Transperineal vs. transrectal biopsy in MRI targeting
Introduction
Biopsy currently remains the gold standard of prostate cancer diagnosis. Although imaging with multiparametric magnetic resonance imaging (mpMRI) has the potential to increase detection and localisation of prostate cancer, tissue is still required for histological confirmation. It is estimated that more than 2 million prostate biopsies are performed around the world every year (1).
MRI-targeted transrectal biopsy (TRB)
The prostate’s anatomical location lends itself to a transrectal approach for biopsy which has therefore been the standard route for decades. Initially finger-guided (2), then guided by transrectal ultrasound (TRUS) probes, TRB can be performed in the office in just 10 min. Historically, men underwent a sextant TRB without any pain relief. However, patients often complained that the biopsy was the worst part of their prostate cancer journey. Thus, the compliance for repeat biopsy in the context of active surveillance has been poor (3). The minimum standard of care for pain relief has now been set as periprostatic infiltration of local anaesthesia (PILA) (4,5), however, this is not always adequate, and does not address the discomfort of initial TRUS probe insertion. Further study in TRB analgesia is therefore required and is indeed underway (ACTRN12615001105538 – Painfree TRUS B) (6).
Whether using cognitive fusion, MRI-US fusion software or in-bore MRI-guided biopsy, the most common approach for MRI-targeted prostate biopsy remains transrectal. Most MRI-US fusion software products (Table 1) are based on the transrectal approach (7,8), and in-bore MRI-guided biopsy is typically performed this way (9,10) with rare exceptions (11,12).
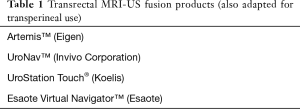
Full table
However, in our opinion TRB has serious disadvantages, which are becoming increasingly important. In TRB the biopsy needle must pass through the rectal wall. If only targeted biopsies are performed, this may be as few as twice, but if saturation biopsies are performed as well, it could be more than 24 times. Each needle passage risks inoculating the prostate and its rich blood supply with rectal bacteria. As a “dirty” procedure, prophylactic antibiotics are necessary and fluoroquinolones are currently recommended as the antibiotics of choice (1,13). However, there are three major concerns regarding the widespread use of fluoroquinolones in TRB.
First, in July 2016 the U.S. Food and Drug Administration (FDA) issued a safety announcement that fluoroquinolones should not be used unless there are no other options due to the risk of “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient” (14). The FDA has previously issued a strong warning on the risks of fluoroquinolone use, but they were recently revised due to further analysis of post-marketing reports of these long-term side effects that involved two or more body systems. Based on this warning, continued widespread use of TRB will therefore require other broad-spectrum antibiotics, or a combination of them, which is also highly problematic (see below).
Second, despite being the recommended prophylactic antibiotic, fluoroquinolones are losing their efficacy due to rising rates of resistance in rectal flora (15-17) and there is evidence that sepsis rates are consequently rising (1). Nam et al reported a population-based study of over 75,000 men in Canada undergoing TRB in the 10 years to 2005. The infective re-admission rate rose from 0.6% to 3.6% over this period (18). More recently, Anastasiadis et al. reported on nearly 200,000 men in the English national cancer registry from 2000 to 2008 (19). They found a 70% increase in re-admission for infection over this period. In addition, Patel et al reported in a series of 316 consecutive patients undergoing TRB in London over 2 years to 2010 that, despite routine use of prophylactic ciprofloxacin, 5% were re-admitted to hospital for infection (20). Of the 16 patients re-admitted, 10 were culture-positive and all grew multi-resistant E. coli. Recent travel or antibiotic use were cited as risk factors.
In Australia, where prescription of fluoroquinolones is restricted, a population-based study was reported in the state of Victoria for infective re-admission following TRUS biopsy over a 5-year period to 2012. In Roth et al.’s study of nearly 35,000 cases, there was no overall rise in infective re-admission, which was 1.7% over the period with a mean cost of US$6,844 per re-admission (21). Similarly, a more recent statewide study of New York State also found a median cost of post-TRB infection at US$4,129 per case (22). The risk of post-TRB sepsis has clearly caused concern amongst clinicians, as evidenced by an increasing rate of the use of prophylactic carbapenems. Leahy et al studied this in a single high-volume Victorian institution and found that in nearly 2,000 men undergoing consecutive TRB over 4 years to 2012, carbapenem prophylaxis rose from 0 to 13% (23).
