Knowledge of front-line health workers on the role of urethral catheterization for primary prevention of obstetric fistula in Ibadan, Nigeria
Introduction
Female genital fistula is the abnormal communication of the urinary tract with the genital tract and/or the rectum resulting in continuous leakage of urine and/or faeces (1). The aetiology could be obstetrics or gynaecologic. Gynaecological fistula can occur following pelvic surgery, rape, female genital mutilation, infection, genital malignancy and irradiation. However, obstetric fistula (OF) is more prevalent in low- and middle-income countries and remains a public health challenge (1,2). The main cause of OF is prolonged obstructed labour (POL) which reflects the poor state of emergency obstetric care (EmOC) in developing nations. Available global estimates suggest that more than 2 million women live with OF and every year, about 80,000 to 100,000 new cases are detected with the largest burden in sub-Saharan Africa and South Asia (1). Nigeria alone has over 1 million women affected with different types of OF with an annual incidence of 2.11 per 1,000 birth (1). Studies in Nigeria showed that there are more OF cases in northern region than the south with the higher prevalence in the north associated with early marriage, poor access to healthcare services, and higher childbirth rate with non-orthodox practitioners (3,4).
OF has been described as a proxy measure of quality maternity healthcare services (5,6). Evidence abounds that OF tends to be prevalent where there are indicators of poor-quality maternity care services such as inadequate skilled human resources for early detection of mechanical obstruction in labour, non-availability of effective tools to make decision and promptly intervene, poor referral within the health system and lack of facility to offer timely EmOC service (7,8). Another important intervention which has also offered convincing result in preventing OF is early catheterization of bladder for 10–14 days following prolonged and/or obstructed labour. Bladder catheterization ensures continuous urine drainage, improve blood perfusion and tissue regeneration leading to subsequent prevention of bladder tissue necrosis and sloughing. Urinary catheterization can be for primary prevention of OF if performed immediately following prolonged and/or obstructed labour, prior to assisted instrumental vaginal delivery or caesarean section and a secondary prevention as early treatment for OF without the need for surgery if the OF is very small (9,10). Studies have reported 15.4% to 25% of OF closing without surgery if early catheterization is instituted (10-12). To this effect, in order to reduce the burden of OF through prevention and early catheter treatment Nigeria adopted a national guideline on bladder catheterization which should be offered by health workers—doctors, midwives, nurses, community health workers (CHWs) without expertise in fistula repair so as to ensure prevention and easy access to immediate treatment even at the nearest community health centre (10,13,14).
In general, epithelialization of bladder after injury takes about 4 days for healing of the lining of the luminal surface and this is usually completed by 14 days following surgical repair (15,16). However, the process of bladder re-epithelialization might take longer period following conservative management depending on the complexity of the injury (15-17).
The re-epithelialization process involves activation of inflammation, proliferation, and tissue remodelling following the production of collagen and extracellular matrix proteins (18). Most crucial is the combination of migration and proliferation of cells into the wound from the wound edges which later differentiates into umbrella cells within few days and covers the wound (18).
The knowledge of health care workers on OF is crucial to planning advocacy for identification of potential precursors and triggers, promote positive behavioural values that limit the burden, associated social and psychological challenges in the community (10,19).
Much as this sounds relevant, there are limited publication on the knowledge and perspective of health workers in preventing this health challenge. A recent study in Ethiopia which was conducted among 548 nurses and midwives showed that a third of the SBAs lacked appropriate knowledge and skills needed for preventing OF (20). However, about eight out of ten interviewed were aware that bladder catheterization could prevent OF. One of the drawbacks of this study is that it did not provide any information on the use of catheter to primarily prevent OF after prolonged and or obstructed labour.
To the best of our knowledge, there is no published article in Nigeria till date on the knowledge of health care providers on the role of bladder catheterization as a primary measure to prevent OF despite the huge burden of the disease. This is vital because we operate task-shifting and task sharing policy with the CHWs involved in providing basic emergency obstetric and neonatal care (BEmONC) in primary health care centres (PHC) in order to increase access to health services and reduce maternal and neonatal morbidity and mortality (21).
In order to address this critical research gap, this study aimed to determine the knowledge of different cadres of healthcare workers who provide mainly obstetrics care and associated factors on the role of bladder catheterization as a primary prevention of OF.
