Pictorial review of tips and tricks for ureteroscopy and stone treatment: an essential guide for urologists from PETRA research consortium
Introduction
Ureteroscopy (URS) was first described by Marshall in 1964 although it was only in 1987 that Bagley introduced the flexible URS (fURS) (1,2). From treatment of small stones in index patients, the spectrum of ureteroscopic stone surgery has now increased to treat large renal stones, stones in pregnancy, morbid obese, urinary diversion, paediatrics and patients with calyceal diverticula (3-7). Similarly, it is now used as a first line diagnostic tool for upper tract TCC and for its treatment in selected group of patients (8,9).
While there are a few papers that mention the ‘tips and tricks’, they lack the pictorial description of some of the key aspects of URS and stone treatment. In this review article we describe some of these important steps, supplemented with pictures, which enhances the understanding of these steps.
Operating room (OR) set-up and preparation for URS procedure
Under general anaesthesia, with peri-operative antibiotic prophylaxis, the patient is placed in a lithotomy position and the fluoroscopy is set-up. For fluoroscopy, always place the X-ray source under the table and the receptor above but closer to the patient to decrease the zoom effect and the radiation exposure to the surgeon.
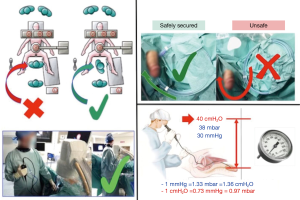
As the operator is standing, it is recommended that he/she is not directly facing the patient. The ideal position is a 90-degree rotation in a lateral position. This allows the operator to block and control the ureteroscope (Figure 1). The safety wire is secured inside the plastic sheath of the wire. To avoid displacement, this should be at the same level and as close to the urethral orifice as possible (Figure 1). To maintain a low intrarenal pressure, a simple gravity irrigation using saline should be used with a pressure of no more than 40 cm water (30 mmHg). The outflow can be enhanced by using a ureteral access sheath (UAS). As the laser fiber is 2–2.5 m long, for asepsis and safe handling it should be placed on the working table with saline soaked compresses or gauze on top of the fiber. Its weight will stabilise the fiber. The equipment set-up should allow the radiology C-arm and endoscopic tower to be on the contralateral sides.
Use and ergonomics of the equipment (safety wire, ureteral access sheath)
Guide wires are helpful to get access in the renal collecting system and for passage of scopes and stents. Typically, guide wires have a flexible tip, low friction and a rigid shaft. A ureteral access sheath (UAS) is increasingly used for treatment of large renal stones (10). Whilst it facilitates multiple scope passages, it also helps to reduce the intrarenal pressure thereby improving flow and visibility. Studies have shown a reduction of infectious complications with its use (11).
The selection of UAS is based on the clinical necessity, patient anatomy, type and size of the ureteroscope used as well as surgeon’s preference (12). Intrarenal pressure depends on the inflow via the working channel (typically 3.6 Fr), and outflow via the residual space between the ureteroscope and wall of UAS. It is recommended to use a smaller size UAS and not to apply force while placing it. While it aids flexible URS, care must be taken to ensure its safe placement avoiding injury to the ureter. Long-term use of UAS has a theoretical risk of ureteric stricture although this has not been proven in a recent paediatric study (13). The tip of UAS should be either just below pelviureteric junction (PUJ) or in the upper ureter. If UAS placement encounters resistance, then the scope should either be placed over the guide wire or a temporary ureteral stent is inserted for a secondary URS procedure at a later date (14,15).
Ureteral orifice access
Ureteral access is an important step in endourology and must be done safely. We recommend placement of a safety wire via a cystoscope first. Once the position is confirmed, a semi-rigid URS (R-URS) is then carried out over a working wire using the dominant hand (16,17). If the ureteric orifice (UO) is tight or difficult to access, rotate the scope 90°–180° at the UO to help with access. Semi-rigid URS allows a natural dilatation of the UO and the ureter along with identification and treatment of ureteric stones. Besides, mapping the ureter allows an estimate of the possibility and size of UAS that can be inserted.
Flexible scope manipulation
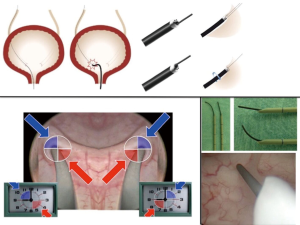
A flexible URS (F-URS) can either be inserted via a UAS or directly over a guide wire. For the later, an angled guidewire is helpful (Figure 2). Scope manipulation uses a combination of rotation, deflection and in/out movement (Figure 3). With the dominant hand pronation and supination is used to change the direction of the tip of the scope, supination is useful when the scope is in the right renal cavities and pronation is useful when the scope is in the left renal cavities. The exploration of the collecting system is begun with the upper calices followed by middle and lower calices.
