The infrapubic surgical approach for inflatable penile prosthesis placement
Introduction
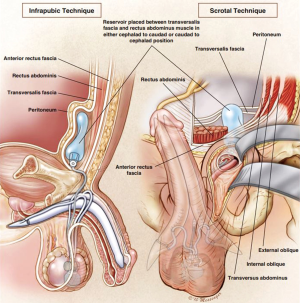
Since the first description of the use of an internalized inflatable penile prosthesis by Scott et al. in 1973 (1), the devices and associated surgical approaches have evolved to make the operation easier, safer and more effective. Several surgical approaches for penile prosthetics have been described, including a dorsal subcoronal, dorsal penile shaft, ventral penile shaft, penoscrotal, perineal, infrapubic and suprapubic (2). However, the infrapubic and the penoscrotal surgical incisions have stood the test of time and are commonly used for implantation of inflatable penile prosthetics. The 2015 International Consultation of Sexual Medicine (ICSM) states “penoscrotal, infra-pubic, and subcoronal are the three main approaches for inserting a penile prosthesis” (3). The surgical technique and penile prosthesis type chosen depends upon surgeon preference and may be directed by familiarity, the patient’s specific anatomy or prior surgical history.
The infrapubic surgical approach was detailed by Barrett and Furlow in 1985 (4). Since then, several revisions of this technique have subsequently been described in the literature, including using a penoscrotal counter-incision for pump placement (5) and a smaller infrapubic incision to make for a more minimally invasive surgical procedure (6). Two of the obvious advantages to the infrapubic approach are the ability to implant the reservoir more rapidly and under direct vision through the same incision and the avoidance of an extra incision on the scrotum, removing one obstacle to rehabilitation (3,7). The disadvantages that have been cited include potential damage to the dorsal nerves of the penis with resultant sensory loss (albeit never documented in the literature), limited distal corporal exposure and the lack of access to the most dependent part of the scrotum for pump fixation (7,8). These disadvantages are overcome with careful dissection, the use of hydrodilatation, and the use of the nasal speculum for pump placement.
In one of the earliest studies to analyze patient satisfaction and post-operative complications for three-piece inflatable prostheses, Candela et al. showed no statistically significant difference between the penoscrotal and the infrapubic approach, including incisional discomfort, scrotal pain/edema, scrotal hematoma, incidence of penile paresthesia, or post-operative infection rate (9). Further updates to the literature may show that this continues to hold true today.
Patient selection
We believe that any patient is a candidate for an infrapubic approach to a penile implant. For example, revisions are often best served through the infrapubic approach in order to at least attempt reservoir retrieval without the need for a secondary incision. Reservoir placement through an infrapubic incision, as described below, allows the procedure to proceed without a Foley catheter, something many patients find appealing. Anecdotally, we can confirm that patients also prefer a 1–2 cm incision outside the actual penis and scrotum. However, the obese patient provides the unique challenge of finding an adequately flat surface to negotiate the longest instrument utilized in the infrapubic approach to a penile implant: the Furlow passer. Careful positioning, as described below, should alleviate this difficulty for even the most inexperienced of implanters during the infrapubic case.
Operative technique
The patient must be positioned on the table in the dorsal recumbent position with the table hyper-extended creating a flat surface at the mons pubis.
The groin hair is removed by shaving with a razor, as opposed to a clipper. The patient has been told to void prior to entering the operating room. Those that do not void are straight-cathed prior to the prep. The groin is then prepped with a Hibiclens® hand preparation followed by two ChloraPrep™ sticks from the umbilicus to the mid-thigh.
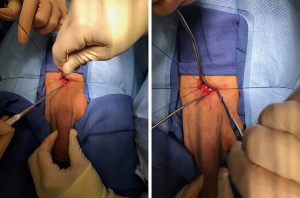
Prior to incision, patients are administered a pudendal nerve block with 10 cc of ropivacaine by scything lateral to the corpora and injecting at Alcock’s canal. We begin the procedure with an artificial erection using a total of 60 cc of normal saline or a combination of normal saline plus lidocaine if performing the implant under pure local anesthesia. The first 30 cc are injected while placing pressure directly to the base of the penis in order to identify potential pathology that may have not been evident on physical exam of the flaccid penis. The remaining 30 cc is then injected to accomplish the complete hydrodilatation of the corpora supplanting serial dilation in the penis with no pathology. This hydrodilatation also allows for identification of the dorsal nerve and easy lateral placement of the stay sutures (Figure 1).
