Surgical patient selection and counseling
Introduction
On January 28, 2013, an Orange County Urologist and developer of a topical spray for premature ejaculation was killed by a distraught patient as he entered the exam room (1). Although the details remain unclear, the suspect—a former VA patient who had been treated nearly 20 years earlier for a prostate condition—had described significant psychological distress relating to stress incontinence from the earlier surgery. The suspect currently remains in prison awaiting trial and has settled a civil case for >$2 million over the surgeon’s wrongful death (2).
Although tragic in nature, this provides one extreme example (of several) of the potential consequences resulting from patient dissatisfaction and surgical complications. Additionally, it underscores a need for appropriate patient selection and counseling with any surgical procedure, particularly when quality of life and satisfaction are the primary objectives of treatment. Despite the unavoidable nature of complications in general, the ability to discriminate appropriate surgical candidates remains completely within the control of the surgeon.
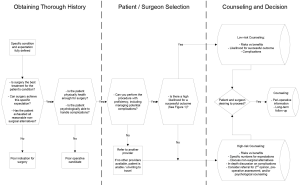
Given the critical importance of patient selection and counseling, the current manuscript is written to provide andrological surgeons with potential tools to identify appropriate surgical candidates. The article begins with a discussion on what defines a successful outcome and determinants of satisfaction and dissatisfaction with surgery, followed by an in-depth analysis of factors relating to patient selection, including organic and psychological patient factors and surgeon characteristics. Additionally, visual algorithms are provided to help demonstrate how these factors integrate into the final decision as to whether a patient is a viable candidate for surgery. And finally, aspects relating to appropriate patient counseling are reviewed.
It is notable that the current manuscript is intended to be a practical reference for andrological surgeons performing surgeries including, but not limited to penile prostheses (PP), Peyronie’s disease (PD) procedures, infertility surgeries, benign prostatic hyperplasia (BPH) and incontinence treatments, penile revascularization, panniculectomy, and other penoscrotal surgeries performed for aesthetic reasons. Since a limited volume of literature exists on this topic, when possible, references on patient satisfaction/dissatisfaction were obtained from the andrological and cosmetic surgery literature. In the absence of available studies, statements were made based on expert opinion or generally accepted clinical principles.
How is success defined?
There is currently no consensus as to what defines therapeutic success. In its simplest form, a successful surgery may be defined as the ability to complete an operation. Success may also be defined by patient satisfaction, lack of dissatisfaction, lack of complications, lack of recurrence, or by many other definitions. In this regard, several outcome measures have been utilized including the Global Assessment Questionnaire, International Index of Erectile Function, Erectile Dysfunction Inventory of Treatment Satisfaction, and Peyronie’s Disease Questionnaire, among many others (3,4). However, each of these definitions and questionnaires are inadequate and fail to describe the full breadth of what should define a successful outcome (5-7).
Arguably, a truly successful outcome is one that is patient-centered and focuses on achieving an optimal result based on the presenting condition and treatment expectations. This suggests a far more comprehensive definition for success and requires a thorough clinical evaluation to define patient desires and expectations, appropriate patient selection to identify organic and psychological barriers and capacities, pre-operative preparation, a wide breadth of surgical skills, volume, and experience, identification and management of complications, and extended patient follow-up.
To highlight the differences among definitions, a surgeon may report successful placement of a penile prosthesis in a patient. However, further investigation may identify that the patient had never tried therapies such as PDE5 inhibitors, or that he was actually seeking enhanced relationship satisfaction with his partner (without caring about penetrative intercourse), or that he was unable to actually utilize the device due to issues with the pump. As such, this patient would have been a surgical success and yet a treatment failure at the same time. Similarly, a patient undergoing a microTESE procedure may develop de-novo low testosterone and have no sperm retrieved, and yet be satisfied by the knowledge that they did all they could to achieve a biological child. In this case, the patient may be defined as a surgical failure but a treatment success.