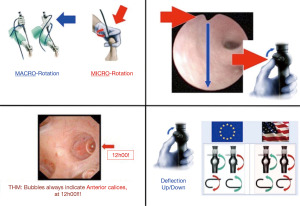
While the macro rotation happens through the dominant hand with scope manipulation, the micro rotation happens with the non-dominant hand at the urethral meatus (Figure 4). The black triangle on the screen denotes the 12 o’clock position and bubble reflects anterior calyces and can be especially useful when using digital F-URS (Figure 4). The scope deflection is also different for the scopes marketed in Europe and USA, whereas deflecting the scope up the tip of scope goes down in Europe, it goes up in USA and vice versa (Figure 4).
Improving vision
Vision is the key for achieving good results during URS and there are certain tricks to improving it. Focusing the scope, adjusting brightness and white balance is the key before beginning the procedure. UAS enhances irrigation and potentially provides a better vision. Similarly, use of pressure irrigation devices can also help improve vision although it should be used carefully and judiciously to avoid complications related to haemorrhage and infections (18-20). Contrast can be useful to clear debris, blood or dust during the procedure and improve vision, although sometimes it might helpful to be patient and wait for the vision to improve naturally. The newer digital scopes also offer a better vision than the older fiberoptic scopes (21).
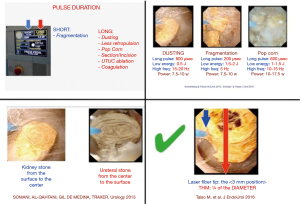
Laser use and settings
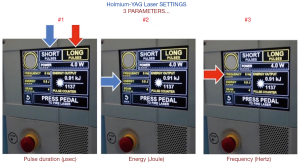
Lasers play a big role in modern endourology with holmium:yttrium-aluminum-garnet (Ho:YAG) proving its safety and efficacy over the last 2 decades (22). Pulse duration, energy and frequency can all be adjusted to either fragment, dust or popcorn the stone (Figures 5,6). While ureteral stones are treated from center to surface, kidney stones are treated from the surface to the center. Fragmentation uses a short pulse duration with high power and low frequency, dusting uses a long pulse duration with low power and high frequency, and popcorning uses a long pulse duration with relatively high power and frequency. Recently, pop-dusting (0.3–0.6 J and a frequency of 20–50 Hz) has also gained momentum which can treat large stones in a single setting (23).
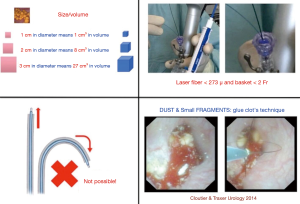
Stone clearance
Irrespective of the technique is used for lasering the stone, it must be remembered that stone volume is not proportionate to the diameter (Figure 7). Larger stones have significantly larger volumes, and this should be recognised while counselling patients for their treatment. It is therefore practically impossible to remove all stone fragments while treating larger stones.
While treating lower pole stones, it might be beneficial to reposition the stone to a more accessible place such as the upper pole before it is treated. In case the stone cannot be repositioned, the laser fiber should ideally be introduced in an undeflected (straight) scope and the F-URS deflected after the fiber is at the tip of the scope (Figure 7). This technique avoids the potential for scope damage although with the disposable scopes and the ball-tip laser fiber the risk is minimised and it is possible to insert the fiber in a deflected scope, albeit at a higher cost (22,24,25). It is also possible to insert the laser fiber and the basket simultaneously via the working channel of the F-URS. After the procedure is completed, the glue-clot technique (24,26) allows the autologous blood to seal the lower pole and to remove the dust and small fragments which become trapped in the clot.
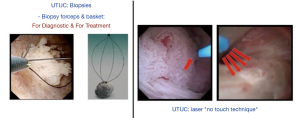
URS for upper tract TCC
Ureteric biopsy has gained importance in the last two decades and correct characterisation seems to be fundamental for diagnosis and patient selection for endoscopic management (8,27,28) (Figure 8). For papillary lesions, the nitinol basket achieves a good histological characterisation (27). Even tumours >1 cm and multifocal tumours can be managed conservatively with laser photoablation (8).
