
Reusable flexible ureterorenoscopes are more cost-effective than single-use scopes: results of a systematic review from PETRA Uro-group
Introduction
Ureteroscopy for stone disease has risen over the last two decades reflecting an increase in the lifetime prevalence of stone disease of up to 14% (1,2). Warm weather, metabolic syndrome, diet and lifestyle are all blamed for this rise (3-5). There has also been broadening indication for its use and it is now preferably been used for stone treatment in paediatrics, pregnancy and obese patients (6-8).
Flexible ureterorenoscopy is now one of the first-choice treatment option for renal stones up to 2 cm (9). As the technology advances, the scope has improved in vision, manoeuvrability, deflection and weight (10-12). With advances in digital technology, single use flexible ureterorenoscope (fURS) are now being marketed and used, with tests showing comparable results in terms of scope characteristics and vision (13-16). While the traditional reusable scopes have a fixed purchase cost, there is additional cost related to scope processing and repairs (17).
The cost of single-use fURS is defined with the initial purchase price, whereas the procedural cost of reusable fURS is dependent on the initial and repair cost, maintenance and scope sterilization/disinfection and on the number of procedures performed before it needs to be repaired. There is also the cost of repair and the number of procedures with a refurbished scope until it has to be replaced. We conducted a systematic review on the cost ($) of fURS based on author reported data on the number of procedures performed before repair, and to compare the cost with disposable flexible ureteroscopes.
Materials and methods
A systematic review was carried out in a Cochrane style and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (18) checklist using MEDLINE, Scopus, CINAHL, EMBASE and Cochrane (19) library for all English language articles. All papers on cost analysis, which mentioned the cost of fURS based on the number of procedures performed and the repairs needed (procedure/repair) as reported by the individual authors, from 2000 to 2018, were included. The latest literature search was performed on June 2018. The search terms researched were “flexible ureterorenoscope”, “cost”, “single use ureterorenoscope”, “single use”, “disposable”, “reusable”, “ureteroscope”, “URS”, “retrograde intra renal surgery” and “RIRS”.
Data was extracted independently by two authors (BK Somani, M Talso) and all discrepancy was resolved by mutual consensus. Costs were initially expressed in USD ($) and Euro (€). Costs in Euros were converted in USD using an online currency converter, with the exchange rate of €1= $1.17. The following information regarding each eligible study was recorded: author’s name, journal of publication, year of publication, country of origin of the first author, study type and total number of cases performed during the study period. Data on brand and model of flexible reusable and single-use scope were also recorded.
Results
Study selection and characteristics
The initial search strategy identified 995 potentially eligible studies of which 19 articles (15,17,20-36) met the inclusion criteria and were considered for this systematic review (Table 1). The studies were published between 2006 and June 2018. Nine studies were performed in the Unites States (21,22,25-30,36), five in Europe (Germany, The Netherlands, France) (15,20,31,33,34), three in the United Kingdom (17,23,24), one in Brazil (35) and one in Australia (32). Thirteen were prospective studies (15,17,20-22,24,27-30,34-36), 4 were retrospective (23,25,26,33), one was a review article (33) and one was a basic-science benchmark study (31).
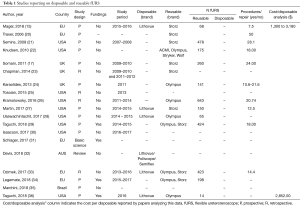
Full table
The brand of the reusable scope was noted in 14 studies: in eight studies Olympus scopes were used (P5, P6, URF-V and URF-V2); in eight studies Karl Storz flexible scopes were used (11278 AU1 Flex X, Flex XC and Flex X2); in one study Wolf Viper, Gyrus ACMI DUR8-E and Stryker Flex-Vision U-500 were used (Table 1). In relation to the disposable scope, six studies remarked which scope was used. All these studies analysed the Boston Scientific LithovueTM scope. Davis et al. (32) in the systematic review, included the PoliscopeTM and the SemiFlexTM. Four studies received industry funding for their study whereas 14 studies did not receive any funding. In one study funding support was not specified (Table 1).
Meta-analysis of studies
Only 5 studies compared disposable and reusable instruments (15,27,28,36) of which 2 studies were multicentric (22,29), 1 was a review (32) and one was a basic science study (31). The rest of them were single-centre studies. Given the substantial heterogeneity across studies we did not attempt a meta-analysis because it would not have yielded clinically meaningful results; data were descriptively summarized.
Repair and procedures performed for re-usable scopes
Out of 19 studies, 11 performed an analysis on number of procedures performed with number of repairs needed (15,17,20-22,24,26,27,29,33,34) (Table 2). The number of uses/repair in various studies varied between 7.5 to 50 procedures with reusable fURS. Eight studies reported an average time to failure, measured as the number of breakages on the total of the fURS performed in a given period of time (15,17,20,21,24,26,27,33). Two authors reported the mean +/– standard deviation and one author reported the median +/– the interquartile range (22,29) (Table 2). Taguchi et al. in a prospective multi centric study, reported the average number of procedures performed by each non-repaired scope, compared to the number of procedures performed by each repaired scope (29).
