The efficacy of resiniferatoxin in prevention of catheter related bladder discomfort in patients after TURP - a pilot, randomized, open study
Introduction
Patients of benign prostatic hyperplasia undergoing transurethral resection of the prostate (TUR-P) often have urinary bladder catheterized. The catheter is frequently left in situ for the purpose of postoperative bladder drainage. As results of catheterization and lesions in proximal part of the urethra or bladder after TUR-P, patients often complain of bladder discomfort (an urge to void or discomfort in the suprapubic region) due to irritation from the catheterization over postoperative period. Severe symptoms of catheter related bladder discomfort (CRBD) are suprapubic pain and problems with outflow from the urethral catheter, conditions so-called bladder spasm. It is a result of lesions in the proximal part of the urethra or bladder due to the presence of indwelling urethral catheter (1). These symptoms are similar to symptoms of overactive bladder (OAB) (2). Muscarinic receptor antagonists oxybutynin and tolterodine which have been used successfully in the management of overactive bladder were also reported to be able to reduce catheter related bladder discomfort (3-7). According to the previous reports, these antagonists can reduce the incidence and severity of bladder discomfort in about half of the patients. However, the adverse events of muscarinic receptor antagonists (such as dry mouth, constipation, dysuria, and dyspepsia) have prevented them from being used as a routine management for CRBD (8-11). A number of investigators have tried other intervention methods, such as using intravesical diamorphine, oral opioids, or i.v. ketamine, to prevent CRBD (5,12). All of them reduce the incidence and severity of CRBD to some degree. However, the anaethetic nature of these drugs rendered them being less popular.
As a potent capsaicin analogue, resiniferatoxin (RTX) has the capacity to excite and then to desensitize type C primary afferent fibers, which in turn leads to desensitization of bladder (13-16). RTX has been shown to have variable efficacy in the treatment of intractable lower urinary tract symptoms (LUTS) and symptoms associated with neurogenic detrusor overactivity (17,18). It has also been used successfully in treating OAB (14-19). However, RTX's efficacy on CRBD remains unknown. In order to evaluate the potential and efficiency of RTX in treatment of CRBD over post-operative period of TURP, we conducted the current pilot, randomized open study.
Methods
Patients and treatment
Approval was received from the Institute's ethics committee and written informed consent was obtained from all the patients. The study was designed to be a pilot, randomized, open investigation. The study consisted of 48 consecutive patients who had undergone standard monopolar TURP at our institute from September 2007 to September 2008. Patients' prostate volume was measured by transrectal ultrasound (TRUS). Patients were also identified as bladder outlet obstruction according to results of urodynamics. Eligible patients were randomly divided. Twenty-four patients in RTX group (Group I) received, intravesically, 40 mL of 20 nM RTX (Hainan Newway Pharmaceutical Co., LTD, P.R. China) 20 hours before operation. Patients were asked to hold the drug for 30 minutes. Before introducing RTX, patients received intravesical instillation of 20 mL 2% lidocaine solution and 10 mL 0.75% bupivacaine solution, in order to prevent the temporary pain of bladder and urethra (20). Twenty-four patients in control Group (Group II) received no treatment before operation. After TUR-P, patients were indwelled with a three-way 22 Fr Foley catheter with 50 mL balloon, which was discharged 5 days after operation. All patients' age, prostates volume, IPSS (International Prostate Symptom Score), Storage Score in IPSS, Void Score in IPSS, and quality of life (QOL) score were collected. In Group I, the average age was 72+8.33 years (range from 56 to 88 years), the average prostates volume 64+19.06 mL (range from 32 to 92 mL), the average international prostate symptom score (IPSS) 22.7+3.16 (range from 16 to 28), the average Storage Score in IPSS 13.1+2.66 (range from 8 to 17), the average Void Score in IPSS 9.6+1.88 (range from 5 to 13), the average QOL score 4.2+0.88 (range from 2 to 6). In Group II, the average age was 69+6.93 years (range from 54 to 86 years), prostates volume 69+17.46 mL (range from 34 to 97 mL), IPSS 23.5+3.57 (range from 16 to 31), Storage Score in IPSS 12.6+2.66 (range from 8 to 17), Void Score in IPSS 10.7+2.21 (range from 6 to 14) QOL score 4.4+1.06 (range from 2 to 6).