The third concern regarding the widespread use of fluoroquinolones in TRB is its potential to exacerbate development of bacterial resistance. The U.S. Center for Disease Control (CDC) advises that antibiotic use is the single most important factor for development of resistance (24), and the World Health Organisation (WHO) warns that if we persist with our current practice of antibiotic use, we are headed for a post-antibiotic era (25).
Some groups have argued for use of either combination antibiotic prophylaxis or routine use of carbapenem prophylaxis. In shifting to multi-drug prophylaxis or culture-specific prophylaxis after use of rectal swabs, the Michigan Urological Surgery Improvement Collaborative (MUSIC) showed a drop in infective re-admission from 1.2% to 0.6% (26). In New Zealand, prophylactic use of ertapenem resulted in a zero sepsis rate (27) and in Leahy et al.’s study of a single institution assessing the rate of prophylactic carbapenem use for TRB, none of those who received it were re-admitted for infection (23). However, these measures go directly against recommendations from the CDC and WHO, as more or more powerful antibiotics are being used as a substitute for basic hygienic technique. Whilst there is some evidence that the use of rectal disinfectant agents such as povidone-iodine (28,29) or formalin (30) may reduce post-TRB infections, neither avoids the need for prophylactic broad-spectrum antibiotics and their waning efficacy.
Where only the transrectal route is available for prostate biopsy, we strongly encourage rectal swab culture and subsequent targeted antibiotic prophylaxis to be routine practice. Both meta-analysis and systematic reviews have shown targeted prophylaxis to significantly reduce infection rates (3.3–4.6% to 0.3–0.7%) when compared to empirical prophylaxis in TRB (31-33).
Performing only MRI-targeted biopsy via the transrectal route may allow as few as 1 or 2 cores to be taken. However, there is scant evidence that this reduces infection risk. In Borghesi et al.’s recent systematic review (1), only one study of 54 cases is cited showing a possible benefit, but it was not statistically significant (34).
MRI-targeted transperineal biopsy (TPB)
For all the above reasons, TPB is gaining wider acceptance and becoming more commonly used (35). TPB is usually performed under general anaesthesia, with obvious ramifications for use of hospital resources, however TPB under local anaesthesia has been reported (36). In TPB, whether via a brachytherapy grid, robotic-guidance or freehand, all cores are taken by passing the trocar through the perineal skin. The skin is prepared with a disinfectant agent as for any other surgical procedure. As neither the gastro-intestinal or urinary tracts are traversed, TPB should be considered a “clean” procedure. The exceedingly low risk of sepsis seen in evidence to date supports this.
In 2014, Grummet et al. published their multi-centre series of 245 consecutive TPB cases showing an infective re-admission rate of zero. They also performed a literature review of infectious complications after TPB and found a rate of just 0.076% when pooling 6,609 cases (37), still far lower than the lowest rates reported for TRB using targeted prophylaxis. Grummet’s group has since updated their prospective series of TPB which is now at 1,194 consecutive cases performed by 6 urologists at 5 centres across Melbourne, Australia (38). The re-admission rate for infection remains at zero. Importantly, a change of practice occurred during this series such that in the latter 710 cases (59.5%) prophylaxis was by a single dose of intravenous cephazolin, only a first-generation cephalosporin antibiotic (39). This series, where data was collected on a prospective database with 100% follow-up, shows that post-biopsy sepsis can be eliminated from practice by using TPB, and by using it without fluoroquinolones, let alone carbapenems. This practice is in line with the current recommendations by Australia’s Therapeutic Guidelines publication, which recommends cephazolin only for TPB prophylaxis (40).
