Frontiers in hormone therapy for male infertility
Introduction
The inability to conceive a child is a distressing reality for a significant number of couples worldwide. After 12 months of unprotected intercourse, it is estimated that approximately 10–15% of couples fail to conceive offspring (1-3). Male factor infertility contributes to 50–60% of overall infertility but is solely responsible in only 20% of couples. Male factor infertility can be due to identifiable hormonal or anatomical etiologies that may be reversible or irreversible. However, a significant portion of men presenting with infertility have no underlying identifiable cause—or one that continues to elude our diagnostic capabilities. In reality, this remains an astounding figure with idiopathic infertility comprising 25–50% of men presenting with fertility challenges (2,3).
The literature regarding the use of empirical medical therapies for men with hypogonadism and/or idiopathic infertility remains inconclusive (1). The fact that there is no current clear consensus on the management of idiopathic oligospermia, for example, likely reflects our failure to fully comprehend and define the precise etiologies underlying idiopathic male infertility (4). With few exceptions, none of the empiric therapies used to treat idiopathic male infertility have been shown to be effective in repeat, randomized, controlled studies (3). Nevertheless, prior to the initiation of hormonal therapy for the treatment of male factor infertility, a careful work-up is imperative to rule-out any reversible causes.
In this review article, we will assess the literature regarding correlations between aberrations in a patient’s hormonal milieu and their subsequent impact on fertility. Along with bringing to light any reported relationship between such hormones and infertility, we also seek to discuss the potential impact of correcting these deviations and the methods currently available to providers. We admit that some of the data on the role of these hormones and treatments in male fertility is either sparse and/or conflicting. Whereas our primary purpose is to define our current state of the science, in doing so, we hope to delineate potential future research or treatment strategies to ultimately aid the reproductive capacity of these patients. Please refer to Table 1 for a reference of the indications and side effects of the treatments discussed in this review. Furthermore, the preferred doses and regimens prescribed by the senior author are also included in Table 1.
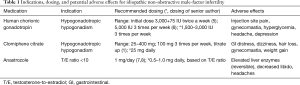
Full table
Clomiphene citrate (Clomid, CC)
CC is a selective estrogen receptor modulator (SERM) that is found in a racemic mixture of two isoforms—enclomiphene and zuclomiphene (2). This class of medications competitively binds to the estrogen receptors on the hypothalamus and pituitary gland thereby negating the negative feedback imposed by estrogen. Luteinizing hormone (LH) secretion is subsequently increased resulting in more testosterone production by the testes (9). The reduced negative inhibition upon the hypothalamus and pituitary gland results in enhanced follicle-stimulating hormone (FSH) secretion subsequently resulting in increased spermatogenesis. Since CC relies on increasing FSH, it will not be effective in patients with an elevated FSH level or in patients lacking a post-treatment FSH surge (2).
CC has not been approved by the Food and Drug Administration (FDA) for administration in men. The use of CC was originally approved for the treatment of ovulatory dysfunction in women; however, many studies have established the safety and efficacy of off-label use of CC for male infertility and hypogonadism (10). Recent surveys by the American Urological Association have shown that estrogen antagonists are the most prescribed medical agents for empiric medical therapy for idiopathic male infertility (11). The optimal dosing of CC has been recommended in doses ranging from 12.5 to 400 mg/day with the ability to administer lower doses attributed to its half-life of 5 days. Several dosing regimens have been suggested including 100 mg 3 times weekly with dosing schedules starting at a low dose of 25 to 50 mg every other day subsequently increasing to 50 mg daily to optimize outcome (1). CC’s effect on hormonal levels or semen analysis parameters is not immediate with the first improvement tending to be an increase in percent motility (1).
The fact that studies evaluating the efficacy of CC date back several decades unveils its potential as an effective therapy for male infertility. In ten patients with idiopathic oligospermia and ten volunteers with normal semen parameters, Masala et al. found that 100 mg of daily CC resulted in marked increases in plasma luteinizing hormone releasing hormone (LH-RH) levels followed by significant increase in testosterone levels. However, no significant differences were seen in the hormonal levels between those with idiopathic oligospermia and those with normal semen parameters (12).
In a prospective study conducted by Ross et al., 53 patients received high-dose, alternate-day CC therapy (100 mg 3 times per week). Overall, a positive response rate of 66% and a pregnancy rate of 26% were observed with significant surges in gonadotropins and testosterone seen in responders. Moreover, it was found that more than 50% of patients responded within the first 3 months of treatment with the rest of the cohort responding after 6–15 months (13). The goal of achieving pregnancy was also observed in 8 of 20 patients (40%) in another study in which men treated with a 6-month trial of intermittent low-dose CC therapy (14). In a prospective, randomized trial, Micic and Dotlic randomized 101 oligospermic men with low to normal FSH levels to receive treatment with 50 mg of CC daily for 6 to 9 months. Significant improvements in semen volume, sperm density and motility were observed in the 56 men randomized to CC therapy versus the 45 controls. Seven pregnancies were observed in the treatment group versus zero in the control group (15).
CC has also been assessed against other hormonal therapies such as gonadotropin releasing-hormone analogues (GnRHa) as a standalone therapy for male factor infertility. Matsumiya et al. prospectively studied the efficacy and adverse effects of GnRHa and CC therapy for treatment of idiopathic normogonadotropic oligoasthenozoospermia (INOA). Forty-four patients with INOA were randomly allocated to treatment with GnRHa or CC. Overall, 23 INOA patients underwent GnRHa therapy with 15 microgram of diluted buserelin acetate given once a day intranasally and 21 INOA patients were treated with 50 mg of CC daily by oral administration. Treatment was well-tolerated amongst both groups; however, compared to baseline semen parameters, those treated with the GnRHa analogue experienced significant (P<0.05) improvements in mean sperm density and mean sperm motility after 3 months of therapy while those treated with CC did not experience any significant changes in semen parameters (16).
The use of estrogen antagonists for treatment of idiopathic male infertility has been supported by two separate meta-analyses. A Cochrane review of 10 studies and 738 men by Vandekerckhove et al. assessed the efficacy of CC or tamoxifen in the treatment of idiopathic oligo and/or asthenospermia. After limiting the review to the five studies that randomized subjects, positive improvements in testosterone levels were identified; however, the overall pregnancy rate was 15.4% compared to a spontaneous rate of 12.5% in control groups. The odds increased to 1.56 when all ten trials were included (17). A meta-analysis reviewing a total of 11 randomized-controlled trials conducted by Chua et al. found the use of estrogen antagonists resulted in statistically significant increases in pregnancy rate compared with controls (P=0.0004) along with significant increases in sperm concentration (P=0.001) and per cent sperm motility (P=0.03). The most significant beneficial effects (P=0.003) were identified in subgroup analysis in those receiving 50 mg daily dosing, however. Furthermore, significant improvements in sperm concentration and motility were identified only within the 50 mg daily dosing subgroup (11). It should be noted that Clomid was the SERM administered in only 5 of the 11 studies reviewed. Moreover, there was inconsistency in dosing, which ranged from 25 to 50 mg per day for treatment durations lasting 3–12 months. Despite some encouraging data reported via these meta-analysis, a subsequent study published by Patel et al. assessing the safety and efficacy of 50 mg every other day dosing of CC on 47 infertile, hypogonadic men demonstrated no significant improvements (P=0.09) in sperm parameters after treatment. As CC use is an off-label therapy for improving fertility in hypogonadal men, parameters for ideal patient selection remain elusive and have not been well-defined.