Another aspect that is relevant to defining success is its temporal nature. A patient may be satisfied at one-time point and dissatisfied at another. Similarly, complications may occur pre-, intra-, or post-operatively, and diseases may change as a function of their natural history (PD). Similarly, comparing outcomes between surgical series is of limited reliability and value, as each surgeon evaluates distinct populations of patients and has unique inclusion/exclusion criteria for patient selection. As such, a surgeon with excellent outcomes may signify true surgical skill, or may simply indicate strict patient selection or less medically-complex patients, among other factors.
Success is further complicated by a lack of 3rd party verification of outcomes. Given the current climate of fee-for-service in many geographic locations, there is an inherent strong incentive to misrepresent success rates. It is interesting to note that in an industry where regulation is ever present and heavily enforced (i.e., exact method of faxing materials is outlined with severe punishments for errors), there remains a glaring absence of transparency on true surgical outcomes and success rates.
Therefore, the best definition for success is likely one that incorporates all of the above factors in a patient-centered manner. Surgeons wishing to achieve excellence in outcomes should thus focus on improving all aspects of patient care, from the initial history, to patient selection, operative outcomes, and long-term post-operative follow-up.
What are determinants of satisfaction and dissatisfaction?
Several factors have been consistently identified as relating to satisfaction and dissatisfaction with surgical procedures. In a study of 21 men undergoing PP surgery, an inverse correlation was noted between pre-operative expectations and post-operative satisfaction, with expectations accounting for approximately 24% of satisfaction overall (8). Operative complications are also directly associated with dissatisfaction, with some cosmetic literature suggesting an approximately 60% increase in dissatisfaction among patients experiencing a complication within 90 days of surgery (9). Similarly, an increasing number of revision surgeries for non-infectious or non-mechanical reasons is inversely correlated with satisfaction, a finding which is not surprising given that, by definition, these patients are dissatisfied with the initial procedure (10,11).
Surgery-specific factors have also been identified to predict either satisfaction directly or indirectly through avoiding undesirable side effects of therapy. For example, satisfaction with PP has been associated with favorable female partner sexual function, BMI ≤30, absence of PD or prostatectomy (12,13). With PD, an increased rate of ED (indirectly associated with decreased satisfaction) is noted among men >55, those with poor pre-op function or activity, curvatures >60 degrees, grafts >3 cm, ventral grafts, or use of specific techniques (14-16).
Similarly, surgical-specific factors relating to dissatisfaction have been reported. Although a complete listing of all andrological procedures is not practical, an example of factors relating to PP include reduced penile length, decreased glanular engorgement, changes in penile or ejaculatory sensation, pain, cosmetic appearance, inability to function the device, pre-operative therapies, and partner dissatisfaction, among others (8,17-26). A thorough understanding of factors associated with satisfaction and dissatisfaction is essential for surgeons wishing to optimize outcomes, as they provide a basic framework for identifying appropriate, and more importantly, inappropriate, surgical candidates.
Patient selection
Patient non-psychological factors
In addition to determinants of satisfaction, the successful surgeon must take into account patient-specific factors that may impact outcomes. These details are then weighed in the balance of risks versus benefits to determine if surgery represents a reasonable option. Arguably, surgeons are very good at this aspect of patient selection, and some would consider this to be the only criteria necessary in deciding who is or is not a candidate for surgery.
Factors that may influence results include the severity of the underlying condition, prior treatments to the operative site, or comorbid conditions and medications impacting healing. Similarly, several conditions may increase the likelihood for peri-operative complications including blood thinning medications (or the holding of the medications), comorbid diseases (in particular cardiac, pulmonary, vascular, or diabetes), living conditions, recreational smoking, drug, or alcohol use.
Although many of these conditions increase the possibility of complications, they should not automatically exclude a patient from undergoing surgery. Rather, they should factor into an analysis weighing the risks and benefits of surgery. As an example, a man with uncontrolled DM wishing to undergo placement of a PP may be excluded by a surgeon until he achieves a lower HbA1c level. This may be done due to concerns over an increased risk for device infection (although the impact of DM on infection rates remains debatable at the present time) (27-29). However, in many cases, patients may never be able to achieve normal HbA1c levels due to various reasons. Rather than exclude the patient from surgery lifelong, it may be more reasonable to counsel the patient that his rate of infection may be higher than compared to someone without DM or with controlled DM and then allow him to make the decision. As such, the astute surgeon recognizes that the risks and sequelae of ED with non-treatment are 100% compared to a potential small increased risk of infection.