Methods
This was a cross sectional study conducted among 147 health workers in different public health facilities in Ibadan. The health workers that participated in the study were: community health extension workers (CHEWs), community health officer (CHO), nurses and midwives that provided obstetrics care in the labour and post-delivery wards in primary health centres in Ibadan, Oyo State. The CHOs and CHEWs are PHC community health professionals who had undertaken a standard training programme and are certified to provide basic medical and preventive care by identifying and providing care to pregnant women during antenatal, intrapartum and postnatal period. They also promote access to health services, provide health education, and promote advocacy for prevention of diseases (21,22).
Ten primary health centres were selected by simple random sampling from each local government areas in Ibadan city to ensure equal representation that will provide a generalisable result. Specifically, we choose five urban and five peri-urban local government areas. A self-administered questionnaire on socio-demographic and professional characteristics, and preventive measures of OF using catheterization was used to collect information. We allowed participant to answer the questions privately to allow for anonymity and to prevent interviewer bias. All consenting health worker who were working in the labour and post-delivery wards and were on duty during the study period in the selected primary health centres were included in the study. Data collection tool was adapted from the structured questionnaire for knowledge assessment on OF prevention using catheterization formulated by Engender Health/Fistula Care (10,19).
In this study, awareness of catheterization for prevention of OF was defined as the ability of the participant to identify that catheterization is one of the preventive measures of OF with a positive response (yes) while the knowledge was measured using a three-point scale question with each scored as 1. A score of 1 and 2 was considered as poor knowledge while 3 was considered as good knowledge.
Data were entered and analysed using SPSS version 20. Participants who had correct responses to all questions were classified as having good knowledge. This was based on Banke-Thomas et al. study on knowledge of OF prevention amongst young women in which correct responses of >50% indicated good knowledge (6). We used higher cut-off for good knowledge in this study because our participants—health care workers are expectedly to be more knowledgeable than women in the community that was used in the previous study (6).
We used mean and standard deviation (SD) to summarize continuous variables while categorical variables were summarized with frequencies and percentages. Chi-square test was used to determine the association between good/poor knowledge of health worker and the independent variables. The odds ratio was used to measure the association between educational level, and the knowledge (good/poor) of health worker and its precision was estimated using 95% confidence intervals. Logistic regression was used to assess factors that independently influence knowledge of participants on catheterization for OF prevention and findings were reported with adjusted odds ratio and confidence intervals. Since we were interested in the knowledge of the healthcare workers according to their cadre, we put the cadre into our final model. Statistical significance was set at P<0.05.
Ethical approval was obtained from the Oyo State ethical committee and further permission secured from the Oyo state Primary healthcare board secretary. A written consent was obtained from each participant before the questionnaire was administered stating their approval to participate in the study and permission to use the data for publication.
Results
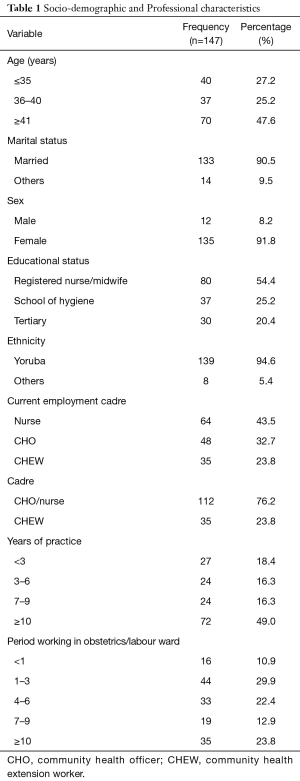
The mean age of participants was 41.6 (SD =8.9) years and almost half (47.6%) were equal or more than 41 years of age. Majority of the participants were married 133 (90.5%) and almost all were females 135 (91.8%). Of the 147 health workers, 64 (43.5%) were nurses, 48 (32.7%) were CHOs while 35 (23.8%) were CHEWs. Majority of the 147 health workers were CHO/nurses (76.2%), while 35 (23.8%) were CHEWs. Almost half (49.0%) of the participants had been practicing for equal or more than 10 years, 18.4% had been working for less than 3 years while participants that had been working for 3–6 and 7–9 years were 16.3% each (Table 1).