CC has also shown efficacy when administered prior to sperm retrieval procedures. In a multicenter study that assessed the impact of CC on semen and surgical testicular sperm extraction (TESE), Hussein et al. titrated treatment with CC to achieve testosterone levels between 600 and 800 ng/dL. A total of 42 patients with non-obstructive azoospermia (NOA) were included in the analysis after azoospermia had been confirmed by a previous testicular biopsy. After CC therapy, 64.3% of patients demonstrated sperm in their semen analyses ranging from 1 to 16 million sperm/mL and sufficient sperm for extraction was identified in all patients (18). The improvement in microdissection TESE was further demonstrated in another study spearheaded by Hussein et al. that concluded that patients receiving therapy with CC had a 20–25% greater chance of identifying sperm on micro-TESE compared to those not receiving treatment (19).
CC is generally well tolerated with common side effects including gastrointestinal distress, dizziness, hair loss, gynecomastia and minimal weight gain. Visual disturbances occur in about 1.5% of patients with symptoms such as blurred vision, photophobia and diplopia, which are all reversible with cessation of medication (2,20). Moreover, a retrospective study of 363 hypogonadal men receiving treatment with CC or testosterone replacement therapy (TRT) found that the prevalence of polycythemia to be much less in men treated with CC than TRT with similar improvements in serum T (21). Furthermore, another study of hypogonadal and/or infertile men found no changes in hematocrit levels as well as no changes in prostate-specific antigen during treatment with CC (22).
Certainly the most significant adverse effect and reason to prompt pause in initiating therapy with CC are reported paradoxical reductions in semen quality after treatment. Pasqualotto et al. described a case report of three patients sent to an infertility clinic for evaluation of azoospermia after the use of CC. Prior to treatment with CC, each patient was known to have severe oligospermia with FSH levels within normal limits. Treatment duration with CC ranged from 3–6 months. After being instructed to stop CC therapy for three months, sperm was present in all follow-up semen analyses (23).
Aromatase inhibitors (AIs)
AIs may be used in men with non-obstructive infertility to address the imbalances in testosterone and estrogen levels that affect spermatogenesis. As previously discussed, estrogen exerts negative feedback on the pituitary and hypothalamus to decrease LH and FSH and negatively affect spermatogenesis (24). Estrogen may also directly inhibit spermatogenesis by down-regulation of spermiogenesis related-genes and inducing spermatocyte apoptosis through estrogen-receptors 1 and 2 (25).
Aromatase is a cytochrome P450 enzyme that irreversibly converts androgens to estrogens in various tissues including the testis, liver, brain and adipose (26,27). In the testis, aromatase is localized to the Leydig cells (28). AIs can selectively increase endogenous testosterone levels without increasing circulating estrogens (29,30). Moreover, AIs can be categorized as steroidal or non-steroidal. Steroidal AIs cause irreversible enzyme inhibition by mimicking androstenedione whereas non-steroidal AIs mimic substrates to cause reversible inhibition (31).
The utility of AIs arises from finding that a subset of patients with idiopathic male-factor infertility have abnormal testosterone-to-estradiol (T/E) ratios (32). Pavlovich et al. compared the serum hormonal levels in 63 infertile men to 40 fertile men to identify significant differences in the T/E ratio. It was discovered that men with infertility and fertile men had T/E ratios of 6.9 versus 14.5 (P<0.01), respectively (32). As such, a T/E ratio of 10 was suggested as the lower limit of normal.
Early studies evaluated the efficacy of testolactone in the treatment of idiopathic male infertility with normal hormonal profiles. In 1989, Clark and Sherins treated 25 men with 2 grams per day of testolactone in a randomized double-blind placebo-controlled cross-over trial (33). A significant (P<0.01) decrease in sex hormone-binding globulin of 30% was observed with a corresponding 36% increase in free testosterone levels (P<0.01), Moreover, FSH, LH, and 17α-hydroxyprogesterone all experienced significant (P<0.05) increases by 20%, 15%, and 90%, respectively. However, no changes were found in total testosterone or estrogen levels nor in sperm parameters or pregnancy rates (33). Pavlovich et al. demonstrated that in a subset of 45 infertile men with low T/E ratio, testolactone at daily doses of 100–200 mg was able to significantly correct the T/E ratio (5.0±0.3 to 12.7±1.2, P<0.01). Semen analyses of a further subset of 12 men showed significant increases in sperm concentration (16.1 to 28.9 million, P=0.03) and motility (27.1% to 45.3%, P<0.01) (33). Of note, testolactone is no longer available for clinical use in the United States (27).
Further investigations studied the efficacy of AIs at lower doses, which overall showed improvements in semen parameters in select patients with low T/E ratios. Raman and Schlegel reported favorable effects on spermatogenesis with treatment of testolactone and anastrozole. One hundred and forty subfertile men with abnormal T/E ratios were treated with either 100–200 mg/day of testolactone or 1 mg/day anastrozole. Both groups had improvements in T/E ratios, sperm concentration and sperm motility index. Interestingly, on subset analysis, anastrozole was not found to be more efficacious in the treatment of obese men compared to men of normal weight (34). This phenomenon lead some to hypothesize that the majority of aromatase activity arises from within the testicles and not via peripheral conversion (27). In 2017, Shoshany et al. reported a retrospective study of 86 subfertile men with low T/E ratios treated with 1 mg/day anastrozole. Improvement in T/E ratio (6.98±0.33 to 34.5±6.5) was observed in 95.3% of men. However, improvements in sperm concentration and motile counts were only demonstrated in men with oligospermia but not those with azoospermia, cryptozoospermia, or normospermia at presentation (7).
Similar improvements in T/E ratio, sperm concentration, and sperm motility were seen with treatment with letrozole. Saylam et al. treated 17 azoospermic and 10 oligospermic men with 2.5 mg letrozole daily for greater than 6 months (35). T/E ratios increased in all patients after treatment. Sperm counts and motility were increased for oligospermic men following treatment with 2 of 10 patients subsequently able to achieve pregnancy during the trial period. In a prospective, non-randomized study of 29 infertile men with low serum T/E ratios, treatment with letrozole or anastrozole were found to increase serum T as well as semen parameters including concentration, morphology and motility (8).
The effects of AIs on spermatogenesis have also been investigated. In a single case report of nonobstructive idiopathic azoospermia, daily 2.5 mg letrozole for 4 months was able to convert a patient with hypospermatogenesis to active spermatogenesis proven by testicular biopsy (36). Although pre-treatment estrogen levels were not available for the study, testosterone, LH, and FSH all observed to increase at 1 month following treatment. Furthermore, the efficacy of letrozole to induce spermatogenesis was further supported by two limited case series. Saylam et al. was able to show spermatozoa in the ejaculate of 4 of 17 azoospermic men after 6 months of treatment with letrozole although 13 patients remained azoospermic after treatment (35). In a smaller study of four patients with NOA, Cavallini et al. demonstrated that just 3 months of therapy with letrozole at 2.5 mg/day was able to improve both T/E ratios and induce spermatozoa in the ejaculate (37).