TPB also lends itself well to performing MRI-targeted biopsies using either cognitive fusion or MRI-US fusion software by providing a stable platform. Cognitive fusion TPB is typically performed using a brachytherapy grid which is fixed against the perineum by the stepper and stabilizer. The corresponding grid hole co-ordinates are displayed on the ultrasound monitor. Following rectal insertion of the ultrasound probe, cores are taken in the longitudinal plane of the prostate from apex to base, with imaging in both sagittal and transverse planes for excellent position localization. The 5mm grid hole spacing permits adjustment for imperfect biopsy needle placement by moving to an adjacent grid hole in any direction, using the previous grid hole co-ordinates as a reference point. As the biopsy trocar must pass through soft tissue to reach the prostate, there can be minor deviation of the needle tip. This can be adjusted for by employing the bevel of the trocar, pointing the tip in the direction of preferred deviation. Using the above technique for cognitive fusion TPB, MRI-targeted biopsy can be performed with excellent precision in experienced hands (10) (see data in other sections of this journal edition).
Some fusion software products (e.g., BiopSee, BioJet) utilize a brachytherapy grid to enable MRI-US fusion TPB. Once the ultrasound images of the prostate are captured, the MRI images, with suspicious lesions previously marked out, are fused using either rigid or elastic algorithms. For MRI-targeted biopsy, cores are then taken via the appropriate grid holes to ensure sampling of the designated area. The size of the lesion and clinician preference determine the number of targeted cores taken. If saturation or template cores are taken as well as targeted cores, very high numbers of cores could be taken. Whilst some cores are taken at different depths through the same grid hole to ensure both apex and base are sampled, most cores are taken via separate skin punctures.
MRI-US fusion TPB can also be performed without a brachytherapy grid. The iSR’obot Mona Lisa is a robotic device which enables TPB via just two perineal skin punctures (41) and takes around half an hour for a standard biopsy. Each puncture site acts as a pivot point, giving a biconical configuration of core positions. Once the TRUS probe has acquired 1mm-slice transverse images from base to apex to create a 3-dimensional model, the previously acquired MRI images, along with suspicious areas again marked out, are fused to the ultrasound model. The Mona Lisa’s biopsy guide point is positioned to touch the perineal skin and the device then automatically creates positioning of all targeted cores, and/or template cores if desired. The biopsy guide point moves to the position of the first core to be taken on the right side of the gland, accounting for angle and depth. The clinician fires the trocar, checking the ultrasound monitor for the typical “flash” of the needle tip as seen in the transverse plane.
There are currently no head-to-head comparisons of TPB using MRI-US fusion software products (Table 2), nor are there comparison studies within TPB of cognitive versus software fusion. However, within TPB, MRI-targeted biopsy has been compared to saturation biopsy. Radtke et al. reported on 294 consecutive men undergoing TPB, comprising 186 initial biopsies and 108 repeat biopsies (42). All men underwent template biopsy using the Ginsburg protocol (43) and those who had suspicious lesions on MRI also underwent MRI-targeted biopsy using the BiopSee system. With significant cancer defined as grade group 2 or greater and targeting PI-RADS 3–5 lesions, systematic template biopsies missed 21% and MRI-targeted biopsies missed 20%. They concluded that, using TPB, MRI-targeted biopsies detected at least as many significant cancers as systematic template biopsies, and that both approaches should be used for optimal cancer detection. This has been validated using radical prostatectomy specimens in which MRI-targeted fusion TPB and saturation TPB together reliably detected 97% of significant cancer foci (44). However, the combined biopsy approach, while missing a lesser number of significant lesions, comes at the cost of detecting more insignificant cancer.
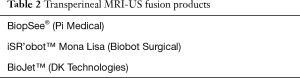
Full table
The only comparative study within TPB compared in-bore MRI-targeted TPB using a manual template versus a robotic template. In a series of 99 cases, Tilak et al. found higher needle placement accuracy in the robotic template group (12). However, procedures took a mean duration of between 90 and 100 min each. Not only would this be difficult for patients to tolerate, the duration of this approach does not seem to be feasible in a routine clinical setting.
