Safety and efficacy of ureteroscopy and stone fragmentation for pediatric renal stones: a systematic review
Introduction
There has been a rise in the incidence of kidney stone disease (KSD) globally (1-4). The overall lifetime prevalence of KSD in the UK now stands at 14% (2). Furthermore, of those patients that are known to have stone disease, there is a recurrence rate of 50–75% at 10 years (3). Although paediatric stone disease remains proportionally much lower than in the adult population, it is thought that the number of cases diagnosed worldwide is on the rise (1,3).
Flexible ureteroscopy (FURS) has long been an established treatment for adult stone disease and its use is becoming increasing popular in the paediatric population (4). Richie et al. first used URS to extract lower ureteric stones in children in 1988 and since then it has been an exciting and developing field of surgery (5,6). With ongoing and emerging advancements in technology, the URS equipment continues to be adapted for paediatric use whilst training opportunities for surgeons have made this a safe intervention. Ureteroscopy can therefore now be used as a treatment for both ureteric and renal paediatric stone disease of varying and increasing complexion. It is fast becoming the mainstay of treatment, meaning that the prolonged hospital stays and long open operations that were previously required, are thankfully increasingly rare (7). However, as this is relatively new practice, there is currently limited evidence with regards the efficacy and safety of its use within specifically the paediatric population. The current evidence suggests that ureteroscopy could be a viable treatment option for paediatric stone disease (8-13).
We wanted to look at the outcomes of flexible ureteroscopy and laser lithotripsy (FURSL) in the paediatric population for stone disease. This would help to better understand its efficacy and safety and therefore its role within the treatment of stone disease in this age group. We conducted a systematic review of literature looking at the outcomes of FURSL for paediatric stone disease.
Methods
We conducted a Cochrane-style systematic review carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) checklist. All major databases were searched including MEDLINE, CINAHL, EMBASE, Scopus, and the Cochrane library. Search terms included ‘paediatric’, ‘ureteroscopy’, ‘flexible’, ‘stones’, ‘calculi’, ‘infants’, ‘retrograde intra renal surgery’, ‘RIRS’, ‘URS’, ‘FURSL’ and ‘ureterorenoscopy’. All English language articles published between January 1990-December 2018 on FURSL in patients ≤18 years of age were included. There were no additional exclusion criteria. Data was then pooled with an existing systematic review and analysed accordingly (14).
Results
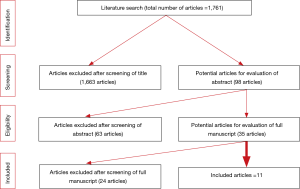
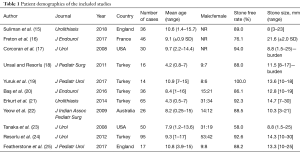
A total of 11 studies (431 patients) were found to meet the criteria set for the review (Figure 1). Of these studies, 5 were published from Turkey, 2 from the USA, 2 from England and 1 each from France and Australia (Table 1). Of the patients included in the study, the male:female ratio was 1.1:1. Gender was not commented on studies by Suliman, Freton or Corcoran (15-17). The mean age of the patients was 8.5 years with a range of 0.25–17 years. Of the studies reported, the mean operating duration was 62 minutes with a mean length of stay of 1.3 days (range, 0–5 days). Nine studies commented on the mean stone size reported as 13 mm (1.5–30 mm), and a mean stone burden reported across 2 other studies of 10.2 mm (1.5–25 mm) (17,18).
Full table
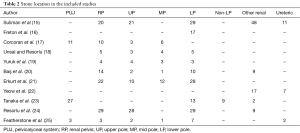
Stone location was variable with majority (n=483) being renal stones. Of these locations, they were in the lower pole (n=141), renal pelvis (n=107), upper pole (n=73), middle pole (n=27) and other unspecified renal stones (n=85) (Table 2). The other stone locations were in the ureteropelvic junction (n=41) and ureteric stones (n=20).
Full table
Seven studies (15,16,19-23) commented on pre-operative stent insertion rates. Of these studies, the mean pre-operative stenting rate was 42.6% (7.1–96.20%). The laterality of the stones was not routinely commented on. The overall stone free rate (SFR) was 87% (58–100%). An average of 76% (60–98%) cases required post-operative stent insertion and three studies (20-22) did not comment on ureteric stent insertion rates.