In a randomized double-blind comparison trial, Helo et al. investigated 26 men with hypogonadism and infertility to receive CC or anastrozole. Significantly greater increases T were identified in men receiving CC though anastrozole resulted in significantly larger increases in T/E ratios. Aside from the differences in the hormonal profiles, no significant differences in semen parameters were identified between the groups (38).
AIs are well tolerated at low doses. Side effects occur in less than 10% of patients and are mild. The most finding is a transient elevation of liver enzymes, which resolves with cessation of therapy (32,34). Decreased libido has been reported (26), as well mild headaches that did not require discontinuation of therapy (7). Additionally, there is a possible risk of decreased bone density due to AI treatment (39).
Human chorionic gonadotropin (HCG)
The use of HCG for the treatment of male infertility is most commonly applied to the treatment of patients presenting with hypogonadotropic hypogonadism (HH). The mechanism of action of HCG involves its action as an analogue of LH and its subsequent role in maintaining and/or increasing intratesticular levels of testosterone (40). Several studies with small numbers of subjects have reported its efficacy in restoring spermatogenesis in patients with HH (9,41,42).
In a 30-year retrospective study, Miyagawa et al. assessed treatment outcomes of HH with HCG/human menopausal gonadotropin (HMG). Thirty-six male patients with primary (81%) and secondary (19%) HH were identified and treated with initial doses of 3,000 IU of HCG and 75 IU of HMG twice a week. Pre-treatment testicular volume was found to be the only significant predictor of treatment response defined as sperm production. Specifically, men with a pre-treatment testicular volume of 7.5±3.5 versus 1.6±0.9 cc were 35% more likely to have sperm production after a mean treatment duration of 56 months (43). Similarly, Yang et al. published their 10-year experience in successfully using HCG, HMG or HCG/HMG to treat men presenting with HH. In this study, it was found that a greater percentage of patients treated with HCG/HMG combination therapy had improvements in testicular volumes versus those treated with HCG alone (76% versus 50%, respectively). Moreover, of the patients who experienced testicular growth, approximately 86% of patients treated with HCG/HMG ultimately achieved spermatogenesis compared to 81% in those treated with HCG alone (42).
The consideration of pre-treatment testicular volume prior to administration HCG/HMG in patients presenting with infertility and HH of any etiology was further supported by a retrospective study by Farhat et al. in 87 men presenting with congenital or acquired HH of various etiologies. Pre-therapy testicular volume was a significant (P<0.0001) predictor of response to therapy with responders found to have a mean testicular volume of 9 cc compared to non-responders who had a mean volume of 5.7 cc. However, even in well-selected patients, pregnancy rates after treatment were still modest (41).
Positive results have been demonstrated with HCG-based hormonal stimulation in men with NOA undergoing sperm retrieval by micro-TESE. Shiraishi et al. studied therapy with 5,000 IU HCG 3 times weekly for 3 months in 28 men who had a previous negative attempt at sperm retrieval by micro-TESE. After treatment, it was found that hormonal therapy significantly increased (P<0.05) the chances of sperm retrieval at the time of second micro-TESE compared to men who did not receive treatment. Sperm were retrieved in 6 men (21%) who had undergone hormonal treatment whereas no sperm were retrieved in the control group (5). In a study of 68 men with non-mosaic Klinefelter’s syndrome, Ramasamy et al. found that sperm retrieval rates during micro-TESE did not depend on the preoperative administration of HCG, CC or AIs. Rather, it was observed that patients with a resultant testosterone ≥250 ng/dL had a 22% higher sperm retrieval rate compared to patients with testosterone levels <250 ng/dL (6).
Overall, in treating infertility, HCG therapy is effective; however, cost of therapy precludes regular and widespread utilization (2). Moreover, HCG is typically only effective when serum FSH, LH and/or testosterone levels are low or are in low normal ranges (44).
Prolactin (PRL)
While PRL has long been known to be the hormone responsible for mammary gland development and lactation in females, understanding its role in the male has been elusive. PRL is mainly expressed and secreted by the anterior pituitary lactotroph cells. PRL secretion is primarily under tonic inhibitory control by the hypothalamus through dopamine acting via D2 receptor on lactotrophs (45). Once secreted, the physiologic processes affected by PRL are vast and include mammary gland development, initiation and maintenance of lactation, immune modulation, osmoregulation and behavioral modification (46).
The role of PRL in male health is still widely unknown but there has been data to suggest that PRL positively modulates several aspects of testicular function. PRL receptor expression has been demonstrated in Leydig, Sertoli and in germ cells. PRL can affect steroidogenesis by modulating the expression of LH receptors, or by regulating the activity of steroidogenic enzymes (47,48). Disturbances in spermatogenic processes was demonstrated by Micic et al. who found that serum FSH levels in hyperprolactinemic infertile men were significantly higher compared to infertile men without hyperprolactinemia and healthy, normal fertile men (49). Furthermore, high seminal PRL levels have also been found to negatively impact the functional capacity of sperm (50). In an animal model study, Binart et al. demonstrated that fertility parameters as well as body and reproductive organ weights were unaffected in PRL receptor knockout mice (48). PRL has also been shown to have a potential impact on sexual function including effects on ejaculation, libido and perception of orgasmic experiences (51-53).
The correlation between PRL and infertility is still being investigated and by no means conclusive. The goal of achieving euprolactinemia in men undergoing infertility studies has demonstrated varied outcomes with Nishimura et al. demonstrating that in ten men with serum PRL levels twice the upper limit of normal, no changes in LH, FSH, testosterone or estradiol concentrations or semen parameters were identified before and after treatment with bromocriptine (54). Conversely, Mancini et al. found that treatment with bromocriptine significantly improved sperm counts in 5 of the 8 men presenting with oligozoospermia (55). This small-cohort data conflicts with a later study published by Okada et al. who investigated the effects of hyperprolactinemia on sperm function in 264 men presenting with semen abnormalities and discovered that no correlation between abnormal semen analyses and hyperprolactinemia existed. Furthermore, no changes in sperm concentration, motility or morphology were found after normalization with serum PRL levels (56).
Those with hypoprolactinemia were similarly investigated by Ufearo et al. who found that production of an adequate number of morphologically normal sperm in males may require adequate concentrations of PRL in the blood. In the study, withdrawal of human prolactin (hPRL) or metoclopramide in men with hypoprolactinemia resulted in recurrence of baseline semen abnormalities namely reduced sperm concentration and poor morphology (57).
Overall, the data regarding PRL and its role in male infertility remains inconclusive. What does appear to be more obvious, however, is that routine measurements of serum PRL in infertile men without symptoms of hyperprolactinemia likely offers little value (58).