To our knowledge, the only study comparing MRI-targeted TRB to MRI-targeted TPB was recently published by Pepe et al. (45). In the setting of repeat biopsy, 200 men underwent mpMRI followed by saturation TPB (28-34 cores). At the same procedure, men who had a suspicious lesion on mpMRI (PI-RADS 4 or 5) underwent both MRI-targeted TRB using fusion software and MRI-targeted TPB (4 cores each) using cognitive fusion. Using the saturation biopsy as the reference standard, clinically significant cancer was found in 60 cases (30%) and all were detected on mpMRI. Twenty cases were missed by MRI-targeted software fusion TRB but only 4 cases were missed by MRI-targeted cognitive fusion TPB. Within the anterior zone only, TRB missed 12 significant cancers to TPB’s 1 (P=0.001).
However, there are several issues with this study. First, significant cancer was defined as ≥2 cores of ≥ grade group 1 (Gleason 6) cancer. In the current context of saturation biopsy and targeted cores, where tumours can be pinpointed, resulting in maximal detection of highest grade and longest length of tumour, this seems too broad a definition. Clinically meaningful results could have been obtained if the definition of ≥ grade group 2 had been used. Unfortunately this data is not supplied and therefore cannot be deduced. Second, TRB with fusion software is compared to TPB using cognitive fusion. It is therefore impossible to determine whether the anatomical approach or the type of fusion is responsible for the differences seen, however, it is suggested that the TPB approach allowed superior access to the anterior aspect of the gland. As a type of fusion was used in both approaches however, one would expect this apparent deficit of TRB to have been overcome. Finally, apart from being stated as rigid fusion, no information is given on the actual form of fusion software used.
Summary
All three methods of MRI-targeted biopsy for prostate cancer diagnosis (cognitive fusion, MRI-US fusion software, and in-bore MRI-guided biopsy) can be performed via either the transrectal or transperineal approach (Table 3). TRB is still the most common approach but TPB usage is increasing. Evidence comparing detection rates of significant cancer involving MRI-targeted TPB is not as rich as for TRB. However, the limited data available suggest that MRI-targeted TPB is as good as systematic template TPB and that the transperineal approach may confer an advantage for detecting anterior tumours, even in an MRI-targeted context. At present, we recommend a combination of both MRI-targeted and systematic TPB for patients with a suspicious lesion on MRI who aim for optimal significant cancer detection and accept a higher risk of diagnosis of indolent disease. In future, this approach might change to use of targeted cores only, but further studies such as PRECISION are needed in this context (ClinicalTrials.gov Identifier: NCT02380027) Studies are also needed to compare the different fusion software products as well as cognitive fusion within TPB.
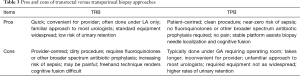
Full table
Given the equivalent or superior detection rates of significant cancer with TPB compared to TRB, the next most important consideration is patient safety. TRB carries a small but clinically significant and increasing risk of sepsis. TPB, whether MRI-targeted or not, consistently results in zero or near-zero rates of serious infection (1). Furthermore, it has now been shown that fluoroquinolones or other combinations of broad-spectrum antibiotics are not necessary for prophylaxis in TPB.
Being typically performed under general anaesthesia (but with possibilities for use under local anaesthesia only), TPB clearly requires substantial use of hospital resources, including operating room time and personnel. Its uptake depends largely on the health system context. In Australia for example, many TRB procedures are already performed under IV sedation in operating theatres, therefore the switch to TPB is not such a leap to make. We recognize that in most other parts of the world, TRB is performed using only local anaesthesia in the urologist’s office, making the switch to TPB far more difficult. Our routine practice, where all men needing prostate biopsy undergo TPB, proves that it can be done, but cost effectiveness studies are clearly required.
In addition, evidence continues to emerge supporting the avoidance of biopsy in MRI-negative men (46,47) and conducting ongoing observation instead (“neo-active surveillance”) if other risk factors are low. It has been suggested that up to half of all prostate biopsies could be avoided this way (9,48), which would go a long way to mitigating the strain on health resources required of TPB. Furthermore, if we are to truly strive for the best possible care of our patients over what is convenient for hospitals and clinicians, we must embrace the various methods of MRI-targeted TPB.