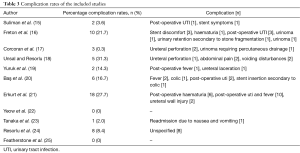
The mean complication rate was 12.6% (n=55) (range, 0–31.3%) with two studies reporting no complications at all. The most frequently occurring complications were fever and urinary tract infection (UTI), haematuria and post-operative pain, including stent discomfort. The complications were classified according to the Clavien classification. Clavien I/II included fever and UTI (n=19), stent discomfort/stent symptoms/post-operative pain (n=8), voiding disturbance (n=2), haematuria (n=7), and post-operative nausea and vomiting (n=1). Clavien III complications included urinoma (n=1), ureteral injury which included perforation (n=6) and acute urinary retention secondary to stone fragmentation (n=1). Clavien IV included urinoma (n=2) and there were no Clavien V complications. The overall complication rate for Clavien I/II complications was 8.9% (n=35), the complication rate for Clavien III/IV complications was 2.5% (n=10). The complications encountered in the paper by Resorlu (24) were unspecified, however there was a reported complication rate of 8.4% (n=8) (Table 3).
Full table
Discussion
Meaning of our review
This review aimed to establish the efficacy and safety of FURS and laser stone fragmentation for the treatment of paediatric stone disease. A total of 11 studies were eligible for inclusion within the study and evidence appears to suggest that ureteroscopy for the management of paediatric stone disease is safe and effective with a low risk of major complications.
Over the past decade, the use of ureteroscopy for the treatment of stone disease has increased dramatically and could be considered the mainstay of initial treatment for both adult and paediatric stone disease. Advances in technology mean that we are now able to use ureteroscopy to treat stones that previously required open surgery. The use of ureteroscopy means that we are able to minimize operating times and cut the length of hospital stays. Only four papers commented on the length of hospital stay after ureteroscopy with a mean stay of 1.3 days (range, 0–5 days) (15,16,20,25). They also commented upon the mean length of operation which was 62 minutes.
Role of paediatric ureteroscopy in literature
Recently, a twin surgeon approach with a paediatric urologist and an experienced adult endourologist has been recommended and this seems to be a sensible approach for achieving good results in paediatric patients (25,26). The results also seem to be equally good in medium and high volume centres (27). Although there is also a rise in minimally invasive PCNL techniques, it seems that URS is also cost effective and is being performed in a wide cohort of patients (28-30). Compared to adult URS, paediatric URS is still performed in a much smaller cohort of patients with an overall risk of complications which is slightly higher than their adult counterparts (31). This slightly increased complication rate may be due to the fact that the paediatric population are surgically and technically more challenging (14). It may also be secondary to the fact that the use of ureteroscopy in the paediatric population is fairly new practice and therefore the equipment and techniques used are still evolving.
Strengths, limitations and areas of future research
Although there are still only a few studies on FURS for paediatric stone disease, our review provides is comprehensive and covers all aspects of this intervention. Clearly there is still a publication bias with only 3 of these studies with over 50 patients. Given that paediatric URS is not common, perhaps multi-centric prospective studies will help in standardised reporting and outcome measure to provide a better quality of evidence.
Conclusions
The use of ureteroscopy for the treatment of paediatric renal stones has increased. Paediatric ureteroscopy appears to achieve a good SFR with a low risk of morbidity when performed in tertiary centres with skilled and experienced surgeons.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Available online: (accessed 19/12/2018)http://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Paediatric-Urology-2018-large-text.pdf
- Rukin NJ, Siddiqui ZA, Chedgy ECP, et al. Trends in Upper Tract Stone Disease in England: Evidence from the Hospital Episodes Statistics (HES) Database. Urol Int 2017;98:391-6. [Crossref] [PubMed]
- Available online: (accessed 19/12/2018).http://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Urolithiasis-2018-large-text.pdf
- Pietropaolo A, Proietti S, Geraghty R, et al. Trends of ‘urolithiasis: interventions, simulation, and laser technology’ over the last 16 years (2000–2015) as published in the literature (PubMed): a systematic review from European section of Uro-technology (ESUT). World J Urol 2017;35:1651-8. [Crossref] [PubMed]
- Ritchey M, Patterson DE, Kelalis PP. A case of pediatric ureteroscopic lasertripsy. J Urol 1988;139:1272-4. [Crossref] [PubMed]
- Ghosh A, Oliver R, Way C, et al. Results of day-case ureterorensocopy (DC-URS) for stone disease: prospective outcomes over 4.5 years. World J Urol 2017;35:1757-64. [Crossref] [PubMed]
- Geraghty RM, Jones P, Somani BK. Worldwide Trends of Urinary Stone Disease Treatment Over the Last Two Decades: A Systematic Review. J Endourol 2017;31:547-56. [Crossref] [PubMed]
- Schuster TG, Russell KY, Bloom DA, et al. Ureteroscopy for the treatment of urolithiasis in children. J Urol 2002;167:1813-; discussion 1815-6.