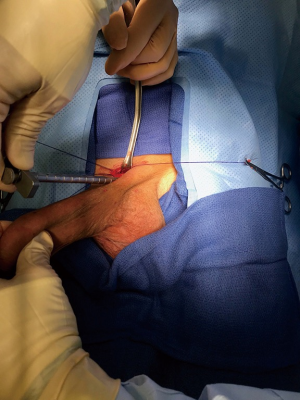
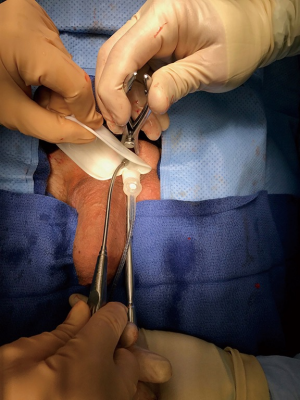
The infrapubic incision is made one fingerbreadths above the penile pubic junction while gently pulling down on the penis. This incision is extended only as wide as the pump (Figure 2). We create a small defect in Scarpa’s fascia and sweep down along either side of the penis to the level of the corpora bilaterally, sparing as many superficial vessels as possible to avoid post-operative penile edema.
We utilize a bent appendiceal retractor to expose the corpora, gently pushing down as opposed to pulling, allowing for greater exposure. We then use a 2-0 MonocrylTM suture on a UR6 needle to reach down and catch tunica with a sturdy needle, especially in patients that may require deeper dissections down to the corpora. A total of four bites are made (a single set of stays bilaterally). A pediatric Yankour is utilized to roll the corpora and thus the neurovascular bundle out of the way before placing a single set of stay sutures bilaterally. This is all made very simple after the hydrodilatation of the penis, providing more corporal topography with which to work. It is important to not take too large of a bite with the stay suture, otherwise when closing, the tunica will bunch up unnecessarily, similar to a Nesbit plication. Our stay sutures are eventually used as our closing sutures (Figure 3).
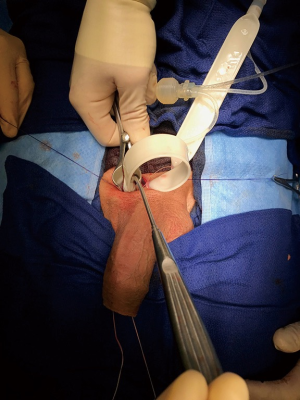
Next, we make the bilateral corporotomies with a #12 blade. The corporotomies are limited to the widest part of the cylinder at the tubing exit site or 1.5 cm (Figure 4). Measurements with the Furlow introducer must be performed along the long axis of the penis with counter traction to avoid proximal perforation (Figure 5). Note that no dilation is necessary in the non-pathologic penis, a state usually known after the hydrodilatation of the penis. Similar measurement along the long axis of the penis is performed distally, pulling down on the penis while scything laterally with the Furlow introducer. One must firmly squeeze the glans in an anterior-posterior fashion to protect the fossa from perforation where the tunica comes down to only one layer. We use a 4×4 gauze to gain control of the glans while performing this maneuver, which allows manipulation of the Furlow introducer through any fibrotic tissue with impunity (Figure 6). Bouncing the Furlow keeps one from gaining too much velocity and potentially damaging the tunica. Serial dilation is not performed if there is no pathology in the penis. A Hegar #12 dilator may be used to calibrate, but not to dilate. We prefer the Hegar dilator to the Brooks dilators because the reticulating arm on the Brooks dilator can be difficult for some surgeons to maintain adequate control.
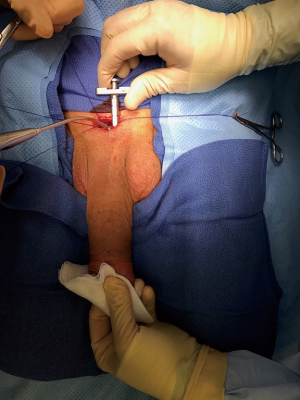
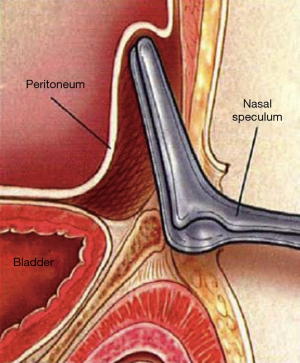
We always use a 125 cc reservoir because we prefer to underfill the reservoir in order to avoid excessive intrinsic pressures. Reservoir placement in the non-compromised pelvis is accomplished by first blunting dissecting the fat off the pubic rami until the external inguinal ring is identified. A 70 mm nasal speculum is then inserted into the external inguinal ring and the transversalis fascia is perforated. The blades are then immediately turned and driven cephalad (Figure 7). When the blades are open one can feel fascia anteriorly and empty space posteriorly. We call this location posterior to transversalis fascia (Figure 8). In patients with compromised pelves, the nasal speculum is advanced less distance into the ring and thrust upward into the space anterior to transversalis fascia (Figure 9). A pediatric Yankauer suction tip is then used to deploy the 125 cc reservoir cephalad (Figure 10).