Full table
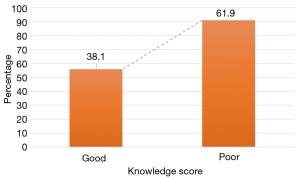
Overall, 38.1% of the health workers had good knowledge while 61.9% had heard of the use of catheterization as a primary prevention of OF (Figure 1). There was higher proportion (40.5%) of those with good knowledge among the health workers aged 36–40 years compared to those aged ≤35 and ≥41 years have good knowledge. The registered nurses and/or midwives had a higher proportion (41.3%) with good knowledge of catheterization compared to those who attended school of hygiene (35.1%) and those with degree in nursing (33.3%). The respondents who functioned as nurses/midwives and CHOs had a higher proportion (41.1%) with good knowledge of catheterization compared to the CHEWs. Higher proportion (42.9%) of healthcare workers who had spent some period working in the labour or post-delivery/post-natal ward for ≥10 years had good knowledge of catheterization compared to those who had spent 4–6 years (42.4%), <1 year (37.5%), 7–9 years (36.8%) and 1–3 years (31.8%) (P=0.853). A higher proportion of respondents who had practiced for between 7–9 years (58.3%) had good knowledge of catheterization in preventing OF compared to those who had practiced for ≥10 years (38.9%), 3–6 years (37.5%) and <3 years (18.5%) (P=0.035) (Table 2).

Full table
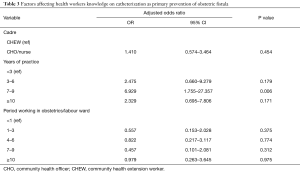
Though not significant on the bivariate analysis, cadre and years of working in obstetrics/labour ward were included in the regression model along with years of practice. CHO/nurses were about twice more likely to have good knowledge of catheterization compared to CHEWs (AOR =1.410, 95% CI, 0.574–3.464). Health workers who had practiced for 7–9 years were about seven times more likely to have good knowledge of catheterization compared to those who had worked for less than three years (OR =6.929, 95% CI, 1.755–27.357) (Table 3).
Full table
Discussion
This study provided information on the assessment of a critical section of front-line healthcare providers in the community on OF. Nurses and CHEWs offered consultation, treat and take vaginal deliveries at the primary healthcare centres in Nigeria, the usual first point of call to seek information or care for medical ailments (23-25). The main finding from this study was that CHO/nurses were more likely to have good knowledge of catheterization compared to CHEW (AOR =1.4) and healthcare providers (both nurses and CHWs) with 7–9 years of medical practice were more likely to have better knowledge on use of bladder catheterization as a primary prevention intervention for OF. Surprisingly, years of practice in obstetric and labour work was not found to influence their knowledge. We also found out that nurses and CHO generally had better knowledge than CHEWs. This might not be unrelated to their training, the nurses/midwives has a more detailed training of 3 to 5 years depending on the degree obtained while the CHEWs are trained for 2 years and CHOs for 3 years on simple but scientifically sound and culturally acceptable methods and skills in prevention, promotion, rehabilitation and or treatment of health conditions in the population or community in reference to their basic needs (21,22). Nevertheless, the CHWs have contributed significantly to reduction of maternal morbidities and mortalities in Nigeria with visible improvement in the utilization of maternal health services leading to an overall reduction of 27% in the maternal malnutrition status (22,24).
The outcome of our study corroborates an Ethiopian study that reported high knowledge of bladder catheterization in preventing OF (20). The high knowledge observed among nurses might reflect robust in-service training in childbirth nursing care as well as practical exposure before and after graduation from school. It also plausible that majority of nurses might have also worked in busy maternity centres where there is clear protocol of managing women with prolonged and/or obstructed labour. This preventive measure often forms part of integral role of nurses in labour ward. In Nigeria, it is given that any nurse that is working in labour ward would have had a mandatory formal midwifery training of at least a year in Nigeria. According to the Nigerian national policy on primary healthcare, CHWs are permitted to offer service in primary healthcare centres to complement nurses, yet the reality in the country is that they form the bulk of healthcare providers at this level of service delivery (23). A survey in 2009 revealed 36,737 CHWs working in the PHCs with only 5,604 doctors, nurses and midwives in Nigeria and 90% of deliveries at the health facilities are conducted by the CHEWs (21). This suggest that the bulk of obstetric care in PHCs are provided by CHWs. Therefore, there is the need to ensure a non-compromising performance with good obstetric outcomes. It is imperative that a pre and in-service competency-based training on catheter insertion and management in relation to OF prevention is popularised and supported at all maternal health training points.
