 1992;147:139-43. [Crossref] [PubMed]
- Gómez RG, Mundy T, Dubey D, et al. SIU/ICUD Consultation on Urethral Strictures: Pelvic fracture urethral injuries. Urology 2014;83:S48-58. [Crossref] [PubMed]
- Jenkins BJ, Badenoch DF, Fowler CG, et al. Long-term results of treatment of urethral injuries in males caused by external trauma. Br J Urol 1992;70:73-5. [Crossref] [PubMed]
- Resnick M, Turner-Warwick R, Chapple C. Urethral Stricture. In: Cohen M, editor. Reoperative Urology New York: Little Brown and Company; 1995. p. 135-72.
- Grotz MR, Allami MK, Harwood P, et al. Open Pelvic Fractures: Epidemiology, current concepts of managment and outcome. Injury 2005;36:1-13. [Crossref] [PubMed]
- Govaert G, Siriwardhane M, Hatzifotis M, et al. Prevention of pelvic sepsis in major open pelviperineal injury. Injury 2012;43:533-6. [Crossref] [PubMed]
- Stein DM, Gonzalez CM, Barbagli G, et al. Erectile function in men with failed hypospadias repair. Arch Esp Urol 2014;67:152-6. [PubMed]
- Andrich DE, Day AC, Mundy AR. Proposed mechanisms of lower urinary tract injury in fractures of the pelvic ring. BJU Int 2007;100:567-73. [Crossref] [PubMed]
- Husmann D. Pediatric Genitourinary Trauma. In: Wein A, Kavoussi, A, Paritin A, Peters C, editor. Campbell-Walsh Urology 4. Philadelphia: Elsevier; 2016. p. 3552-3.
- Blandy JP, Singh M. Fistula involving the adult male urethra. Br J Urol 1972;44:632-43. [Crossref] [PubMed]
- Husmann DA, Wilson WT, Boone TB, et al. Prostatomembranous urethral disruptions: Management by suprapubic cystostomy and delayed urethroplasty. J Urol 1990;144:76-8. [Crossref] [PubMed]
- Davit FE, Schaefer GP, Po RP, et al. Open pelvic fracture and rectal injury managed with abdominoperineal resection. Am Surg 2010;76:E15-6. [PubMed]
- van Wessern K, Mackay P, King K, et al. Sellective faecal diversion in open pelvic factures: Reassessment based on recent experience. Injury 2012;43:522-5. [Crossref] [PubMed]
- Routh JC, Husmann DA. Long-term continence outcomes after immediate repair of pediatric bladder neck lacerations extending into the urethra. J Urol 2007;178:1816-8. [Crossref] [PubMed]
- Figler BD, Figler B, Hoffler CE, et al. Multi-disciplinary update on pelvic fracture associated bladder and urethral injuries. Injury 2012;43:1242-9. [Crossref] [PubMed]
- Kommu SS, Illahi I, Mumtaz F. Patterns of urethral injury and immediate management. Curr Opin Urol 2007;17:383-9. [Crossref] [PubMed]
- Koraitim MM. Complex pelvic fracture urethral distraction defects revisited. Scand J Urol 2014;48:84-9. [Crossref] [PubMed]
- Gao W, Xu C, Xu Y. The study of etiology about erectile dysfunction after pelvic fracture urethral injury. Chin J Urol 2000;21:378-81.
- Zou Q, Zhou S, Zhang K, et al. The Immediate Management of Pelvic Fracture Urethral Injury-Endoscopic Realignment or Cystostomy? J Urol 2017;198:869-74. [Crossref] [PubMed]
- Tausch TJ, Morey AF, Scott JF, et al. Unintended negative consequences of primary endoscopic realignment for men with pelvic fracture urethral injuries. J Urol 2014;192:1720-4. [Crossref] [PubMed]
- Horiguchi A, Shinchi M, Masunaga A, et al. Primary Realignment for Pelvic Fracture Urethral Injury Is Associated With Prolonged Time to Urethroplasty and Increased Stenosis Complexity. Urology 2017;108:184-9. [Crossref] [PubMed]
- Elshout PJ, Veskimae E, MacLennan S, et al. Outcomes of Early Endoscopic Realignment Versus Suprapubic Cystostomy and Delayed Urethroplasty for Pelvic Fracture-related Posterior Urethral Injuries: A Systematic Review. Eur Urol Focus 2017;3:545-53. [Crossref] [PubMed]
- Majeed S. Neurologic deficits in major pelvic injuries. Clin Orthop Relat Res 1992.222-8. [PubMed]
- Angermeier KW, Rourke KF, Dubey D, et al. SIU/ICUD Consultation on Urethral Strictures: Evaluation and follow-up. Urology 2014;83:S8-17. [Crossref] [PubMed]