Thyroid hormones
Infertile men with hyperthyroidism commonly present with decreased libido, erectile dysfunction, premature ejaculation or signs and symptoms of increased estrogen, such as gynecomastia or spider angiomas. Laboratory work-up may demonstrate increase in serum steroid-hormone binding globulin, increased testosterone with a normal free testosterone, increased total and free estradiol, increased progesterone and increased FSH and LH response to exogenous GnRH (59,60). Sertoli cells have been shown to express thyroid hormone receptors (TRs) and thyroid hormones also influence Leydig cell development and steroidogenesis. These findings suggest that thyroid hormones may sustain different populations of germ cells. The clinical manifestation of these observations have been seen in hyperthyroid and hypothyroid men who had a lower proportion of morphologically normal sperm (59,61).
In a study of 25 male patients with active Graves’ disease and 10 normal men, Abalovich et al. demonstrated the deleterious effects of hyperthyroidism on semen analyses with most changes in semen parameters being corrected when euthyroidism was established in these patients (62). Similarly, Krassas et al. found that the only semen parameter noted to be significantly different compared to euthyroid controls was mean motility, which was lower in hyperthyroid males (28%±8% vs. 57%±7%; P<0.01). The hyperthyroid men experienced a significant improvement in motility after treatment (28%±8% vs. 45%±7%; P<0.05) (63).
The literature regarding the effect of hypothyroidism on male semen parameters is scant with Griboff et al. demonstrating an association with decreased libido and erectile dysfunction in a small case series (64,65). In one study involving 24 human male patients with documented hypothyroidism, impaired (P<0.001) semen parameters including poorer sperm count, morphology and motility were observed in those suffering from hypothyroidism compared to normal males (66).
It is evident that hyperthyroidism and hypothyroidism have well-described effects on semen parameters. However, the likelihood that thyroid dysfunction is the sole cause of infertility in affected males is rare (67). Furthermore, studies have supported that screening for thyroid dysfunction in the male population of couples presenting with infertility is low yield and not routinely recommended (68,69).
Future considerations
Several issues have surfaced recently that will likely provide clinicians with new treatment challenges. For instance, there has been significant interest in restoring spermatogenesis after TRT. It has been reported through a recent survey that approximately 25% of urologists have utilized exogenous testosterone to treat patients presenting with infertility associated with low testosterone (4,70). Thus, a rather significant proportion of urologists have directly contributed to the unfavorable effects of TRT on spermatogenesis. Moreover, testosterone usage has markedly increased due to new forms of supplementation, improved consumer advertising and awareness of symptomatic improvement in men receiving TRT (71). Outside the setting of TRT for male infertility, another significant source of exogenous testosterone use has been in the arena of male contraception (72,73). However, regardless of the initial reason for receiving exogenous testosterone, adverse long-term spermatogenic outcomes associated with TRT have presented a challenge for male infertility specialists. The prevalence of obesity continues to have a profound impact on our healthcare system along with a larger cohort of such patients seeking treatment for male infertility (2). The link between varicoceles and fertility is still being explored with initial data seemingly supporting surgical intervention. This section addresses these issues that appear to be the future talking points and/or dilemmas of our ever-evolving field.
TRT and spermatogenesis
In a large multivariate analysis review of 30 studies, Liu et al. established the notion that hormonal male contraceptive regimens are reversible within a predictable time course. Specifically, it was discovered that median times for sperm to recover to thresholds of 20, 10 and 3 million per CC were 3.4, 3.0 and 2.5 months, respectively. Perhaps the most important aspect of the study was the reported probability of 100% recovery to 20 million sperm per CC at 24 months (74). In another study exploring recovery of spermatogenesis after exogenous T use, Kolettis et al. started 22 men presenting with a history of infertility and exogenous T usage on medical recovery therapy utilizing CC or HCG and/or FSH based on the clinical judgment of the providers. Moreover, an additional 16 men were followed up after T cessation only. Patients’ age was 34 years on average with a median duration of T use of 24 months. Ultimately, 15 of 22 men given medical treatment and 16 of 17 men given no treatment other than T cessation had sperm return to the semen. Furthermore, final sperm concentration did not differ between groups. Interestingly, 21% of men in this study did not recover spermatogenesis after cessation or rescue treatment likely due to underlying spermatogenic failure rather than a permanent deleterious effect induced by exogenous T use (71). Wenker et al. reported results of therapy with HCG in 49 men with a history of exogenous testosterone and subsequent severe aberrations in sperm production. These individuals were placed on combination therapy, which included 3,000 units of subcutaneous HCG administered every other day supplemented with CC, tamoxifen, anastrozole or recombinant FSH. After therapy, follow-up semen analyses identified return of spermatogenesis and improved counts for azoospermic men and for men with severe oligospermia, respectively. On average, spermatogenesis was identified after 4.6 months of therapy with a mean first density of 22.6 million/mL (75). Kohn et al. recently published that increasing age and duration of exogenous testosterone use significantly reduced the likelihood of recovery of sperm in the ejaculate after rescue therapy with HCG and SERMs based on a criterion of a TMC of 5 million sperm, at 6 and 12 months (76). It is clear that patients presenting with infertility and concurrent T use should be counseled to immediately cease all use of T. Moreover, a thorough discussion regarding the likelihood of recovery and the risks and benefits of medical rescue therapy should be offered.
Enclomiphene citrate (Androxal, EC)
EC is a SERM that is similar to CC but differs in the absence of the cis isomer, zuclomiphene, found in CC (77). There has been interest in the use of EC in the treatment of hypogonadism and oligospermia due to its improved and pure estrogen antagonism compared to CC, which is found as a mixture of isomers with both antagonistic and agonistic mechanisms (78).
In a 2013 proof-of-principle study, Kaminetsky and colleagues evaluated the use of EC in the treatment of secondary hypogonadism in men previously treated with topical T and found that EC increased T and sperm counts with evidence of improved endogenous T production due to appropriate changes in LH and FSH levels (79). This proof-of-concept study was subsequently applied to a follow-up study of men with secondary hypogonadism in which the efficacy of treatment with enclomiphene versus 1% topical T gel was evaluated. In this investigation, all enrolled in the study were naïve to topical T. Overall, it was found that EC increased morning serum T, estradiol and LH similar to those obtained with topical T gel along with preservation of sperm counts. Specifically, regardless of 12.5 or 25 mg EC dosing, men maintained significantly greater total sperm counts (P=0.004 and P=0.012, respectively) compared to treatment with topical T (78).
Preliminary data involving EC shows promise but requires further investigation with randomized-controlled studies with the ultimately goal of securing FDA approval for the treatment of hypogonadism and/or male infertility.
Obesity and infertility
With the rapid rise in the obesity rate worldwide, the effect of obesity on male infertility has been a topic of interest. This increase in obesity has paralleled reports of rising rates of poor sperm quality and male infertility (80). Deriving direct associations between obesity and infertility is colluded by the several factors that are influenced by and may already be present within the obese patient presenting with concerns about fertility. Potential culprits that stymie an obese patient’s fertility potential include alterations in their hormonal profile such as decreased testosterone and sex hormone binding globulin (SHBG) and increased estrogen, body temperature, overall response to inflammation and oxidative stress. Moreover, various confounding co-morbidities that are often present in those with obesity such as insulin resistance and vascular disease may all contribute to limited fertility potential (81,82).