The poor knowledge by a significant proportion of study participants is source of concern particularly in a setting where the prevalence of prolonged and or obstructed labour is very high, and it constituted a significant proportion of maternal morbidity and mortality (26,27). Furthermore, the poor knowledge might also be reflection to lack of access to the national policy and protocols and continuous medical training on the role of bladder catheterization in the prevention of obstructed labour. In 2016, the Federal Ministry of Health launched a national document and subsequently integrated bladder catheterization into the EmOC training curriculum for healthcare providers including nursing and CHWs (23). The motive behind this document is to promote primary prevention OF using effective cheap technology.
To our knowledge, this is probably the first published study in Nigeria that assessed this subject, but we will like to caution on the interpretation of the study. First, the study did not ask question on previous training of bladder catheterization in preventing OF. Our assumption was based on the common knowledge that every healthcare worker would have had training on it as part of obstetric training. Secondly, we also did not ask question on whether they have seen the national policy and training curriculum on EmOC. Lastly, we did not ask question on their previous involvement on management of OF or how they currently manage cases of prolonged/obstructed labour. Despite all these, our findings provided a rear opportunity for a wake-up call to address the observed knowledge gap to address a simple but strategic intervention that could potentially prevent further escalation of an already huge burden of OF in Nigeria. It is also important to seek information on the use of partograph in the primary healthcare settings as a way to promptly detect and refer all cases of obstructed labour early.
Conclusions
This study showed a moderate knowledge score among healthcare workers in primary healthcare settings in Nigeria with higher proportion of those with good knowledge being nurses or CHOs with long period of practice. There was no difference in knowledge score according to the cadre of the health workers interviewed. We advocate better integration of bladder training in the curriculum of potential health workers offering maternity care services in our setting. Re-training to update knowledge and skills is also a necessity.
There is increased need for training and re-training of health workers in primary PHC in low resource settings on the vital role of fistula prevention through catheterization immediately following obstructed labour, prior to assisted vaginal delivery and caesarean delivery.
Acknowledgments
We thank Mrs. Tolulope Babawarun who provided statistical analysis support for this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from the Oyo State ethical committee and further permission secured from the Oyo state Primary healthcare board secretary (No. AD/13/479/902B). A written consent was obtained from each participant before the questionnaire was administered stating their approval to participate in the study and permission to use the data for publication.
References
- Lewis G, de Bernis L. Obstetric Fistula. Guiding Principles for Clinical Management and Programme Development. Geneva, Switzerland: World Health Organization; 2006. Available online: http://www.who.int/iris/handle/10665/43343. Accessed 28 Jan 2016.
- Kelly J. Outreach programmes for obstetric fistulae. J Obstet Gynaecol 2004;24:117-8. [Crossref] [PubMed]
- Ijaiya MA, Rahman AG, Aboyeji AP, et al. Vesicovaginal fistula: a review of Nigerian experience. West Afr J Med 2010;29:293-8. [PubMed]
- Nigeria demographic health survey (NDHS). NDHS Final Report, 2013. Available online: Accessed 28 Dec 2016.https://dhsprogram.com/pubs/pdf/fr293/fr293.pdf
- Ijaiya MA, Aboyeji PA. Obstetric urogenital fistula: the Ilorin experience, Nigeria. West Afr J Med 2004;23:7-9. [Crossref] [PubMed]
- Banke-Thomas AO, Kouraogo SF, Siribie A, et al. Knowledge of Obstetric Fistula Prevention amongst Young Women in Urban and Rural Burkina Faso: A Cross-Sectional Study. PLoS One 2013;8:e85921. [Crossref] [PubMed]
- Mselle LT, Kohi TW, Mvungi A, et al. Waiting for attention and care: birthing accounts of women in rural Tanzania who developed obstetric fistula as an outcome of labour. BMC Pregnancy Childbirth 2011;11:75. [Crossref] [PubMed]
- Mselle LT, Kohi TW. Perceived Health System Causes of Obstetric Fistula from Accounts of Affected Women in Rural Tanzania: A Qualitative Study. Afr J Reprod Health 2015;19:124-32. [PubMed]
- Ali A, Masakhwe BA. WHO midwifery education module 3: Managing prolonged and obstructed labour. Geneva Foundation for Medical Education and Research. 2010 Jul 18. Available online: http://www.gfmer.ch/SRH-Course-2010/assignments/Managing-prolonged-obstructed-labour-Ali-Masakhwe-2010.htm
- Fistula Care. Urinary Catheterization for Primary and Secondary Prevention of Obstetric Fistula: Report of a Consultative Meeting to Review and Standardize Current Guidelines and Practices, March 13-15 at the Sheraton Hotel, Abuja, Nigeria. New York: EngenderHealth/Fistula Care, 2013. Available online: http://pdf.usaid.gov/pdf_docs/PA00JFDJ.pdf. Accessed14 Jul 2016.