Patient psychological factors
One of the most important aspects of patient selection is accurately identifying the patient’s goals, objectives, and expectations of treatment. Although some patients have previously decided on a treatment course prior to office evaluation, many are seeking the surgeon’s recommendations on which therapy would be most likely to address their underlying concern. Appropriate patient selection is therefore dependent on obtaining a thorough history and fully understanding which specific issue he is hoping to treat.
As an example, a patient presenting with medically refractory erectile dysfunction (ED) may actually be more bothered by decreased libido secondary to depression, reduced frequency of intercourse secondary to partner issues, or embarrassment with penile length. His goals with surgery may be to improve these other conditions, rather than just the erection itself. If the patient receives a PP, he is at high risk for dissatisfaction, as a PP is not able to address these other issues.
Potential surgical patients must also have the psychological capacity to handle all potential post-operative scenarios. Although most patients may experience a good outcome, complications will invariably occur. If a patient does not have the psychological reserve or ability to cope with a significant complication, he is a poor surgical candidate (30). Similarly, patient expectations must be within the ability of the surgeon and the surgical procedure to address. By definition, a patient with unreasonable expectations cannot be satisfied, even in the setting of a good post-operative result.
From a practical standpoint, it is often difficult to identify which patients do and do not have sufficient reserve to handle complications, particularly in referral or busy surgical practices, where clinicians may need to decide on surgery after a single office visit. To address this need, the mnemonic “CURSED Patient,” for compulsive, unrealistic, revision, surgeon shopping, entitled, denial, and psychiatric has been suggested to identify patients who are at high risk of dissatisfaction (31). Although the mnemonic was originally described for men undergoing PP, it is likely applicable to many other surgical areas. See Table 1 for additional details regarding traits included in the “CURSED Patient” mnemonic.
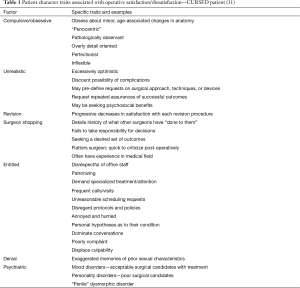
Full table
Surgeon factors
Surgeons should trust their own intuition or “gut-feeling” stemming from patient encounters in regard to patient readiness for surgery. It is important to remember that some poor surgical candidates may not fit into the CURSED Patient pneumonic. At the same time, surgeons should empower their entire office staff to feel comfortable informing the surgeon that they feel the patient is a poor surgical candidate. Thus, surgical schedulers, administrative assistants, medical assistants, nurses and advanced practice providers should have surgical readiness “veto” power.
Surgeons also have varied capacities to psychologically cope with complications, and this should influence the selection of operative candidates. Even early predictors of responses to complications during residency or fellowship often are unable to mirror the challenges of complications encountered once one is ultimately responsible. Although surgeons may feel as if their experiences are unique, they often undergo four similar phases of response: the kick (‘am I good enough’), the fall (‘was it my fault’), the recovery (‘what can I learn’), and the long-term impact (32). Surgeon burn-out is also related to this phenomenon. An entire article is dedicated to this topic later on in this special edition to help surgeons develop tools to prepare for and deal with complications.
Patient selection is further influenced by surgeon factors. As nearly all skills are dependent on the frequency of repetition, a low-volume surgeon with limited specialty training is likely to have a higher rate of complications and reduced outcomes compared to one who is higher-volume and more experienced at a specific procedure (33). At the same time, inexperienced surgeons (even those with fellowship training) just starting their surgical careers often feel pressured to “get busy” quickly and are excited to implement their craft that they have been studying for 5 or more years. Without proper recognition, this may result in overly optimistic pre-operative counseling which minimizes complications and exaggerates positive outcomes.