Assessment of CRBD
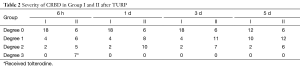
Catheter related bladder discomfort (CRBD) was assessed by the investigators at 6 hours, 1, 3 and 5 days after TURP. Severity of bladder discomfort was recorded as degree 0 (did not complain of any bladder discomfort), degree 1 (mild, reported by the patient only on questioning and does not need treatment), degree 2 (moderate, reported by the patient on their own, such as an urge to pass urine or discomfort in the suprapubic region, and does not need treatment), and degree 3 (severe, bladder spasm, reported by the patient without questioning, accompanied by behavioral responses) (4,5). All patients of degree 3 received tolterodine.
Statistics
The Independent samples t test and Fisher's exact test were used for statistical analyses of the different age, prostates volume, IPSS score and severity of CRBD between the Group I and Group II. SPSS 16.0 software was used to perform all statistical computations.
Results
General information of patients
There was no statistical difference between Group I and Group II in patients' age, prostates volume, IPSS score, Storage Score in IPSS, Void Score in IPSS, and QOL, P values were 0.213, 0.356, 0.471, 0.554, 0.055, and 0.380, respectively.
Effect of RTX on CRBD
During the first three days of post-operative period, the incidence of patients' CRBD was lower in Group I than that in Group II (25% vs. 75%, P=0.001, Fisher's exact test). On the fifth day after surgery, although the incidence of CRBD was still lower in Group I than that in Group II (50% vs. 75%), there was no significant difference between them (P=0.135, Fisher's exact test). The incidence and severity of patients' CRBD was detailed in Tables 1 and 2.

Full table
Full table
No patient in Group-1 required muscarinic receptor antagonist (tolterodine). However, seven patients with degree 3 CRBD in Group-II received tolterodine during the first day after operation. Degree 3 symptoms in all these patients in Group II were controlled, and the degree of CRBD in these patients were reduced to lower grade after the treatment in days to follow. The number of patients who received tolterodine was statistically different between the two groups, P=0.009. Table 2 summarizes the details of severity of patients' CRBD in Group I and II.
The intravesical instillation RTX caused temporal pain of bladder and urethra which were relieved without treatment. No other obvious adverse events were otherwise observed.
Discussion
Generally, the incidence of CRBD caused by catheter related bladder irritation during the postoperative period was about 55% (4,5). The incidence was much higher in patients after TUR-P (1). CRBD, especially bladder spasm not only results in severe suffering of the patients but also increase the chance of post-operative bleeding, clot forming, and may lead to a re-operation after TUR-P. Muscarinic receptor antagonists and anesthesia agents, such as oxybutynin, tolterodine, and ketamine have been used successfully for the management of CRBD (6,9-12). However, adverse event of these drugs, such as dry mouth, constipation, dyspepsia, dysuria, and urinary retention limited the use of these drugs post TUR-P (8-11). The post-TURP condition is therefore requires more efficient and safer management.
In a reflex response, afferent input determines efferent output. Any approach which blocks the conduction of afferent nerve fibers may also be used to control CRBD. As a C fiber neurotoxin, resiniferatoxin (RTX) is an extract from the latex of Euphorbia resinifera. It is an ultrapotent capsaicin analog, and has a significant advantage of being less irritable. It binds to transient receptor potential vanilloid 1 (TRPV1), previously known as vanilloid receptor type 1 (VR1) (13,14,21). It has the capacity to excite and then to desensitize type C primary afferent fibers. Following the TRPV1 opening, the excitation leads to spike-like calcium currents. The transient high levels of intracellular calcium and other ions cause neuropeptide release (such as substance P) (22,23). The temporary bladder pain patients experienced during RTX treatment is known to be the result of detrusor contractions. In C afferent fibers, activation of bioelectricity will eventually stop and thus block bladder sensory transmission. The desensitization mechanisms by resiniferatoxin include: decreases in sensory input conveyed in bladder C-fibers, and decreases in the number of spinal neurons that become excited by bladder stimuli (24). There have been reported that RTX can be used to treat detrusor instability, BPH associated storage lower urinary tract symptoms, and overactive bladder (25). Thus, we hypothesized that intravesical administration of RTX may reduce the incidence and severity of CRBD after TUR-P.