In the current environment of patient-centred care and of warnings that our current misuse of antibiotics will lead us into a post-antibiotic era, TPB satisfies both patient demand for the safest possible method of prostate biopsy and health authorities’ demands for antibiotic stewardship, such that we believe TRB will play a minor role in future. Until then, where TRB is performed, it should be MRI-targeted, with PILA as a minimum for analgesia. Men scheduled to undergo TRB should be assessed for risk factors for multi-drug-resistant rectal flora, such as overseas travel or recent antibiotic use, with subsequent use of either tailored prophylactic antibiotics depending on rectal culture swab, and/or a disinfectant enema such as with povidone-iodine if TPB is unavailable.
Acknowledgements
None.
Footnote
Conflicts of Interest: J Grummet: paid proctor for Biobot iSR’obot Mona Lisa, Biobot sponsored attendance at UAA ASM 2016; paid by Scanmedics for BK Ultrasound to run TPB Workshop 2014. B Hadaschik has funding from the German Research Foundation and the European Foundation for Urology and has received research support from MedCom and Uromed; none of these sources had any input into this article. The other authors have no conflicts of interest to declare.
References
- Borghesi M, Ahmed H, Nam R, et al. Complications After Systematic, Random, and Image-guided Prostate Biopsy. Eur Urol 2017;71:353-65. [Crossref] [PubMed]
- Scherr DS, Eastham J, Ohori M, et al. Prostate biopsy techniques and indications: when, where, and how? Semin Urol Oncol 2002;20:18-31. [Crossref] [PubMed]
- Bokhorst LP, Alberts AR, Rannikko A, et al. Compliance Rates with the Prostate Cancer Research International Active Surveillance (PRIAS) Protocol and Disease Reclassification in Noncompliers. Eur Urol 2015;68:814-21. [Crossref] [PubMed]
- Autorino R, De Sio M, Di Lorenzo G, et al. How to decrease pain during transrectal ultrasound guided prostate biopsy: a look at the literature. J Urol 2005;174:2091-7. [Crossref] [PubMed]
- Maccagnano C, Scattoni V, Roscigno M, et al. Anaesthesia in transrectal prostate biopsy: which is the most effective technique? Urol Int 2011;87:1-13. [Crossref] [PubMed]
- Huang S, Pepdjonovic L, Konstantatos A, et al. Penthrox alone versus Penthrox plus periprostatic infiltration of local analgesia for analgesia in transrectal ultrasound-guided prostate biopsy. ANZ J Surg 2016;86:139-42. [Crossref] [PubMed]
- Wysock JS, Rosenkrantz AB, Huang WC, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur Urol 2014;66:343-51. [Crossref] [PubMed]
- Valerio M, Donaldson I, Emberton M, et al. Detection of Clinically Significant Prostate Cancer Using Magnetic Resonance Imaging-Ultrasound Fusion Targeted Biopsy: A Systematic Review. Eur Urol 2015;68:8-19. [Crossref] [PubMed]
- Pokorny MR, de Rooij M, Duncan E, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol 2014;66:22-9. [Crossref] [PubMed]
- Wegelin O, van Melick HH, Hooft L, et al. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur Urol 2017;71:517-31. [Crossref] [PubMed]
- Penzkofer T, Tuncali K, Fedorov A, et al. Transperineal in-bore 3-T MR imaging-guided prostate biopsy: a prospective clinical observational study. Radiology 2015;274:170-80. [Crossref] [PubMed]
- Tilak G, Tuncali K, Song SE, et al. 3T MR-guided in-bore transperineal prostate biopsy: A comparison of robotic and manual needle-guidance templates. Journal of magnetic resonance imaging JMRI 2015;42:63-71. [Crossref] [PubMed]
- Walker JT, Singla N, Roehrborn CG. Reducing Infectious Complications Following Transrectal Ultrasound-guided Prostate Biopsy: A Systematic Review. Rev Urol 2016;18:73-89. [PubMed]
- FDA Drug Safety Communication: FDA updates warnings for oral and injectable fluoroquinolone antibiotics due to disabling side effects: U.S. Food and Drug Administration; 2016 [cited 2016 24 September, 2016]. Available online: http://www.fda.gov/Drugs/DrugSafety/ucm511530.html
- Anderson E, Leahy O, Cheng AC, et al. Risk factors for infection following prostate biopsy - a case control study. BMC Infect Dis 2015;15:580. [Crossref] [PubMed]
- Wagenlehner FM, van Oostrum E, Tenke P, et al. Infective complications after prostate biopsy: outcome of the Global Prevalence Study of Infections in Urology (GPIU) 2010 and 2011, a prospective multinational multicentre prostate biopsy study. Eur Urol 2013;63:521-7. [Crossref] [PubMed]
- Williamson DA, Barrett LK, Rogers BA, et al. Infectious Complications Following Transrectal Ultrasound-Guided Prostate Biopsy: New Challenges in the Era of Multidrug-Resistant Escherichia coli. Clin Infect Dis 2013;57:267-74. [Crossref] [PubMed]
- Nam RK, Saskin R, Lee Y, et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J Urol 2013;189:S12-7; discussion S7-8.