Evidence suggests that there is an increased prevalence of azoospermia and oligospermia in obese men (OR, 2.04; 95% CI, 1.59–2.62) (83). Moreover, obesity has been found to contribute to a reduction in sperm concentration by up to 21.6% as compared to men of normal weight (84,85). The association between obesity and motility and morphology are inconclusive; while some studies found body mass index (BMI) to negatively affect motility and morphology, others have found no difference (81,84-87). Obesity is associated with increased fragmentation of sperm DNA (87,88). In a 3-year multicenter study of 330 patients, Dupont and colleagues found increased DNA fragmentation in obese men compared to normal weight men, which persisted after adjusting for age and tobacco use (88).
It thus stands to reason that weight loss should subsequently improve such aberrations in sperm concentration and quality. No studies to date have reported an association between weight loss and improvement in birth rates in infertile couples with an obese male partner. Weight loss achieved by low-calorie diet and behavioral modifications, however, has been shown to improve both testosterone levels as well as SHBG (89,90).
Hormonal changes and sperm parameters have been studied in patients who have lost weight by undergoing bariatric surgery. Reis et al. assessed fertility in 20 morbidly-obese men over a 24-month period. It was found that those that underwent lifestyle modification followed by gastric bypass did not have significant changes in sperm quality at any time point over the course of 2 years though there was an improvement in sexual function as well as increased serum free testosterone, total testosterone, and FSH (91). El Bardisi et al. was able to demonstrate improvement in sperm concentration in those that were oligospermic or azoospermic prior to sleeve gastrectomy (P<0.05) along with significant increases in serum testosterone (P<0.001) (92). In a prospective double-armed study comparing semen parameters in men undergoing gastric bypass versus non-operative management, Samavat et al. demonstrated improvements in progressive/total sperm motility and number; however only semen volume and viability were found to have sustained significant improvements (P<0.05) after surgery (93).
As the prevalence of male obesity continues to rise, it is clear that there is a link between obesity, derangements of sexual hormones and semen parameters. However, the precise etiology is not well established and still requires considerable research. In their review, Meldrum et al. suggest that epigenetic studies may help us arrive to an enhanced understanding of the consequences of obesity on reproductive health (94). While associations between BMI and male infertility are currently being established, expanding our knowledge of the implications of obesity, as a disease, should prove to aid our ability in guiding these patients through the hopeful process of conceiving a child.
Hypogonadism and varicocelectomy
Despite the fact that over 35% of subfertile males have an identifiable varicocele (95), the notion that varicocelectomy may improve hypogonadism remains controversial with conflicting results regarding improvement of serum testosterone status-post surgery (96).
Hsiao et al. discovered that microsurgical varicocelectomy resulted in significant increases in serum testosterone levels regardless of the grade of the varicocele. In this retrospective study, 83% of men experienced a mean improvement in testosterone of 109.1±12.8 ng/dL after a mean follow-up of 7 months (97). These results corroborated the results of study by Zohdy et al. that found significant improvements in serum total testosterone levels (P<0.0001) after varicocelectomy. The mean improvement in serum testosterone in these patients was 71±35.6 ng/dL (98). In a meta-analysis of seven combined studies and 712 patients, Chen et al. discovered that males experienced a significant improvement (P<0.00001) in mean serum testosterone after undergoing a varicocelectomy. Interestingly, this improvement was significantly more pronounced in hypogonadal males compared to eugonadal or untreated males (P<0.00001). Whether these improvements in serum testosterone levels translate to improved symptoms in hypogonadal men is not well-established.
It does appear that varicocelectomy has desirable effects on semen parameters and testosterone levels; however, the indication of varicocele correction in the setting of hypogonadism is still not durably established without more randomized-control trials being done.
Growth hormone (GH)
In development, GH is important in the timing of puberty (99) and gonadal size (100). GH and its mediator insulin-like growth factor-1 (IGF-1) are thought to have gonadotropic effects, although the exact mechanisms are unclear. A series of studies of azoospermic men have shown that GH secretion in response to various stimuli such as arginine, clonidine, GHRH may be impaired in infertile men (101-103). Men with abnormal sperm parameters also have lower levels of serum IGF-1 compared with men with normal sperm parameters (104).
In animal studies, treatment with GH improves spermiogenesis. GH-deficient rats that are treated with GH show improvements in sperm concentration, morphology and motility (105). The spermatozoa of bulls treated with GH have improved motility after freezing and thawing and have higher rates of artificial insemination (106). However, the potential fertility benefits of GH in human subjects have not yet been demonstrated in large randomized trials.
A small observational study of ten men with idiopathic oligospermia (<10 million/mL) found that recombinant GH therapy may increase sperm concentration and total motile spermatozoa (107). Unfortunately, this result was not reproducible by Lee and colleagues who found no difference in sperm count in response to subcutaneous GH injections (108). Ovesen et al. treated nine asthenospermic and nine oligospermic males with GH for 12 weeks. Sperm motility was increased during the treatment period for both groups but there were no improvements in sperm count during treatment.
The small size and observational nature of these studies preclude our ability to make recommendations regarding the use of GH in treatment of male fertility. Thus far, it appears that GH may favorably affect sperm motility in patients with asthenospermia, but further investigation is needed.
Conclusions