- Wollin TA, Teichman JM, Rogenes VJ, et al. Holmium: YAG lithotripsy in children. J Urol 1999;162:1717-20. [Crossref] [PubMed]
- Minevich E, Rousseau MB, Wacksman J, et al. Pediatric ureteroscopy: technique and preliminary results. J Pediatr Surg 1997;32:571-4. [Crossref] [PubMed]
- Kurzrock EA, Huffman JL, Hardy BE, et al. Endoscopic treatment of pediatric urolithiasis. J Pediatr Surg 1996;31:1413-6. [Crossref] [PubMed]
- al Busaidy SS, Prem AR, Medhat M. Paediatric ureteroscopy for ureteric calculi: a 4-year experience. Br J Urol 1997;80:797-801. [Crossref] [PubMed]
- Thomas R, Ortenberg J, Lee BR, et al. Safety and efficacy of pediatric ureteroscopy for management of calculous disease. J Urol 1993;149:1082-4. [Crossref] [PubMed]
- Ishii H, Griffin S, Somani B. Flexible ureteroscopy and lasertripsy (FURSL) for paediatric renal calculi: Results from a systematic review. J Pediatr Urol 2014;10:1020-5. [Crossref] [PubMed]
- Suliman A, Burki T, Garriboli M, et al. Flexible ureterorenoscopy to treat upper urinary tract stones in children. Urolithiasis 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Freton L, Peyronnet B, Arnaud A, et al. Extracorporeal Shockwave Lithotripsy Versus Flexible Ureteroscopy for the Management of Upper Tract Urinary Stones in Children. J Endourol 2017;31:1-6. [Crossref] [PubMed]
- Corcoran AT, Smaldone MC, Mally D, et al. When is prior ureteral stent placement necessary to access the upper urinary tract in prepubertal children? J Urol 2008;180:1861-3; discussion 1863-4.
- Unsal A, Resorlu B. Retrograde intrarenal surgery in infants and preschool-age children. J Pediatr Surg 2011;46:2195-9. [Crossref] [PubMed]
- Yuruk E, Tuken M, Gonultas S, et al. Retrograde intrarenal surgery in the management of pediatric cystine stones. J Pediatr Urol 2017;13:487.e1-487.e5. [Crossref] [PubMed]
- Baş O, Dede O, Aydogmus Y, et al. Comparison of Retrograde Intrarenal Surgery and Micro-Percutaneous Nephrolithotomy in Moderately Sized Pediatric Kidney Stones. J Endourol 2016;30:765-70. [Crossref] [PubMed]
- Erkurt B, Caskurlu T, Atis G, et al. Treatment of renal stones with flexible ureteroscopy in preschool age children. Urolithiasis 2014;42:241-5. [Crossref] [PubMed]
- Yeow WC, Pemberton R, Barker A. Flexible Ureteroscopy and laser lithotripsy in children. J Indian Assoc Pediatr Surg 2009;14:63-5. [Crossref] [PubMed]
- Tanaka ST, Makari JH, Pope JC 4th, et al. Pediatric ureteroscopic management of intrarenal calculi. J Urol 2008;180:2150-3; discussion 2153-4. [Crossref] [PubMed]
- Resorlu B, Unsal A, Tepeler A. Comparison of retrograde intrarenal surgery and mini-percutaneous nephrolithotomy in children with moderate-size kidney stones: results of multi-institutional analysis. Urology 2012;80:519-23. [Crossref] [PubMed]
- Featherstone NC, Somani BK, Griffin SJ. Ureteroscopy and laser stone fragmentation (URSL) for large (≥1 cm) paediatric stones: Outcomes from a university teaching hospital. J Pediatr Urol 2017;13:202.e1-202.e7. [PubMed]
- Somani BK, Griffin S. Ureteroscopy for paediatric calculi: The twin-surgeon model. J Pediatr Urol 2018;14:73-4. [Crossref] [PubMed]
- Rob S, Jones P, Pietropaolo A, et al. Ureteroscopy for Stone Disease in Paediatric Population is Safe and Effective in Medium-Volume and High-Volume Centres: Evidence from a Systematic Review. Curr Urol Rep 2017;18:92. [Crossref] [PubMed]
- Wright A, Rukin N, Smith D, et al. ‘Mini, Ultra, Micro’ - Nomenclature and cost of these new minimally invasive percutaneous nephrolithotomy (PCNL) techniques. Ther Adv Urol 2016;8:142-6. [Crossref] [PubMed]
- Somani BK, Robertson A, Kata G. Decreasing cost of Flexible ureterorenoscopic procedures: Cost volume relationship. Urology 2011;78:528-30. [Crossref] [PubMed]
- Ishii H, Couzins M, Aboumarzouk O, et al. Outcomes of systematic literature review of Ureteroscopy for stone disease in the Obese and Morbidly Obese Population. J Endourol 2016;30:135-45. [Crossref] [PubMed]
- Somani BK, Giusti G, Sun Y, et al. Complications associated with ureteroscopy (URS) related to treatment of urolithiasis: The Clinical Office of Endourological Society URS Global Study. World J Urol 2017;35:675-81. [Crossref] [PubMed]