- Anastasiadis E, van der Meulen J, Emberton M. Hospital admissions after transrectal ultrasound-guided biopsy of the prostate in men diagnosed with prostate cancer: a database analysis in England. Int J Urol 2015;22:181-6. [Crossref] [PubMed]
- Patel U, Dasgupta P, Amoroso P, et al. Infection after transrectal ultrasonography-guided prostate biopsy: increased relative risks after recent international travel or antibiotic use. BJU Int 2012;109:1781-5. [Crossref] [PubMed]
- Roth H, Millar JL, Cheng AC, et al. The state of TRUS biopsy sepsis: readmissions to Victorian hospitals with TRUS biopsy-related infection over 5 years. BJU Int 2015;116 Suppl 3:49-53. [Crossref] [PubMed]
- Halpern JA, Sedrakyan A, Dinerman B, et al. Indications, Utilization, and Complications Following Prostate Biopsy: a New York State Analysis. J Urol 2017;197:1020-5. [Crossref] [PubMed]
- Leahy OR, O'Reilly M, Dyer DR, et al. Transrectal ultrasound-guided biopsy sepsis and the rise in carbapenem antibiotic use. ANZ J Surg 2015;85:931-5. [Crossref] [PubMed]
- Antibiotic Resistance Threats in the Unites States, 20132013 24 September 2016. Available online: http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf
- Chan M. Combat drug resistance: no action today means no cure tomorrow. 2011 24 September 2016. Available online: http://www.who.int/mediacentre/news/statements/2011/whd_20110407/en/
- Womble PR, Linsell SM, Gao Y, et al. A Statewide Intervention to Reduce Hospitalizations after Prostate Biopsy. J Urol 2015;194:403-9. [Crossref] [PubMed]
- Losco G, Studd R. Post-TRUS sepsis: Targeted use of prophylactic ertapenem for high-risk patients. Melbourne, Australia: Abstracts of the 66th Annual Scientific Meeting of the Urological Society of Australia and New Zealand; 13-16 April 2013.