Present literature regarding the endocrine management for male infertility lacks rigorous data to provide useful tools for the urologist’s armamentarium. That said, a few overarching themes exist. Modulations in sex hormone levels may improve semen parameters in the appropriately selected patient and agents such as SERMS, AIs and HCG are generally well tolerated. Correction of PRL, thyroid and GH levels may help in those that have abnormalities in semen parameters pertaining to those specific hormones. Obesity negatively affects fertility through multiple mechanisms and is an area of great potential for a growing number of patients. The desired outcome of pregnancy for the infertile couple is difficult to measure as a direct outcome of endocrinologic intervention. However, this must be attempted in multicenter controlled-randomized trials in order to appropriately characterize the true potential of our interventions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chehab M, Madala A, Trussell JC. On-label and off-label drugs used in the treatment of male infertility. Fertil Steril 2015;103:595-604. [Crossref] [PubMed]
- Ring JD, Lwin AA, Köhler TS. Current medical management of endocrine-related male infertility. Asian J Androl 2016;18:357-63. [Crossref] [PubMed]
- Cocuzza M, Agarwal A. Nonsurgical treatment of male infertility: specific and empiric therapy. Biologics 2007;1:259-69. [PubMed]
- Ko EY, Siddiqi K, Brannigan RE, et al. Empirical medical therapy for idiopathic male infertility: a survey of the American Urological Association. J Urol 2012;187:973-8. [Crossref] [PubMed]
- Shiraishi K, Ohmi C, Shimabukuro T, et al. Human chorionic gonadotrophin treatment prior to microdissection testicular sperm extraction in non-obstructive azoospermia. Hum Reprod 2012;27:331-9. [Crossref] [PubMed]
- Ramasamy R, Ricci JA, Palermo GD, et al. Successful fertility treatment for Klinefelter's syndrome. J Urol 2009;182:1108-13. [Crossref] [PubMed]
- Shoshany O, Abhyankar N, Mufarreh N, et al. Outcomes of anastrozole in oligozoospermic hypoandrogenic subfertile men. Fertil Steril 2017;107:589-94. [Crossref] [PubMed]
- Gregoriou O, Bakas P, Grigoriadis C, et al. Changes in hormonal profile and seminal parameters with use of aromatase inhibitors in management of infertile men with low testosterone to estradiol ratios. Fertil Steril 2012;98:48-51. [Crossref] [PubMed]
- Kim ED, Crosnoe L, Bar-Chama N, et al. The treatment of hypogonadism in men of reproductive age. Fertil Steril 2013;99:718-24. [Crossref] [PubMed]
- Patel DP, Brant WO, Myers JB, et al. The safety and efficacy of clomiphene citrate in hypoandrogenic and subfertile men. Int J Impot Res 2015;27:221-4. [Crossref] [PubMed]
- Chua ME, Escusa KG, Luna S, et al. Revisiting oestrogen antagonists (clomiphene or tamoxifen) as medical empiric therapy for idiopathic male infertility: a meta-analysis. Andrology 2013;1:749-57. [Crossref] [PubMed]
- Masala A, Delitala G, Alagna S, et al. Effect of clomiphene citrate on plasma levels of immunoreactive luteinizing hormone-releasing hormone, gonadotropin, and testosterone in normal subjects and in patients with idiopathic oligospermia. Fertil Steril 1978;29:424-7. [Crossref] [PubMed]
- Ross LS, Kandel GL, Prinz LM, et al. Clomiphene treatment of the idiopathic hypofertile male: high-dose, alternate-day therapy. Fertil Steril 1980;33:618-23. [Crossref] [PubMed]
- Jones TM, Fang VS, Rosenfield RL, et al. Parameters of response to clompiphene citrate in oligospermic men. J Urol 1980;124:53-5. [Crossref] [PubMed]
- Mićić S, Dotlić R. Evaluation of sperm parameters in clinical trial with clomiphene citrate of oligospermic men. J Urol 1985;133:221-2. [Crossref] [PubMed]
- Matsumiya K, Kitamura M, Kishikawa H, et al. A prospective comparative trial of a gonadotropin-releasing hormone analogue with clomiphene citrate for the treatment of oligoasthenozoospermia. Int J Urol 1998;5:361-3. [Crossref] [PubMed]
- Vandekerckhove P, Lilford R, Vail A, et al. Clomiphene or tamoxifen for idiopathic oligo/asthenospermia. Cochrane Database Syst Rev 2000. [PubMed]
- Hussein A, Ozgok Y, Ross L, et al. Clomiphene administration for cases of nonobstructive azoospermia: a multicenter study. J Androl 2005;26:787-91; discussion 792-3. [Crossref] [PubMed]
- Hussein A, Ozgok Y, Ross L, et al. Optimization of spermatogenesis-regulating hormones in patients with non-obstructive azoospermia and its impact on sperm retrieval: a multicentre study. BJU Int 2013;111:E110-4. [Crossref] [PubMed]
- Allag IS, Alexander NJ. Clomiphene citrate therapy for male infertility. Urology 1979;14:500-3. [Crossref] [PubMed]
- Wheeler KM, Smith RP, Kumar RA, et al. A Comparison of Secondary Polycythemia in Hypogonadal Men Treated with Clomiphene Citrate versus Testosterone Replacement: A Multi-Institutional Study. J Urol 2017;197:1127-31. [Crossref] [PubMed]
- Chandrapal JC, Nielson S, Patel DP, et al. Characterising the safety of clomiphene citrate in male patients through prostate-specific antigen, haematocrit, and testosterone levels. BJU Int 2016;118:994-1000. [Crossref] [PubMed]
- Pasqualotto FF, Fonseca GP, Pasqualotto EB. Azoospermia after treatment with clomiphene citrate in patients with oligospermia. Fertil Steril 2008;90:2014.e11-2. [Crossref] [PubMed]
- Kulin HE, Reiter EO. Gonadotropin suppression by low dose estrogen in men: evidence for differential effects upon FSH and LH. J Clin Endocrinol Metab 1972;35:836-9. [Crossref] [PubMed]
- Dumasia K, Kumar A, Deshpande S, et al. Differential roles of estrogen receptors, ESR1 and ESR2, in adult rat spermatogenesis. Mol Cell Endocrinol 2016;428:89-100. [Crossref] [PubMed]
- Carreau S, Bouraima-Lelong H, Delalande C. Estrogen, a female hormone involved in spermatogenesis. Adv Med Sci 2012;57:31-6. [Crossref] [PubMed]
- Schlegel PN. Aromatase inhibitors for male infertility. Fertil Steril 2012;98:1359-62. [Crossref] [PubMed]
- Inkster S, Yue W, Brodie A. Human testicular aromatase: immunocytochemical and biochemical studies. J Clin Endocrinol Metab 1995;80:1941-7. [PubMed]
- Raven G, de Jong FH, Kaufman JM, et al. In men, peripheral estradiol levels directly reflect the action of estrogens at the hypothalamo-pituitary level to inhibit gonadotropin secretion. J Clin Endocrinol Metab 2006;91:3324-8. [Crossref] [PubMed]
- T'Sjoen GG, Giagulli VA, Delva H, et al. Comparative assessment in young and elderly men of the gonadotropin response to aromatase inhibition. J Clin Endocrinol Metab 2005;90:5717-22. [Crossref] [PubMed]
- de Ronde W, de Jong FH. Aromatase inhibitors in men: effects and therapeutic options. Reprod Biol Endocrinol 2011;9:93. [Crossref] [PubMed]
- Pavlovich CP, King P, Goldstein M, et al. Evidence of a treatable endocrinopathy in infertile men. J Urol 2001;165:837-41. [Crossref] [PubMed]
- Clark RV, Sherins RJ. Treatment of men with idiopathic oligozoospermic infertility using the aromatase inhibitor, testolactone. Results of a double-blinded, randomized, placebo-controlled trial with crossover. J Androl 1989;10:240-7. [Crossref] [PubMed]