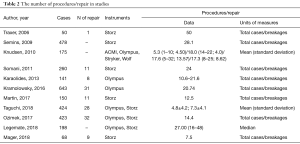
Full table
Cost per procedure using re-usable or single use scope
Eight studies calculated the total costs of reusable fURS repair in a given period of time and they divided it by the number of cases performed (15,17,21,25-27,33,36), obtaining the average repair cost per case (Table 3) that ranged from $120.73 to $957.61. Six authors performed a cost-per-procedure analysis regarding the reusable fURS (15,17,25,27,33,36). In this case, the lowest cost per case was reported as $197 by Somani and colleagues (17). The cost per repair was $7521 in Tosoian et al.’s study (25) giving an average cost of $355 per fURS performed. Single use scopes prices varied from $700 to $1,500 per disposable scope (32).
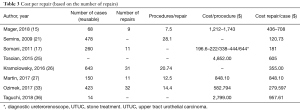
Full table
Discussion
Ureteroscopy is a safe effective procedure to access the upper urinary tract (37,38). Reusable flexible ureteroscopes are now well established for diagnosis and treatment of stones and upper tract tumours. There are proven benefits of new digital fURSs compared to the traditional optical ones, especially in terms of their image quality (15). Disposable digital flexible ureteroscopes are new entrants in the market with similar clinical outcomes to the existing scopes (15,39).
There seems to be a surge of clinical papers on the use of disposable scopes. The cost seems to vary between different manufacturers and the special discounts they give for the amount of usage, however, these costs seem to vary between $700 to $1,500 (32). While there is more interest and wider use of these disposable scopes in USA, the use would be dictated by the healthcare system, the reimbursement for the procedure and ultimately who would be responsible to bear the cost of these procedures or scopes. Although costs need to be justified, in some countries like France, Italy and UK where public health system provides a full reimbursement for surgical interventions the use of disposable scopes would be higher compared to a predominantly private healthcare system in some Asian countries such as India. Similarly, when private insurance covers the cost of all consumables, it is perhaps easier to use them. With global URS cases set to rise, there will be an increased demand of both reusable and disposable scopes in the future (40).
Our review shows that there is no one standardized method to analyse costs among reported studies. The data is heterogeneous that makes it difficult to analyse the overall cost. For example, Somani et al. (17) analysed the average cost of each flexible ureterorenoscopy by dividing the total cost based on the number of repairs and the ancillary costs for the procedure. In their study the cost of diagnostic flexible ureteroscopy ranged from $196.6 to $222, and the cost of stone treatment ranged between $444 and $644 although they excluded the cost of the initial purchase of the ureterorenoscopes and the holmium laser. In another study, Mager et al. calculated the costs with and without the instrument purchase price, with a cost variation that ranged from $436 to $1,743 per case respectively (15). On the contrary, Tosoian and colleagues presented their data with direct variable costs, indirect variable costs, direct fixed costs, and indirect fixed costs and they calculated that the average institutional cost of each URS was $4,852 (25).
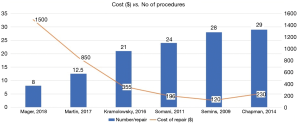
Due to differences in cost comparison and reporting, it is difficult to compare costs across studies. As Mager and colleagues showed, the longer a reusable fURS’s endurance the more cost-saving is a reusable ureterorenoscope program. The authors hypothesized that centres performing only a small number of flexible ureterorenoscopies per year might realize cost savings using single-use ureterorenoscopes, particularly if the purchase of an expensive new plasma sterilization system was necessary. They fixed the threshold of 61 cases per year/institution for preferring reusable ureterorenoscopes instead of single-use ureterorenoscopes if calculated with the lower limit recurring and reprocessing costs for the reusables (15). There was a wide variation in the literature on the cost of repair and the number of cases/repair (Figure 1). Although when we consider all studies that looked at cost of repair and number of repairs both, it was clear that as the number of repairs reduced, so did the cost of doing the procedure (Figure 2). When we take these 6 studies into account, the mean cost per repair per procedure was $370, which needs to be added to the initial cost of equipment purchase and the reprocessing costs which might vary across different countries.
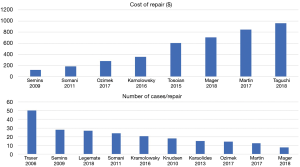
The cost repair/case rate, indicates the cost of a repair divided by the number of usages of the instrument before the breakage. To better understand this ratio, imagine to use a scope 10 times before the breakage and the total cost to repair the scope is 10,000 USD: the ratio will be 10,000/10. This means that the cost of repair will be 1,000 USD per case. The more cases performed with a multiple use instrument, the less this ratio will be.