The breadth of surgical techniques available to a surgeon also impacts patient selection. A 30-year-old male with ED secondary to arterial insufficiency and an isolated vascular occlusion may benefit from an arterial bypass surgery. However, if a surgeon is uncomfortable performing this procedure, he/she may elect to proceed with a PP, which may not be the optimal choice in this particular case.
These statements should not be interpreted to suggest that only high-volume surgeons who have the complete breadth of surgical ability should be operating. Rather, it indicates that surgeons should understand when a patient would most benefit from alternative procedures that they may not offer, potentially avoid surgery in complex cases, refer when appropriate, and appropriately counsel patients as to anticipated expectations. Additional training may also be warranted to improve skills or expand surgical offerings. This is particularly the case with procedures associated with a high risk of significant and permanent complications, such as incision/partial excision and grafting for PD, complex penile reconstructions, revision/salvage PP, neophallus procedures, vascular reconstruction, or similar surgeries.
Beyond surgical skill, surgeons may have relevant conflicts of interest that impact their ability to provide an impartial recommendation. In an idyllic setting, if a surgeon’s salary is linked to a specific surgical procedure, the decision for surgery should optimally be made by an uninvolved 3rd party. Although the surgeon would retain the ability to decide if the patient were healthy enough and a good candidate for the procedure, the decision as to surgery versus non-surgical alternatives should be left to one who does not have a financial conflict of interest. Ironically, the majority of surgical centers utilize an opposite model, where the surgeon decides on which therapy is given, while the decision as to fitness for surgery is left to medical colleagues.
Likelihood of a successful outcome
Appropriate patient selection includes the integration of each of the previously discussed factors (patient non-psychological, patient psychological, surgeon) in a dynamic model (see Figure 1 for graphical representation). Using this model, patient psychological capacity, patient expectations, the complexity of the surgical case, and surgeon volume are combined to determine the overall likelihood for a successful outcome, both technically as well as relating to patient satisfaction.
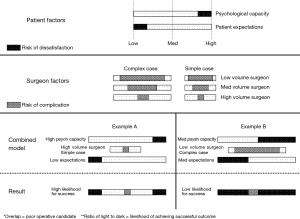
To illustrate the model, first, a patient’s psychological capacity is determined. A higher capacity results in a bar that is mostly white, while a low capacity is mostly black. Second, the patient expectations are determined. Those with low expectations exhibit a bar that is mostly white, while those with high expectations have one that is mostly black. Third, the complexity of the case is selected. A complex case results in a wider grey band (i.e., wider standard deviation of results), while a simple case exhibits narrower bands. And finally, the surgeon volume is considered. Those with low volumes have wider grey bands, signifying a higher risk for complications. The four factors are then combined into one final bar, with higher ratios of light to dark colors representing a higher likelihood for a successful outcome. In “Example A,” a high-volume surgeon performing a simple case on a patient with high psychiatric capacity and low expectations is very likely to achieve a successful outcome. In contrast, “Example B” demonstrates a low-volume surgeon performing a complex case in a patient with medium psychiatric capacity and expectations has a low likelihood for “success”. If any of the bars overlap (as in “Example B”), the patient is a poor operative candidate.
Counseling
Patient counseling is an important component in achieving optimal outcomes. As overall satisfaction relates to the entirety of a patient’s experience, appropriate counseling helps manage all aspects of care outside of surgery itself. This may include setting reasonable expectations, reviewing anticipated risks, optimizing post-operative compliance to reduce complications, and providing ongoing support for the patient’s condition. Counseling is also a key factor in the process of mutual decision-making (see Figure 2).
Setting expectations
Setting expectations begins with obtaining a thorough history. A notable quote from a lead Yale Industrial Engineer is instructive, “If I had only one hour to solve a problem, I would spend up to two-thirds of that hour in attempting to define what the problem is.” (34). This concept of accurately defining the underlying concern is particularly relevant in regards to andrological surgery, where the true chief complaint may not be immediately evident. A PD patient may be assumed to seek a correction in curvature, when in fact he may seeking a return of normal penile length, treatment of indentation deformities, enhancement of penile rigidity beyond the diseased region, improvement in self-confidence, or restoration of his prior sexual intimacy. Appropriate treatment for these varied complaints may, therefore, range from use of penile traction or a vacuum device, to penile plication, incision/excision and grafting, placement of a PP, or counseling alone. Completely understanding patients’ primary and secondary complaints is a key differentiator between simply performing successful surgery and actually treating their ‘condition’. This concept is highlighted by Welliver and colleagues who elegantly demonstrated that only 50% men treated for lower urinary tract symptoms had their chief complaint of nocturia treated effectively using traditional BPH treatment algorithms by a BPH expert (35).