- Raman JD, Schlegel PN. Aromatase inhibitors for male infertility. J Urol 2002;167:624-9. [Crossref] [PubMed]
- Saylam B, Efesoy O, Cayan S. The effect of aromatase inhibitor letrozole on body mass index, serum hormones, and sperm parameters in infertile men. Fertil Steril 2011;95:809-11. [Crossref] [PubMed]
- Patry G, Jarvi K, Grober ED, et al. Use of the aromatase inhibitor letrozole to treat male infertility. Fertil Steril 2009;92:829.e1-2. [Crossref] [PubMed]
- Cavallini G, Beretta G, Biagiotti G. Preliminary study of letrozole use for improving spermatogenesis in non-obstructive azoospermia patients with normal serum FSH. Asian J Androl 2011;13:895-7. [Crossref] [PubMed]
- Helo S, Ellen J, Mechlin C, et al. A Randomized Prospective Double-Blind Comparison Trial of Clomiphene Citrate and Anastrozole in Raising Testosterone in Hypogonadal Infertile Men. J Sex Med 2015;12:1761-9. [Crossref] [PubMed]
- Kacker R, Conners W, Zade J, et al. Bone mineral density and response to treatment in men younger than 50 years with testosterone deficiency and sexual dysfunction or infertility. J Urol 2014;191:1072-6. [Crossref] [PubMed]
- Ramasamy R, Armstrong JM, Lipshultz LI. Preserving fertility in the hypogonadal patient: an update. Asian J Androl 2015;17:197-200. [Crossref] [PubMed]
- Farhat R, Al-zidjali F, Alzahrani AS. Outcome of gonadotropin therapy for male infertility due to hypogonadotrophic hypogonadism. Pituitary 2010;13:105-10. [Crossref] [PubMed]
- Yang L, Zhang SX, Dong Q, et al. Application of hormonal treatment in hypogonadotropic hypogonadism: more than ten years experience. Int Urol Nephrol 2012;44:393-9. [Crossref] [PubMed]
- Miyagawa Y, Tsujimura A, Matsumiya K, et al. Outcome of gonadotropin therapy for male hypogonadotropic hypogonadism at university affiliated male infertility centers: a 30-year retrospective study. J Urol 2005;173:2072-5. [Crossref] [PubMed]
- Check JH. Treatment of male infertility. Clin Exp Obstet Gynecol 2007;34:201-6. [PubMed]
- Bolyakov A, Paduch DA. Prolactin in men's health and disease. Curr Opin Urol 2011;21:527-34. [Crossref] [PubMed]
- Ben-Jonathan N, Mershon JL, Allen DL, et al. Extrapituitary prolactin: distribution, regulation, functions, and clinical aspects. Endocr Rev 1996;17:639-69. [PubMed]
- Rastrelli G, Corona G, Maggi M. The role of prolactin in andrology: what is new? Rev Endocr Metab Disord 2015;16:233-48. [Crossref] [PubMed]
- Binart N, Melaine N, Pineau C, et al. Male reproductive function is not affected in prolactin receptor-deficient mice. Endocrinology 2003;144:3779-82. [Crossref] [PubMed]
- Micic S, Dotlic R, Ilić V, et al. Hormone profile in hyperprolactinemic infertile men. Arch Androl 1985;15:123-8. [Crossref] [PubMed]
- Sueldo CE, Berger T, Kletzky O, et al. Seminal prolactin concentration and sperm reproductive capacity. Fertil Steril 1985;43:632-5. [Crossref] [PubMed]
- Nair S, Milsom S. Anejaculation as the presenting feature of pituitary microadenoma. Fertil Steril 2008;90:2012.e21-3. [Crossref] [PubMed]
- Krüger TH, Haake P, Haverkamp J, et al. Effects of acute prolactin manipulation on sexual drive and function in males. J Endocrinol 2003;179:357-65. [Crossref] [PubMed]
- Corona G, Wu FC, Rastrelli G, et al. Low prolactin is associated with sexual dysfunction and psychological or metabolic disturbances in middle-aged and elderly men: the European Male Aging Study (EMAS). J Sex Med 2014;11:240-53. [Crossref] [PubMed]
- Nishimura K, Matsumiya K, Tsuboniwa N, et al. Bromocriptine for infertile males with mild hyperprolactinemia: hormonal and spermatogenic effects. Arch Androl 1999;43:207-13. [Crossref] [PubMed]
- Mancini A, Guitelman A, Levalle O, et al. Bromocriptine in the management of infertile men after surgery of prolactin secreting adenomas. J Androl 1984;5:294-6. [Crossref] [PubMed]
- Okada H, Iwamoto T, Fujioka H, et al. Hyperprolactinaemia among infertile patients and its effect on sperm functions. Andrologia 1996;28:197-202. [Crossref] [PubMed]
- Ufearo CS, Orisakwe OE. Restoration of normal sperm characteristics in hypoprolactinemic infertile men treated with metoclopramide and exogenous human prolactin. Clin Pharmacol Ther 1995;58:354-9. [Crossref] [PubMed]
- Lotti F, Corona G, Maseroli E, et al. Clinical implications of measuring prolactin levels in males of infertile couples. Andrology 2013;1:764-71. [Crossref] [PubMed]
- Mintziori G, Kita M, Duntas L, et al. Consequences of hyperthyroidism in male and female fertility: pathophysiology and current management. J Endocrinol Invest 2016;39:849-53. [Crossref] [PubMed]
- Krassas GE, Pontikides N. Male reproductive function in relation with thyroid alterations. Best Pract Res Clin Endocrinol Metab 2004;18:183-95. [Crossref] [PubMed]
- Kumar A, Shekhar S, Dhole B. Thyroid and male reproduction. Indian J Endocrinol Metab 2014;18:23-31. [Crossref] [PubMed]
- Abalovich M, Levalle O, Hermes R, et al. Hypothalamic-pituitary-testicular axis and seminal parameters in hyperthyroid males. Thyroid 1999;9:857-63. [Crossref] [PubMed]
- Krassas GE, Pontikides N, Deligianni V, et al. A prospective controlled study of the impact of hyperthyroidism on reproductive function in males. J Clin Endocrinol Metab 2002;87:3667-71. [Crossref] [PubMed]
- Griboff SI. Semen analysis in myxedema. Fertil Steril 1962;13:436-43. [Crossref] [PubMed]
- Madhukar D, Rajender S. Hormonal treatment of male infertility: promises and pitfalls. J Androl 2009;30:95-112. [Crossref] [PubMed]
- Nikoobakht MR, Aloosh M, Nikoobakht N, et al. The role of hypothyroidism in male infertility and erectile dysfunction. Urol J 2012;9:405-9. [PubMed]
- Patel DP, Chandrapal JC, Hotaling JM. Hormone-Based Treatments in Subfertile Males. Curr Urol Rep 2016;17:56. [Crossref] [PubMed]
- Poppe K, Glinoer D, Tournaye H, et al. Is systematic screening for thyroid disorders indicated in subfertile men? Eur J Endocrinol 2006;154:363-6. [Crossref] [PubMed]
- Lotti F, Maseroli E, Fralassi N, et al. Is thyroid hormones evaluation of clinical value in the work-up of males of infertile couples? Hum Reprod 2016;31:518-29. [Crossref] [PubMed]
- Crosnoe LE, Grober E, Ohl D, et al. Exogenous testosterone: a preventable cause of male infertility. Transl Androl Urol 2013;2:106-13. [PubMed]
- Kolettis PN, Purcell ML, Parker W, et al. Medical testosterone: an iatrogenic cause of male infertility and a growing problem. Urology 2015;85:1068-72. [Crossref] [PubMed]
- Kinniburgh D, Zhu H, Cheng L, et al. Oral desogestrel with testosterone pellets induces consistent suppression of spermatogenesis to azoospermia in both Caucasian and Chinese men. Hum Reprod 2002;17:1490-501. [Crossref] [PubMed]