- Waaldijk K. The immediate management of fresh obstetric fistulas. Am J Obstet Gynecol 2004;191:795-9. [Crossref] [PubMed]
- Waaldijk K. The immediate surgical management of fresh obstetric fistulas with catheter and/or early closure. Int J Gynaecol Obstet 1994;45:11-6. [Crossref] [PubMed]
- Nigeria Ministry of Health. (Nigeria MOH), National Strategic Framework for the Elimination of Obstetric Fistula in Nigeria: 2011-2015. Abuja, Nigeria. 2012. Available online: https://fistulacare.org/archive/files/5/5.4/Nigeria_National_Strategy_2011-2015.pdf. Accessed: 26 Feb 2019.
- Nigeria Federal Ministry of Health. (Nigeria FMOH). Guidelines on Urethral catheterization for Prevention and Management of Obstetric fistula in Nigeria, 2016.
- Obara T, Matsuura S, Narita S, et al. Bladder acellular matrix grafting regenerates urinary bladder in the spinal cord injury rat. Urology 2006;68:892-7. [Crossref] [PubMed]
- Sutherland RS, Baskin LS, Hayward SW, et al. Regeneration of bladder urothelium, smooth muscle, blood vessels and nerves into an acellular tissue matrix. J Urol 1996;156:571-7. [Crossref] [PubMed]
- Reddy PP, Barrieras DJ, Wilson G, et al. Regeneration of functional bladder substitutes using large segment acellular matrix allografts in a porcine model. J Urol 2000;164:936-41. [Crossref] [PubMed]
- Larsson P, Chamorro CI, Fossum M. Review on Bladder Wound Healing after Mechanical Injury. J Tissue Sci Eng 2016;7:170. [Crossref]
- Fistula Care. Prevention and recognition of obstetric fistula training package: Participant handbook. Chapel Hill, NC: Fistula Care/IntraHealth International, 2012. Available online: Accessed 18 Jul 2016.https://fistulacare.org/wp-fcp/wp-content/uploads/pdf/Training/prevention_recognition_obfistula-facilitatormanual_final_february2012.pdf
- Legesse M. Knowledge and practice on prevention of obstetric fistula among skilled birth attendants in public health centers in Addis Ababa, Ethiopia. Int J Dev Res 2016;6:10072-9.
- Task-Shifting and Task sharing Policy for Essential Health Care Services in Nigeria. Federal Ministry of Health, August 2014. Available online: https://advancefamilyplanning.org/sites/default/files/resources/Nigeria%20taskshifting%20policy-Aug2014%20REVISEDCLEAN%20_Approved%20October%202014.pdf. Accessed 25 Feb 2019.
- Ibama AS, Dennis P. Role of Community Health Practitioners in National Development: The Nigeria Situation. Int J Clin Med 2016;7:511-8. [Crossref]
- National Primary Health Care Development Agency, Nigeria. Integrated Training Manual for Primary Health Care (PHC) Workers in Nigeria, 2017.
- Deller B, Tripathi V, Stender S, et al. Task shifting in maternal and newborn health care: key components from policy to implementation. Int J Gynaecol Obstet 2015;130 Suppl 2:S25-31. [Crossref] [PubMed]
- Federal Ministry of Health. Modified Life Saving Skills (MLSS) for Community Health Extension Workers/Community Health Officers (CHEW/CHO); January, 2014.
- Federal Ministry of Health. The Participant Training Manual on Life Saving Skills (LSS) for Nurses/Midwives; January, 2014.
- World Health Organization (WHO). In: Obstetric fistula: guiding principles for clinical management and program development, 2006. Available online: http://whqlibdoc.who.int/publications/2006/9241593679_eng.pdf. Accessed 3 Feb 2016.