Once patient expectations are fully established, the surgeon may then address the ability or inability of a specific treatment modality to achieve these expectations. This discussion is ideally based on surgeon-specific outcomes rather than quoting other published literature. If other surgeons’ numbers are quoted, this should be expressly indicated during the discussion, so as to avoid any misrepresentation or misunderstanding. Good patient counseling (and ultimately good patient selection) begins with good record keeping.
Discussing risks
Perhaps no component of patient counseling is ‘re-lived’ more often after the fact than anticipated risks with surgery. Patients who experience complications will often feel that these risks were not discussed prior to surgery, particularly in cases of severe adverse effects. This is complicated by the fact that it is clearly not possible for a surgeon to anticipate or discuss all potential risks of a given procedure. As an example, a recent patient treated with a PP in our practice developed Shingles immediately after surgery. The infection resulted in him experiencing a prolonged partial paralysis of half of his face that remains indeterminate at the present time. This type of complication is clearly very difficult to predict, and the rarity precludes ability to thoroughly and accurately discuss in any setting.
Given these limitations, one potential discussion strategy revolves around reviewing a ‘best case’, ‘worst case’, and ‘most likely case’ set of scenarios. Patients may then be reviewed the likelihood for common complications if known. The natural tendency to minimize the possibility of complications to encourage a patient to proceed with surgery should also be recognized and avoided. This is particularly an issue in the current era of medical consumerism and fee-for-service, where surgeons are also expected to be salesmen and are essentially paid on commission in many cases. To limit this tendency, surgeons may consider having a 3rd party individual involved in the informed consent portion of discussions. Alternatively, or in addition, this information may be made available in written form for patients to review at a later time. Otherwise, while information delivered before surgery is considered informed consent, the same discussion after surgery is viewed as an excuse.
Post-operative counseling
Post-operative counseling is an important aspect of optimizing outcomes and patient satisfaction. Often, surgeons go to extensive lengths to assure operative success but then perform limited post-operative counseling or follow-up. Appropriate counseling may reduce complications and most certainly leads to an enhanced relationship between the patient and surgeon. Key components of post-operative counseling include how to appropriately manage the wound, restricting selected physical activities, and monitoring for potential significant complications.
In the case of post-operative complications, the frequency of patient contact should be increased. This runs counter to a natural tendency to avoid, redirect blame, and minimize post-op issues. However, in this challenging time, patients are often seeking additional support and wish to know that they have not been abandoned in their extremity. In a study of 100 successive legal claims, 37% stemmed from poor communication from the patient’s ability to accept or understand the natural course of their disease (36). In cases where patients are suggesting that inappropriate care has been delivered, it is also helpful to have another surgeon in the community to whom you can refer for a second opinion when needed.
Another important aspect of post-operative counseling is the use of long-term follow-up. This can be performed with routinely administered surveys or via follow-up visits in clinic. Although not all patients will take advantage of these points of interaction, they are an important aspect of care, as they provide an avenue where patients can discuss longer-term concerns or issues that may require additional therapies. In the absence of these visits, patients may feel uncomfortable in approaching their original surgeon with concerns about specific undesirable outcomes.
Additionally, long-term follow-up helps in all other aspects of patient selection and counseling, as it provides further data on anticipated outcomes and predictors of success. As satisfaction measured at one point in time may not reflect later outcomes, ongoing surveys help to better understand the process and timing of satisfaction, in a similar way that Kaplan-Meier curves help to more fully understand the impact of cancer treatments on disease-specific and overall survival. It is an interesting observation that many ‘highly successful’ practices emphasize high rates of primary and low rates of rates of revision surgeries, when in reality, this likely only highlights that patients are going elsewhere after an initial experience. In the arena of consumer retail, return customers are often a better indicator of overall satisfaction than ‘total sales’. Publication (the tendency to only publish good results) and attrition bias (only reporting on the patients who follow up with that provider) is rampant in the Andrology literature, likely overestimating successful patient outcomes.