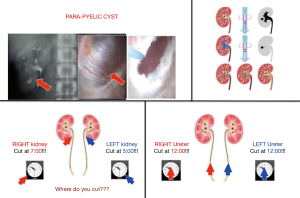
Use of URS in special situations
Flexible URS has been used to treat parapelvic cysts, calyceal diverticuli and ureteric/PUJ strictures (29-31). Once the F-URS is in the renal pelvis, the cyst is identified, and incision and drainage of renal cyst wall is done with a laser (29) (Figure 9). A post-incision ureteric stent is placed in the cyst and removed after 4 weeks. For a diverticulum, contrast with indigo carmin is injected to identify the diverticular neck under fluoroscopic guidance. Once the collecting system is washed with saline, the leakage of dye from the diverticulum is seen endoscopically and the neck of the diverticulum is incised with a laser (14,24). For ureteral stricture, this needs to be located and a full-thickness incision into fat is performed. To avoid vascular injury this is done posterolaterally for proximal stricture and anteromedially for distal strictures (30,31) (Figure 9).
Strengths, limitations and areas of further research
While there are a few reviews on tips and tricks of F-URS, a pictorial guide helps to explain the steps and provides a better understanding of the procedure. These technical principles are our own suggestions and there may be other effective ways to accomplish many of the tips and tricks’ we describe. Although we have tried to explain the important steps, we were not able to explain the procedure on its entirety. This is not a step-by-step guide for how to perform URS, rather an opportunity to refine technical steps of the procedure. It has been shown that URS is more cost effective than shockwave lithotripsy but in future more needs to be done for simulation-based training in URS so that the training is standardised, and this translates into better clinical outcomes (32,33).
Conclusions
Flexible URS has revolutionised the treatment of kidney stones with expanding indications and safer outcomes. We hope that these ‘tips and tricks’ will help in guiding endourologists for an effective and safe treatment for upper urinary tract surgery.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Marshall VF. Fiber optics in urology. J Urol 1964;91:110-4. [Crossref] [PubMed]
- Bagley DH. Ureteral endoscopy with passively deflectable, irrigating flexible ureteroscopes. Urology 1987;29:170-3. [Crossref] [PubMed]
- Rukin NJ, Siddiqui Z, Chedgy E, et al. Trends in Upper Tract Stone Disease in England: Evidence from the Hospital Episodes Statistics (HES) Database. Urologia Internationalis 2017;98:391-6. [Crossref] [PubMed]
- Ishii H, Couzins M, Aboumarzouk O, et al. Outcomes of systematic literature review of Ureteroscopy for stone disease in the Obese and Morbidly Obese Population. J Endourol 2016;30:135-45. [Crossref] [PubMed]
- Somani BK, Robertson A, Kata SG. Decreasing cost of Flexible ureterorenoscopic procedures: Cost volume relationship. Urology 2011;78:528-30. [Crossref] [PubMed]
- Somani BK, Giusti G, Sun Y, et al. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: The Clinical Research Office of Endourological Society URS Global Study. World J Urol 2017;35:675-81. [Crossref] [PubMed]
- Somani BK, Dellis A, Liatsikos E, et al. Review of diagnosis and management of Urolithiasis in Pregnancy: An ESUT practical guide for Urologists. World J Urol 2017;35:1637-49. [Crossref] [PubMed]
- Villa L, Capitanio U, Haddad M, et al. Which patients with upper tract urothelial carcinoma can be safely treated with conservative treatment by flexible ureteroscopy with Holmium: YAG laser photo ablation? Long-term results from a high-volume institution. J Urol 2018;199:66-73. [Crossref] [PubMed]
- Tsivian A, Tsivian M, Stanevsky Y, et al. Routine diagnostic ureteroscopy for suspected upper tract transitional-cell carcinoma. J Endourol 2014;28:922-5. [Crossref] [PubMed]
- Geraghty RM, Ishii H, Somani BK. Outcomes of flexible ureteroscopy and laser fragmentation for treatment of large renal stones with and without the use of ureteral access sheaths: Results from a university hospital with a review of literature. Scand J Urol 2016;50:216-9. [Crossref] [PubMed]