With our reservoir filled and our implant not yet delivered to the field, we drape off everything but the incision with antibiotic impregnated towels. We use the Keith needle for cylinder insertion. When deploying the Keith needle, one must always remember to again work along the long axis of the penis, which requires traction of the penis to keep the axis straight. Where the Keith needle comes out on the glans is not of much consequence as long as it comes out on the ipsilateral side because the implant will find the correct position.
In order to place the cylinder proximally, we like to pull the cylinder distally with the lead string maintaining tension on the string while holding the cylinder like a pen, draping the cylinder over the thumb. This allows the cylinder to act as a retractor, allowing a straight shot to drop the cylinder proximally. We make certain to fill any redundant cylinder into the corpora like an accordion. Some trainees prefer to drop the cylinder in proximally using a nasal speculum, first pushing down with your finger or the Yankauer suction tip and then pulling distally (Figure 11).
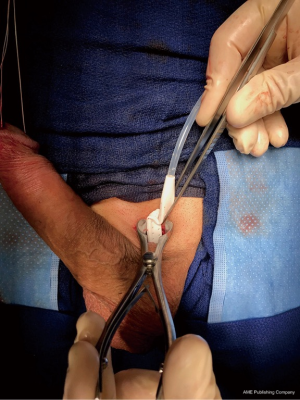
A rapid fill is then performed with a 60 cc syringe as a surrogate reservoir to evaluate the functional and cosmetic result. One may have to manipulate the penis back and forth to assist in correct cylinder seating. The coporotomies are closed using the pre-placed stay sutures. The sutures are usually tied distal to the tubing exit site.
Pump placement is always midline, posterior and dependent. The pump is brought down along the same side as the reservoir using the nasal speculum to pop through Colles’ fascia deep into the most dependent portion of the scrotum. The blades of the nasal speculum point to where the pump will reside (Figure 12). The assistant takes the pump in an anterior-posterior fashion and gently pulls down until the dartos fascia is felt to release, resulting in perfect pump placement (Figure 13). Proper pump position is confirmed by pulling up on the penis (Figure 14). If the pump remains in the dependent position, the patient and patient’s partner should be satisfied. The pump is then pulled up to the mid scrotum for easy tubing connection between the reservoir and the pump. When the pump is returned to the dependent portion of the scrotum no residual tubing remains at the incision site.


Finally, a #10 Jackson-Pratt surgical drain is placed along the entire length of the surgical field adjacent to the implant (Figure 15). The end of the drain is brought out through a separate stab wound superior to the incision. Scarpa’s fascia is closed with a running suture. Staples are used to close the skin, as the staples tend to deter patients from touching their surgical wounds. A TegadermTM is used to dress the wound. Compressive dressings are not utilized. A 10-pound sand bag is placed on the incision for 2 h in the recovery room. Once the sand bag is removed, the drain output is monitored over the next hour. If a brisk amount of drainage is documented (>60 cc), the sand bag is reapplied (Figure 16).
Post-operative care
All our patients have drains post-operatively which are removed sometime between 1 and 3 days out. Patients, and their surgeons, should expect somewhere around 100 cc of drainage within the first 24 h. If the drainage has dropped off over the previous 4 h, the drains are usually ready to be removed post-operative day #1. The patient is then immediately instructed to pull down on his pump and attempt to find the deflate mechanism every time he voids. Patients must not submerse in water until the wound is completely sealed. Patients are discharged home on NSAIDs. Any pain warranting narcotics should be further investigated. No outpatient antibiotics are prescribed. Implants are cycled as soon as the patient can tolerate the process and patients are encouraged to engage in sexually activity sometime after 3 weeks.