Two examples from our surgical practice highlight the importance of appropriate post-operative counseling. In the first example, a patient who had undergone placement of a PP experienced an unexpected post-operative complication of Ogilvie syndrome, renal failure, and pneumonia, requiring a prolonged hospital stay. The patient was also very disappointed in his post-operative penile length, which he indicated had not been accurately discussed pre-operatively. Although he was not on a urology service while in the hospital, attempts were made to visit him daily until final dismissal. Post-operative surveys were also sent, to which the patient replied regularly and very negatively. The patient was contacted after each survey to attempt to address any specific concerns, and ultimately, he returned to the office to discuss further. At that point, he was referred to another andrological surgeon for a second opinion. With subsequent surveys, the patient began indicating overall satisfaction with the procedure, and years later he re-presented for revision surgery after the initial device experienced a mechanical malfunction.
In the second example, a patient was counseled to pull down on a PP pump to assure appropriate positioning within the scrotum. However, in our practice, we routinely use liposomal bupivacaine, which results in prolonged numbing of the surgical site. The patient proceeded to routinely pull down aggressively on the pump over the next several days. Less than one week after the surgery, he called reporting some concerns and was seen in the office. On exam, we observed that he had pulled so aggressively, that he had essentially pulled open three layers of closure of the penoscrotal incision. This experience led us to discontinue the practice of having patients pull on the pump, and ultimately, it provides an example of how appropriate or inappropriate counseling is directly associated with complications.
Achieving an optimal balance
Time is a finite resource, and often surgeons are pulled between many competing priorities. Particularly in an era of diminishing reimbursement and fee-for-services, surgeons are often left to balance a need to see more patients and perform more surgery in shorter periods of time and with fewer resources. Often these pressures lead to relaxed patient selection and reduced time spent in counseling.
To offset these limitations, many contemporary practices utilize various methods, including educational brochures or videos to assist in patient education and counseling. Additionally, some attempt to cluster discussions via group visits, or have nurses or advanced practice providers perform much of the pre- and post-operative visits. Each of these highlights the concept that modern medicine is increasingly dependent on team-based approaches to patient care, with less and less reliance on the physician to perform all aspects alone.
Consequences of poor patient selection and counseling
There are many potential consequences that may originate from poor patient selection and counseling. Perhaps the most important is the possibility of direct patient harm. This may occur due to a lack of surgical competency, selection of incorrect surgical procedure, or baseline patient comorbidities. Harms may result directly from the surgery or anesthesia itself, or indirectly through development or worsening of side effects (i.e., ED after PD surgery).
Other consequences may include patient and surgeon dissatisfaction, reduced success rates, or lack of surgical confidence. In the most severe cases, inappropriate patient selection and counseling can result in potential personal injury, lawsuits, or even investigations for fraud or misconduct. This may also lead to a loss of credibility, both to patients as well as to the broader scientific community. Given the severity of these potentially avoidable consequences, it is clearly in the surgeon’s best interest to focus on enhancing not only the surgical procedure itself, but also to improve the quality and volume of education delivered pre- and post-operatively.
Summary
The concept of surgical success is an elusive concept that is variably defined. When viewed from a patient-care perspective, it likely includes many factors beyond traditionally reported outcomes, and centers on the ability to address the patient’s underlying objectives and expectations. To optimize a successful outcome, the surgeon must therefore be adept at multiple aspects of patient care including in obtaining the initial history, patient selection, operative capabilities, perioperative counseling and long-term patient follow-up. All of this must also be performed with a baseline understanding as to factors predisposing patients to satisfaction or dissatisfaction with a given procedure.