- Abughosh Z, Margolick J, Goldenberg SL, et al. A prospective randomized trial of povidone-iodine prophylactic cleansing of the rectum before transrectal ultrasound guided prostate biopsy. J Urol 2013;189:1326-31. [Crossref] [PubMed]
- Pu C, Bai Y, Yuan H, et al. Reducing the risk of infection for transrectal prostate biopsy with povidone-iodine: a systematic review and meta-analysis. Int Urol Nephrol 2014;46:1691-8. [Crossref] [PubMed]
- Issa MM, Al-Qassab UA, Hall J, et al. Formalin disinfection of biopsy needle minimizes the risk of sepsis following prostate biopsy. J Urol 2013;190:1769-75. [Crossref] [PubMed]
- Roberts MJ, Williamson DA, Hadway P, et al. Baseline prevalence of antimicrobial resistance and subsequent infection following prostate biopsy using empirical or altered prophylaxis: A bias-adjusted meta-analysis. Int J Antimicrob Agents. 2014;43:301-9. [Crossref] [PubMed]
- Roberts MJ, Bennett HY, Harris PN, et al. Prostate Biopsy Related Infection: a Systematic Review of Risk Factors, Prevention Strategies and Management Approaches. Urology 2017;104:11-21. [Crossref] [PubMed]
- Cussans A, Somani BK, Basarab A, Dudderidge TJ. The role of targeted prophylactic antimicrobial therapy before transrectal ultrasonography-guided prostate biopsy in reducing infection rates: a systematic review. BJU Int 2016;117:725-31. [Crossref] [PubMed]
- Egbers N, Schwenke C, Maxeiner A, et al. MRI-guided core needle biopsy of the prostate: acceptance and side effects. Diagn Interv Radiol 2015;21:215-21. [Crossref] [PubMed]
- Davis P, Paul E, Grummet J. Current practice of prostate biopsy in Australia and New Zealand: A survey. Urol Ann 2015;7:315-9. [PubMed]
- Murphy DG, Grummet JP. Planning for the post-antibiotic era - why we must avoid TRUS-guided biopsy sampling. Nat Rev Urol 2016;13:559-60. [Crossref] [PubMed]
- Grummet JP, Weerakoon M, Huang S, Lawrentschuk N, Frydenberg M, Moon DA, et al. Sepsis and 'superbugs': should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int 2014;114:384-8. [PubMed]
- Grummet J, Pepdjonovic L, Moon D. Re: Marco Borghesi, Hashim Ahmed, Robert Nam, et al. Complications After Systematic, Random, and Image-guided Prostate Biopsy. Eur Urol 2017;71:e143-e144. [Crossref] [PubMed]
- Pepdjonovic L, Tan GH, Huang S, et al. Zero hospital admissions for infection after 577 transperineal prostate biopsies using single-dose cephazolin prophylaxis. World J Urol 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Antibiotic: Transperineal prostatic biopsy: Therapeutic Guidelines; 2016 [cited 2016 October 3]. Available online: http://online.tg.org.au/ip/desktop/index.html
- Ho H, Yuen JS, Mohan P, et al. Robotic transperineal prostate biopsy: pilot clinical study. Urology 2011;78:1203-8. [Crossref] [PubMed]
- Radtke JP, Kuru TH, Boxler S, et al. Comparative analysis of transperineal template saturation prostate biopsy versus magnetic resonance imaging targeted biopsy with magnetic resonance imaging-ultrasound fusion guidance. J Urol 2015;193:87-94. [Crossref] [PubMed]
- Kuru TH, Wadhwa K, Chang RT, et al. Definitions of terms, processes and a minimum dataset for transperineal prostate biopsies: a standardization approach of the Ginsburg Study Group for Enhanced Prostate Diagnostics. BJU Int 2013;112:568-77. [Crossref] [PubMed]
- Radtke JP, Schwab C, Wolf MB, et al. Multiparametric Magnetic Resonance Imaging (MRI) and MRI-Transrectal Ultrasound Fusion Biopsy for Index Tumor Detection: Correlation with Radical Prostatectomy Specimen. Eur Urol 2016;70:846-53. [Crossref] [PubMed]
- Pepe P, Garufi A, Priolo G, et al. Transperineal Versus Transrectal MRI/TRUS Fusion Targeted Biopsy: Detection Rate of Clinically Significant Prostate Cancer. Clin Genitourin Cancer 2017;15:e33-6. [Crossref] [PubMed]
- Hansen N, Patruno G, Wadhwa K, et al. Magnetic Resonance and Ultrasound Image Fusion Supported Transperineal Prostate Biopsy Using the Ginsburg Protocol: Technique, Learning Points, and Biopsy Results. Eur Urol 2016;70:332-40. [Crossref] [PubMed]
- Wysock JS, Mendhiratta N, Zattoni F, et al. Predictive value of negative 3T multiparametric magnetic resonance imaging of the prostate on 12-core biopsy results. BJU Int 2016;118:515-20. [Crossref] [PubMed]
- Thompson JE, Moses D, Shnier R, et al. Multiparametric magnetic resonance imaging guided diagnostic biopsy detects significant prostate cancer and could reduce unnecessary biopsies and over detection: a prospective study. J Urol 2014;192:67-74. [Crossref] [PubMed]