We can hypothesise that in high volume centres, reusable fURSs is likely to be cost effective. Based on literature, the carbon footprint of single use and reusable ureteroscopes seems to be comparable and is also likely that the cost of disposable scopes will reduce in future (39). Some studies have compared new reusable ureteroscopes to disposable scopes, and with the former degrading with time and usage, it might give an edge to the single use scopes. Given the substantial heterogeneity across studies in our review it was not possible to perform a meta-analysis.
Conclusions
Although, the disposable and reusable scopes seem to be comparable in terms of their performance, reusable scopes seem to be more cost effective in high volume centres. The overall procedural costs for reusable scopes depend on the initial capital outlay, reprocessing and importantly the number of repairs needed.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Rukin NJ, Siddiqui ZA, Chedgy ECP, et al. Trends in Upper Tract Stone Disease in England: Evidence from the Hospital Episodes Statistics Database. Urol Int 2017;98:391-6. [Crossref] [PubMed]
- Pietropaolo A, Proietti S, Geraghty R, et al. Trends of ‘Urolithiasis: Interventions, Simulation and Laser technology’ over the last 16 years (2000-2015) as published in the literature (PubMed): A systematic review. World J Urol 2017;35:1651-8. [Crossref] [PubMed]
- Geraghty RM, Proietti S, Traxer O, et al. Worldwide impact of warmer seasons on the incidence of renal colic and kidney stone disease (KSD): Evidence from a systematic review of literature. J Endourol 2017;31:729-35. [Crossref] [PubMed]
- Wong YV, Cook P, Somani BK. The association of metabolic syndrome and urolithiasis. Int J Endocrinol 2015;2015:570674.
- Wong Y, Cook P, Roderick P, et al. Metabolic syndrome and kidney stone disease: A systematic review of literature. J Endourol 2016;30:246-53. [Crossref] [PubMed]
- Featherstone NC, Somani BK, Griffin S. Ureteroscopy and laser stone fragmentation (URSL) for large (>1cm) paediatric stones: Outcomes from a University Teaching Hospital. J Pediatr Urol 2017;13:202.e1-202.e7. [PubMed]
- Ishii H, Couzins M, Aboumarzouk O, et al. Outcomes of Systematic Review of Ureteroscopy for Stone Disease in the Obese and Morbidly Obese Population. J Endourol 2016;30:135-45. [Crossref] [PubMed]
- Ishii H, Aboumarzouk O, Somani BK. Current status of ureteroscopy for Stone Disease in Pregnancy. Urolithiasis 2014;42:1-7. [Crossref] [PubMed]
- Tekgül S, Dogan HS, Hoebeke P, et al. EAU Guidelines on Paediatric Urology. European Association of Urology. 2016. Accessed July 2018. Available online: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Paediatric-Urology-2016-1.pdf
- Talso M, Proietti S, Emiliani E, et al. Comparison of Flexible Ureterorenoscope Quality of Vision: An In Vitro Study. J Endourol 2018;32:523-8. [Crossref] [PubMed]
- Proietti S, Somani B, Sofer M, et al. The "Body Mass Index" of Flexible Ureteroscopes. J Endourol 2017;31:1090-95. [Crossref] [PubMed]
- Dragos LB, Somani BK, Sener ET, et al. Which Flexible Ureteroscopes (Digital vs Fiber-optic) can reach the difficult lower pole calices and have better end-tip deflection: In vitro study on K-box. A PETRA Evaluation. J Endourol 2017;31:630-7. [Crossref] [PubMed]
- Emiliani E, Traxer O. Single use and disposable flexible ureteroscopes. Curr Opin Urol 2017;27:176-81. [Crossref] [PubMed]
- Davis NF, Quinlan MR, Browne C, et al. Bolton Single-use flexible ureteropyeloscopy: a systematic review. World J Urol 2018;36:529-36. [Crossref] [PubMed]
- Mager R, Kurosch M, Höfner T, et al. Clinical outcomes and costs of reusable and single-use flexible ureterorenoscopes: a prospective cohort study. Urolithiasis 2018;46:587-93. [Crossref] [PubMed]
- Hennessey DB, Fojecki GL, Papa NP, et al. Single-use disposable digital flexible ureteroscopes: an ex vivo assessment and cost analysis. BJU Int 2018;121 Suppl 3:55-61. [Crossref] [PubMed]
- Somani BK, Robertson A, Kata SG. Decreasing the cost of flexible ureterorenoscopic procedures. Urology 2011;78:528-30. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [Crossref] [PubMed]