Post-operative complications
Immediate post-operative urinary retention is seen approximately 4% of our patients undergoing penile implants using the infrapubic approach. As with for our penoscrotal counterparts, our most frequent postoperative complaint is scrotal pain. However, in the case of the infrapubic approach this is almost exclusively related to tubing running down the affected side and resolves around post-operative day #14. After more than 6,000 cases with more than 400 visiting urologists accompanying our team, we have yet to document one case of penile sensory loss.
Distal urethral injuries were not uncommon in our early years because we did not focus on protecting the fossa during measurement with the Furlow. Currently, we are not satisfied unless the fossa is protected by squeezing the glans with a 4×4 gauze pad for increased stability. This portion of the procedure was further improved upon by gently bouncing the Furlow down the penis during measurement, never allowing the device enough velocity to overcome your protections. Our bowel, bladder and vascular injury record for reservoir placement has stood test of time using the aforementioned techniques (10). However, recently Gross et al. demonstrated that patients with low BMIs should be more cautiously monitored for inadvertent intraperitoneal placement of the reservoir using ATF or PTF placement of the reservoir (11). Finally, our infection rates are routinely less than 1% yearly.
Lessons learned
Pre-operatively, the patient may be concerned about incision location, use of a catheter, type of anesthetic, degree of pain and penis size. Postoperatively, the patient is concerned about incisional discomfort, scrotal pain/edema, scrotal hematoma, incidence of penile paresthesia, infection, time to resume sexual activity and again penile implant size. As one decides on the approach to placing a penile implant, he/she must consider all the aforementioned concerns and issues. We believe that our minimally invasive infrapubic approach as described provides the patient with a more direct path to resuming normal sexual activity by limiting the obstacles to rehabilitation: scrotal incision, scrotal fluid collection, etc.
Nearly all lessons a penile prosthetic specialist would encounter could be related to improper patient expectations, regardless of the approach. All prosthetic surgeons should be well versed in discussing penile size, both before and after the procedure. All prosthetic surgeons should understand the existence of glanular hypermobility and have an established algorithm for treating the patient suffering from this often expected anatomical finding. Finally, we are not trained psychiatrists, although at times many of you must act as if you are dabbling in the trade. Proper comfort with your approach will aid the implanter and patient in recognizing that your finest work was performed in placing the prosthesis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Scott FB, Bradley WE, Timm GW. Management of erectile impotence. Use of implantable inflatable prosthesis. Urology 1973;2:80-2. [Crossref] [PubMed]
- Montague DK. Penile prostheses. In: Montague DK. editor. Disorders of Male Sexual Function. Chicago: Year Book Medical Publishers, 1988:154-91.
- Levine LA, Becher E, Bella A, et al. Penile Prosthesis Surgery: Current Recommendations From the International Consultation on Sexual Medicine. J Sex Med 2016;13:489-518. [Crossref] [PubMed]
- Barrett DM, Furlow WL. Penile prosthesis implantation. In: Segraves RT, Schoenberg HW. editors. Diagnosis and Treatment of Erectile Disturbances: A Guide for Clinicians. New York: Plenum Medical Book Co., 1985:219-40.
- Graydon RJ, Berlin BB. Improved pump placement with infrapubic penile prosthetic implantation. J Urol 1992;148:102-3. [Crossref] [PubMed]
- Perito PE. Minimally invasive infrapubic inflatable penile implant. J Sex Med 2008;5:27-30. [Crossref] [PubMed]
- Montague DK, Angermeir KW. Surgical approaches for penile prosthesis implantation: penoscrotal vs infrapubic. Int J Impot Res 2003;15 Suppl 5:S134-5. [Crossref] [PubMed]
- Kramer A, Chason J. Residents at the University of Maryland Medical System provide insight to learning infrapubic approach for IPP surgery: relative benefits but novel challenges exposed in first 15 cases. J Sex Med 2010;7:1298-305. [Crossref] [PubMed]
- Candela JV, Hellstrom WJ. Three-piece inflatable penile prosthesis implantation: a comparison of the penoscrotal and infrapubic surgical approaches. J La State Med Soc 1996;148:296-301. [PubMed]
- Stember DS, Garber BB, Perito PE. Outcomes of abdominal wall reservoir placement in inflatable penile prosthesis implantation: a safe and efficacious alternative to the space of Retzius. J Sex Med 2014;11:605-12. [Crossref] [PubMed]
- Gross MS, Stember DS, Garber BB, et al. A retrospective analysis of risk factors for IPP reservoir entry into the peritoneum after abdominal wall placement. Int J Impot Res 2017. [Epub ahead of print]. [Crossref] [PubMed]