- Anderson RA, Kelly RW, Wu FC. Comparison between testosterone enanthate-induced azoospermia and oligozoospermia in a male contraceptive study. V. Localization of higher 5 alpha-reductase activity to the reproductive tract in oligozoospermic men administered supraphysiological doses of testosterone. J Androl 1997;18:366-71. [PubMed]
- Liu PY, Swerdloff RS, Christenson PD, et al. Rate, extent, and modifiers of spermatogenic recovery after hormonal male contraception: an integrated analysis. Lancet 2006;367:1412-20. [Crossref] [PubMed]
- Wenker EP, Dupree JM, Langille GM, et al. The Use of HCG-Based Combination Therapy for Recovery of Spermatogenesis after Testosterone Use. J Sex Med 2015;12:1334-7. [Crossref] [PubMed]
- Kohn TP, Louis MR, Pickett SM, et al. Age and duration of testosterone therapy predict time to return of sperm count after human chorionic gonadotropin therapy. Fertil Steril 2017;107:351-7.e1. [Crossref] [PubMed]
- Rodriguez KM, Pastuszak AW, Lipshultz LI. Enclomiphene citrate for the treatment of secondary male hypogonadism. Expert Opin Pharmacother 2016;17:1561-7. [Crossref] [PubMed]
- Wiehle RD, Fontenot GK, Wike J, et al. Enclomiphene citrate stimulates testosterone production while preventing oligospermia: a randomized phase II clinical trial comparing topical testosterone. Fertil Steril 2014;102:720-7. [Crossref] [PubMed]
- Kaminetsky J, Werner M, Fontenot G, et al. Oral enclomiphene citrate stimulates the endogenous production of testosterone and sperm counts in men with low testosterone: comparison with testosterone gel. J Sex Med 2013;10:1628-35. [Crossref] [PubMed]
- Raad G, Hazzouri M, Bottini S, et al. Paternal obesity: how bad is it for sperm quality and progeny health? Basic Clin Androl 2017;27:20. [Crossref] [PubMed]
- Hammoud AO, Gibson M, Peterson CM, et al. Impact of male obesity on infertility: a critical review of the current literature. Fertil Steril 2008;90:897-904. [Crossref] [PubMed]
- Kahn BE, Brannigan RE. Obesity and male infertility. Curr Opin Urol 2017;27:441-5. [Crossref] [PubMed]
- Sermondade N, Faure C, Fezeu L, et al. BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum Reprod Update 2013;19:221-31. [Crossref] [PubMed]
- Jensen TK, Andersson AM, Jorgensen N, et al. Body mass index in relation to semen quality and reproductive hormones among 1,558 Danish men. Fertil Steril 2004;82:863-70. [Crossref] [PubMed]
- Cui X, Jing X, Wu X, et al. Protective effect of resveratrol on spermatozoa function in male infertility induced by excess weight and obesity. Mol Med Rep 2016;14:4659-65. [Crossref] [PubMed]
- Magnusdottir EV, Thorsteinsson T, Thorsteinsdottir S, et al. Persistent organochlorines, sedentary occupation, obesity and human male subfertility. Hum Reprod 2005;20:208-15. [Crossref] [PubMed]
- Kort HI, Massey JB, Elsner CW, et al. Impact of body mass index values on sperm quantity and quality. J Androl 2006;27:450-2. [Crossref] [PubMed]
- Dupont C, Faure C, Sermondade N, et al. Obesity leads to higher risk of sperm DNA damage in infertile patients. Asian J Androl 2013;15:622-5. [Crossref] [PubMed]
- Kaukua J, Pekkarinen T, Sane T, et al. Sex hormones and sexual function in obese men losing weight. Obes Res 2003;11:689-94. [Crossref] [PubMed]
- Niskanen L, Laaksonen DE, Punnonen K, et al. Changes in sex hormone-binding globulin and testosterone during weight loss and weight maintenance in abdominally obese men with the metabolic syndrome. Diabetes Obes Metab 2004;6:208-15. [Crossref] [PubMed]
- Reis LO, Zani EL, Saad RD, et al. Bariatric surgery does not interfere with sperm quality--a preliminary long-term study. Reprod Sci 2012;19:1057-62. [Crossref] [PubMed]
- El Bardisi H, Majzoub A, Arafa M, et al. Effect of bariatric surgery on semen parameters and sex hormone concentrations: a prospective study. Reprod Biomed Online 2016;33:606-11. [Crossref] [PubMed]
- Samavat J, Cantini G, Lotti F, et al. Massive Weight Loss Obtained by Bariatric Surgery Affects Semen Quality in Morbid Male Obesity: a Preliminary Prospective Double-Armed Study. Obes Surg 2018;28:69-76. [Crossref] [PubMed]
- Meldrum DR, Morris MA, Gambone JC. Obesity pandemic: causes, consequences, and solutions-but do we have the will? Fertil Steril 2017;107:833-9. [Crossref] [PubMed]
- Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril 1993;59:613-6. [Crossref] [PubMed]
- Chen X, Yang D, Lin G, et al. Efficacy of varicocelectomy in the treatment of hypogonadism in subfertile males with clinical varicocele: A meta-analysis. Andrologia 2017.49. [PubMed]
- Hsiao W, Rosoff JS, Pale JR, et al. Varicocelectomy is associated with increases in serum testosterone independent of clinical grade. Urology 2013;81:1213-7. [Crossref] [PubMed]
- Zohdy W, Ghazi S, Arafa M. Impact of varicocelectomy on gonadal and erectile functions in men with hypogonadism and infertility. J Sex Med 2011;8:885-93. [Crossref] [PubMed]
- Tatò L, Zamboni G, Antoniazzi F, et al. Gonadal function and response to growth hormone (GH) in boys with isolated GH deficiency and to GH and gonadotropins in boys with multiple pituitary hormone deficiencies. Fertil Steril 1996;65:830-4. [Crossref] [PubMed]
- Carani C, Granata AR, De Rosa M, et al. The effect of chronic treatment with GH on gonadal function in men with isolated GH deficiency. Eur J Endocrinol 1999;140:224-30. [Crossref] [PubMed]
- Ovesen P, Jorgensen JO, Ingerslev J, et al. Growth hormone treatment of subfertile males. Fertil Steril 1996;66:292-8. [Crossref] [PubMed]
- Shimonovitz S, Zacut D, Ben Chetrit A, et al. Growth hormone status in patients with maturation arrest of spermatogenesis. Hum Reprod 1993;8:919-21. [Crossref] [PubMed]
- Fujisawa M, Yamanaka K, Okada H, et al. Growth hormone releasing hormone test for infertile men with spermatogenetic maturation arrest. J Urol 2002;168:2083-5. [Crossref] [PubMed]
- Lee HS, Park YS, Lee JS, et al. Serum and seminal plasma insulin-like growth factor-1 in male infertility. Clin Exp Reprod Med 2016;43:97-101. [Crossref] [PubMed]
- Gravance CG, Breier BH, Vickers MH, et al. Impaired sperm characteristics in postpubertal growth-hormone-deficient dwarf (dw/dw) rats. Anim Reprod Sci 1997;49:71-6. [Crossref] [PubMed]
- Sauerwein H, Breier BH, Gallaher BW, et al. Growth hormone treatment of breeding bulls used for artificial insemination improves fertilization rates. Domest Anim Endocrinol 2000;18:145-58. [Crossref] [PubMed]
- Radicioni A, Paris E, Dondero F, et al. Recombinant-growth hormone (rec-hGH) therapy in infertile men with idiopathic oligozoospermia. Acta Eur Fertil 1994;25:311-7. [PubMed]
- Lee KO, Ng SC, Lee PS, et al. Effect of growth hormone therapy in men with severe idiopathic oligozoospermia. Eur J Endocrinol 1995;132:159-62. [Crossref] [PubMed]