- Higgins JPT, Green S. editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0: updated March 2011. 2011. Available online: https://handbook-5-1.cochrane.org/
- Traxer O, Dubosq F, Jamali K, et al. New-generation flexible ureterorenoscopes are more durable than previous ones. Urology 2006;68:276-9; discussion 280-1. [Crossref] [PubMed]
- Semins MJ, George S, Allaf ME, et al. Ureteroscope cleaning and sterilization by the urology operating room team: the effect on repair costs. J Endourol 2009;23:903-5. [Crossref] [PubMed]
- Knudsen B, Miyaoka R, Shah K, et al. Durability of the next-generation flexible fiberoptic ureteroscopes: a randomized prospective multi-institutional clinical trial. Urology 2010;75:534-8. [Crossref] [PubMed]
- Chapman RA, Somani BK, Robertson A, et al. Decreasing cost of flexible ureterorenoscopy: single-use laser fiber cost analysis. Urology 2014;83:1003-5. [Crossref] [PubMed]
- Karaolides T, Bach C, Kachrilas S, et al. Improving the durability of digital flexible ureteroscopes. Urology 2013;81:717-22. [Crossref] [PubMed]
- Tosoian JJ, Ludwig W, Sopko N, et al. The effect of repair costs on the profitability of a ureteroscopy program. J Endourol 2015;29:406-9. [Crossref] [PubMed]
- Kramolowsky E, McDowell Z, Moore B, et al. Cost Analysis of Flexible Ureteroscope Repairs: Evaluation of 655 Procedures in a Community-Based Practice. J Endourol 2016;30:254-6. [Crossref] [PubMed]
- Martin CJ, McAdams SB, Abdul-Muhsin H, et al. The Economic Implications of a Reusable Flexible Digital Ureteroscope: A Cost-Benefit Analysis. J Urol 2017;197:730-5. [Crossref] [PubMed]
- Usawachintachit M, Isaacson DS, Taguchi K, et al. A Prospective Case-Control Study Comparing LithoVue, a Single-Use, Flexible Disposable Ureteroscope, with Flexible, Reusable Fiber-Optic Ureteroscopes. J Endourol 2017;31:468-75. [Crossref] [PubMed]
- Taguchi K, Harper JD, Stoller ML, et al. Identifying factors associated with need for flexible ureteroscope repair: a Western Endourology STone (WEST) research consortium prospective cohort study. Urolithiasis 2018;46:559-66. [Crossref] [PubMed]
- Isaacson D, Ahmad T, Metzler I, et al. Defining the Costs of Reusable Flexible Ureteroscope Reprocessing Using Time-Driven Activity-Based Costing. J Endourol 2017;31:1026-31. [Crossref] [PubMed]
- Schlager D, Hein S, Obaid MA, et al. Performance of Single-Use FlexorVue vs Reusable BoaVision Ureteroscope for Visualization of Calices and Stone Extraction in an Artificial Kidney Model. J Endourol 2017;31:1139-44. [Crossref] [PubMed]
- Davis NF, Quinlan MR, Browne C, et al. Single-use flexible ureteropyeloscopy: a systematic review. World J Urol 2018;36:529-36. [Crossref] [PubMed]
- Ozimek T, Schneider MH, Hupe MC, et al. Retrospective Cost Analysis of a Single-Center Reusable Flexible Ureterorenoscopy Program: A Comparative Cost Simulation of Disposable fURS as an Alternative. J Endourol 2017;31:1226-30. [Crossref] [PubMed]
- Legemate JD, Kamphuis GM, Freund JE, et al. Durability of Flexible Ureteroscopes: A Prospective Evaluation of Longevity, the Factors that Affect it, and Damage Mechanisms. Eur Urol Focus 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Marchini GS, Batagello CA, Monga M, et al. In Vitro Evaluation of Single-Use Digital Flexible Ureteroscopes: A Practical Comparison for a Patient-Centered Approach. J Endourol 2018;32:184-91. [Crossref] [PubMed]
- Taguchi K, Usawachintachit M, Tzou DT, et al. Micro-Costing Analysis Demonstrates Comparable Costs for LithoVue Compared to Reusable Flexible Fiberoptic Ureteroscopes. J Endourol 2018;32:267-73. [Crossref] [PubMed]
- de la Rosette J, Denstedt J, Geavlete P, et al. The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 2014;28:131-9. [Crossref] [PubMed]
- Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol 2016;69:475-82. [Crossref] [PubMed]
- Davis NF, McGrath S, Quinlan M, et al. Carbon Footprint in Flexible Ureteroscopy: A Comparative Study on the Environmental Impact of Reusable and Single-Use Ureteroscopes. J Endourol 2018;32:214-7. [Crossref] [PubMed]
- Somani BK, Giusti G, Sun Y, et al. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: the Clinical Research Office of Endourological Society URS Global study. World J Urol 2017;35:675-81. [Crossref] [PubMed]