In this context, an ideal surgeon is not only technically skilled in accomplishing a surgery, but is also able to assess and meet expectations, perform the right procedure for the right indication, is not financially conflicted (or has methods of reducing potential conflicts of interest), accurately determine which patients have the psychological capacity to undergo surgery, provide thorough pre- and post-op counseling, and follow outcomes long-term. In contrast, traits of a suboptimal surgeon include poor surgical skill, inability to recognize and/or treat complications, refusal to refer complex patients or those who would benefit from therapies offered by others, being overly selective or lenient of patients (fear of complications vs. motivated by finances or other personal gain), presence of financial or other conflicts of interest, and lack of interest in performing thorough counseling and long-term follow-up.
The incorporation of enhanced patient selection and counseling offers the possibility for improving patient satisfaction and overall outcomes. Additionally, it may limit potential adverse consequences including patient or personal harm, lawsuits, impaired credibility or other similar effects.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Köhler is a consultant for both Boston Scientific and Coloplast Corporation. All other authors have no relevant disclosures.
References
- Mohajer ST. Urologist shot dead in exam room; man in custody. 2013. Available online: http://www.sandiegouniontribune.com/sdut-urologist-shot-dead-in-exam-room-man-in-custody-2013jan29-story.html
- Coker M. Stanwood Fred Elkus, Alleged Murderer of Dr. Ronald Gilbert, Surrenders Assets to Family. 2014. Available online: http://www.ocweekly.com/news/stanwood-fred-elkus-alleged-murderer-of-dr-ronald-gilbert-surrenders-assets-to-family-6453932
- Althof SE, Corty EW, Levine SB, et al. EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology 1999;53:793-9. [Crossref] [PubMed]
- Rosen RC, Riley A, Wagner G, et al. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997;49:822-30. [Crossref] [PubMed]
- Pineda M, Burnett AL. Distinguishing Failure to Cure From Complication After Penile Prosthesis Implantation. J Sex Med 2017;14:731-7. [Crossref] [PubMed]
- Pineda M, Burnett AL. Response and Rebuttal to Editorial Comment on "Distinguishing Failure to Cure From Complication After Penile Prosthesis Implantation". J Sex Med 2017;14:740. [Crossref] [PubMed]
- Trost L. Editorial Comment on "Distinguishing Failure to Cure From Complication After Penile Prosthesis Implantation". J Sex Med 2017;14:738-9. [Crossref] [PubMed]
- Kramer AC, Schweber A. Patient expectations prior to coloplast titan penile prosthesis implant predicts postoperative satisfaction. J Sex Med 2010;7:2261-6. [Crossref] [PubMed]
- Colakoglu S, Khansa I, Curtis MS, et al. Impact of complications on patient satisfaction in breast reconstruction. Plast Reconstr Surg 2011;127:1428-36. [Crossref] [PubMed]
- Hellings PW, Nolst Trenite GJ. Long-term patient satisfaction after revision rhinoplasty. Laryngoscope 2007;117:985-9. [Crossref] [PubMed]
- Meyer L, Jacobsson S. The predictive validity of psychosocial factors for patients' acceptance of rhinoplasty. Ann Plast Surg 1986;17:513-20. [Crossref] [PubMed]
- Akin-Olugbade O, Parker M, Guhring P, et al. Determinants of patient satisfaction following penile prosthesis surgery. J Sex Med 2006;3:743-8. [Crossref] [PubMed]
- Gittens P, Moskovic DJ, Avila D Jr, et al. Favorable female sexual function is associated with patient satisfaction after inflatable penile prosthesis implantation. J Sex Med 2011;8:1996-2001. [Crossref] [PubMed]
- Flores S, Choi J, Alex B, et al. Erectile dysfunction after plaque incision and grafting: short-term assessment of incidence and predictors. J Sex Med 2011;8:2031-7. [Crossref] [PubMed]