- Traxer O, Wendt-Nordahl G, Sodha H, et al. Differences in renal stone treatment and outcomes for patients treated either with or without the support of a ureteral access sheath: The Clinical Research Office of the Endourological Society Ureteroscopy Global Study. World J Urol 2015;33:2137-44. [Crossref] [PubMed]
- De Coninck V, Keller EX, Rodríguez-Monsalve M, et al. Systematic review of ureteral access sheaths: facts and myths. BJU Int 2018;122:959-69. [Crossref] [PubMed]
- Anbarasan R, Griffin S, Somani BK. Outcomes and long-term follow-up with the use of ureteral access sheath (UAS) for paediatric ureteroscopy and stone treatment: Results from a tertiary endourology centre. J Endourol 2019;33:79-83. [Crossref] [PubMed]
- Doizi S, Traxer O. Flexible ureteroscopy: technique, tips and tricks. Urolithiasis 2018;46:47-58. [Crossref] [PubMed]
- Traxer O, Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of ureteral access sheath during retrograde intrarenal surgery. J Urol 2013;189:580-4. [Crossref] [PubMed]
- Whitehurst LA, Somani BK. Semi-rigid ureteroscopy: indications, tips and tricks. Urolithiasis 2018;46:39-45. [Crossref] [PubMed]
- Veneziano D, Ahmed K, Van Cleynenbreugel BSEP, et al. Development methodology of the novel Endoscopic stone treatment step 1 (EST s1) training/assessment curriculum. J Endourol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Whitehurst L, Jones P, Somani BK. Global mortality of kidney stone disease over the last two decades. A systematic review of literature. World J Urol 2018. [Epub ahead of print]. [Crossref]
- Whitehurst LA, Somani BK. Perirenal haematoma after ureteroscopy: A Systematic review. J Endourol 2017;31:438-45. [Crossref] [PubMed]
- Proietti S, Dragos L, Somani BK, et al. In vitro comparison of maximum pressure developed by irrigation systems in a kidney model. J Endourol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Zilberman DE, Lipkin ME, Ferrandino MN, et al. The digital flexible ureteroscope: in vitro assessment of optical characteristics. J Endourol 2011;25:519-22. [Crossref] [PubMed]
- Kronenberg P, Somani B. Advances in lasers for the treatment of stones – A systematic review. Curr Urol Rep 2018;19:45. [Crossref] [PubMed]
- Pietropaolo A, Jones P, Whitehurst L, et al. Role of 'dusting and pop-dusting' using a high-powered (100 W) laser machine in the treatment of large stones (≥ 15 mm): prospective outcomes over 16 months. Urolithiasis 2019;47:391-4. [Crossref] [PubMed]
- Somani BK, Aboumarzouk O, Srivastava A, et al. Flexible ureterorenoscopy: Tips and tricks. Urol Ann 2013;5:1-6. [Crossref] [PubMed]
- Haddad M, Emiliani E, Rouchausse Y, et al. Impact of the curve diameter and laser settings on laser fiber fracture. J Endourol 2017;31:918-21. [Crossref] [PubMed]
- Cloutier J, Cordeiro ER, Kamphuis GM, et al. The glue-clot technique: a new technique description for small calyceal fragments removal. Urolithiasis 2014;42:441-4. [Crossref] [PubMed]
- Breda A, Territo A, Sangueloce F, et al. Comparison of biopsy devices in upper tract urothelial carcinoma. World J Urol 2019;37:1899-905. [Crossref] [PubMed]
- Rai BP, Shelley M, Coles B, et al. Surgical management for upper urinary tract transitional cell carcinoma (UUT-TCC): a systematic review. BJU Int 2012;110:1426-35. [Crossref] [PubMed]
- Mao X, Xu G, Wu H, et al. Ureteroscopic management of asymptomatic and symptomatic simple parapelvic renal cysts. BMC Urol 2015;15:48. [Crossref] [PubMed]
- Elmussareh M, Traxer O, Somani BK, et al. Laser Endopyelotomy in the Management of Pelviureteric Junction Obstruction in Adults: A Systematic Review of the Literature. Urology 2017;107:11-22. [Crossref] [PubMed]
- Lucas JW, Ghiraldi E, Ellis J, et al. Endoscopic management of ureteral strictures: an Update. Curr Urol Rep 2018;19:24. [Crossref] [PubMed]
- Geraghty R, Jones P, Herrmann T, et al. Ureteroscopy is more cost effective than shock wave lithotripsy for stone treatment: systematic review and meta-analysis. World J Urol 2018;36:1783-93. [Crossref] [PubMed]
- Veneziano D, Ploumidis A, Proietti S, et al. Evolution and Uptake of the Endoscopic Stone Treatment Step 1 (EST-s1) Protocol: Establishment, Validation, and Assessment in a Collaboration by the European School of Urology and the Uro-Technology and Urolithiasis Sections. Eur Urol 2018;74:401-2. [Crossref] [PubMed]