- Alphs HH, Navai N, Kohler TS, et al. Preoperative clinical and diagnostic characteristics of patients who require delayed IPP after primary Peyronies repair. J Sex Med 2010;7:1262-8. [Crossref] [PubMed]
- Mulhall J, Anderson M, Parker M. A surgical algorithm for men with combined Peyronie's disease and erectile dysfunction: functional and satisfaction outcomes. J Sex Med 2005;2:132-8. [Crossref] [PubMed]
- Montorsi F, Rigatti P, Carmignani G, et al. AMS three-piece inflatable implants for erectile dysfunction: a long-term multi-institutional study in 200 consecutive patients. Eur Urol 2000;37:50-5. [Crossref] [PubMed]
- Goldstein I, Newman L, Baum N, et al. Safety and efficacy outcome of mentor alpha-1 inflatable penile prosthesis implantation for impotence treatment. J Urol 1997;157:833-9. [Crossref] [PubMed]
- Minervini A, Ralph DJ, Pryor JP. Outcome of penile prosthesis implantation for treating erectile dysfunction: experience with 504 procedures. BJU Int 2006;97:129-33. [Crossref] [PubMed]
- Deveci S, Martin D, Parker M, et al. Penile length alterations following penile prosthesis surgery. Eur Urol 2007;51:1128-31. [Crossref] [PubMed]
- Knoll LD, Henry G, Culkin D, et al. Physician and patient satisfaction with the new AMS 700 momentary squeeze inflatable penile prosthesis. J Sex Med 2009;6:1773-8. [Crossref] [PubMed]
- Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med 2011;8:2112-7. [Crossref] [PubMed]
- Porena M, Mearini L, Mearini E, et al. Penile prosthesis implantation and couple's satisfaction. Urol Int 1999;63:185-7. [Crossref] [PubMed]
- Anafarta K, Yaman O, Aydos K. Clinical experience with Dynaflex penile prostheses in 120 patients. Urology 1998;52:1098-100. [Crossref] [PubMed]
- McLaren RH, Barrett DM. Patient and partner satisfaction with the AMS 700 penile prosthesis. J Urol 1992;147:62-5. [Crossref] [PubMed]
- Whalen RK, Merrill DC. Patient satisfaction with Mentor inflatable penile prosthesis. Urology 1991;37:531-9. [Crossref] [PubMed]
- Mulcahy JJ, Carson CC 3rd. Long-term infection rates in diabetic patients implanted with antibiotic-impregnated versus nonimpregnated inflatable penile prostheses: 7-year outcomes. Eur Urol 2011;60:167-72. [Crossref] [PubMed]
- Antonini G, Busetto GM, De Berardinis E, et al. Minimally invasive infrapubic inflatable penile prosthesis implant for erectile dysfunction: evaluation of efficacy, satisfaction profile and complications. Int J Impot Res 2016;28:4-8. [Crossref] [PubMed]
- Mohamed ER, Hammady AR, Eldahshoury MZ, et al. Surgical outcomes and complications of Tube(R) (Promedon) malleable penile prostheses in diabetic versus non-diabetic patients with erectile dysfunction. Arab J Urol 2016;14:305-11. [Crossref] [PubMed]
- Adamson PA, Litner JA. Psychologic aspects of revision rhinoplasty. Facial Plast Surg Clin North Am 2006;14:269-77. v. [Crossref] [PubMed]
- Trost LW, Baum N, Hellstrom WJ. Managing the difficult penile prosthesis patient. J Sex Med 2013;10:893-906. [Crossref] [PubMed]
- Luu S, Patel P, St-Martin L, et al. Waking up the next morning: surgeons' emotional reactions to adverse events. Med Educ 2012;46:1179-88. [Crossref] [PubMed]
- Henry GD, Kansal NS, Callaway M, et al. Centers of excellence concept and penile prostheses: an outcome analysis. J Urol 2009;181:1264-8. [Crossref] [PubMed]
- Markle WH. The Manufacturing Manager's Skills. In: Finley RE, Ziobro HR. editors. The Manufacturing Man and His Job. New York: American Management Association Inc., 1 966:18.
- Welliver C, Sulaver R, Whittington A, et al. Analyzing Why Men Seek Treatment for Lower Urinary Tract Symptoms and Factors Associated With Nonimprovement. Urology 2015;86:862-7. [Crossref] [PubMed]
- Neale G. Clinical analysis of 100 medicolegal cases. BMJ 1993;307:1483-7. [Crossref] [PubMed]