According the results of our study, the pre-operative administration of RTX intravesically could reduce both incidence and severity of CRBD during the first 3 days of post-operative period. The need for using antimuscarinic drugs was also reduced. In Group I, no patients had CRBD of degree 3. RTX was effective for detrusor instability, detrusor hyperreflexia, and alleviating bladder pain. In the US, most patients have indwelling catheter only 1-2 days after TURP. However, it may be companied severe lower urinary tract syndrome (LUTS). So, most patients usually indwelling catheter 3-5 days in China. Our result suggested that patients of RTX Group may not need catheter for 5 days either. However, patients will experience phasic detrusor contractions shortly after the intravesical instillation RTX. The detrusor contractions result in the patients having urge sensation to urinate. In addition, patients felt itching or warm in the lower abdomen during the initial period of RTX administration (26,27). All of these temporary discomforts can be prevented by intravesical administration lidocaine and bupivacaine solution. There was no patient suffering from severe adverse events in our study. In addition, in order to avoid intravesical instillation RTX related bladder discomfort overlapping with CRBD post-operation, we instilled RTX 20 hours before operation. Compared with instilling RTX half an hour before operation after patient received spinal anesthesia which we used in our preliminary study, the new procedure has the advantage of minimum waiting time prior and during anaesthesia, thus allowing less time to be spent in the operating theatre. On the other hand, the temporary discomfort related to RTX will have disappeared before the start of the operation. The 20-hour pre-operative period is therefore long enough for the temporary discomfort by RTX to diminish.
The lowest dose to decrease bladder sensitivity and bladder pain was 10 nM. With an increase in dosage, significant improvement in symptoms and prolonged duration of improvement were obtained. In our study, with a dosage of RTX 20 nM, we achieved a significant reduction of incidence and severity of CRBD. The maximum effect was noted during the first three post-operative days. On the fifth day post-operative, the advantage of Group I over that of Group II no longer exists. Probably, with the recovery from lesions in proximal part of the urethra or bladder, the longer duration after TUR-P the more tolerable of patients become to indwelling urethral catheter. In additional, a portion of the patients in Group II had used tolterodine which would also reduce the incidence and severity of CRBD. Finally, we view that the dosage of RTX used in the present study was relatively low. A higher and safe dosage of RTX may reduce incidence and severity of CRBD more significantly and last longer time. On the other hand, it is proposed that intravesical instillation of RTX again on the third day after operation may be more effective for CRBD, and may be a useful adjunct for lower urinary tract symptoms post TUR-P. Clearly, more studies are necessary in testing different dosages and repeated intravesical instillation RTX.
Conclusions
In our pilot randomized open study, a single intravesical administration of 40 mL of 20 nM RTX before TUR-P reduced both incidence and severity of post-operative CRBD via desensitization of bladder. The procedure has no contraindication and does not have other adverse event caused by RTX. The temporary pain of bladder and urethra can be prevented by analgesia with intravesical instillation of lidocaine and bupivacaine solution. Therefore, the procedure can be considered as a safe pretreatment option for decreasing CRBD in patients after TUR-P. Whether using a higher dose of RTX or repeated intravesical instillation RTX may reduce incidence and severity of CRBD more significantly require further investigation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Yates V, Tanner J, Crossley A. Bladder spasm following transurethral surgery. Br J Perioper Nurs 2004;14:259-60,262. [PubMed]
- Freeman R, Hill S, Millard R, et al. Reduced perception of urgency in treatment of overactive bladder with extended-release tolterodine. Obstet Gynecol 2003;102:605-11. [PubMed]
- Chapple CR, Van Kerrebroeck PE, Jünemann KP, et al. Comparison of fesoterodine and tolterodine in patients with overactive bladder. BJU Int 2008;102:1128-32. [PubMed]
- Agarwal A, Raza M, Singhal V, et al. The efficacy of tolterodine for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Anesth Analg 2005;101:1065-7. table of contents. [PubMed]
- Agarwal A, Gupta D, Kumar M, et al. Ketamine for treatment of catheter related bladder discomfort: a prospective, randomized, placebo controlled and double blind study. Br J Anaesth 2006;96:587-9. [PubMed]
- Agarwal A, Dhiraaj S, Singhal V, et al. Comparison of efficacy of oxybutynin and tolterodine for prevention of catheter related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Br J Anaesth 2006;96:377-80. [PubMed]
- Moodie P. PHARMAC responds on tolterodine for overactive bladder. N Z Med J 2006;119:U1871. [PubMed]
- Garely AD, Burrows L. Benefit-risk assessment of tolterodine in the treatment of overactive bladder in adults. Drug Saf 2004;27:1043-57. [PubMed]
- Andersson KE, Chapple CR. Oxybutynin and the overactive bladder. World J Urol 2001;19:319-23. [PubMed]
- Appell RA, Sand P, Dmochowski R, et al. Prospective randomized controlled trial of extended-release oxybutynin chloride and tolterodine tartrate in the treatment of overactive bladder: results of the OBJECT Study. Mayo Clin Proc 2001;76:358-63. [PubMed]
- Appell RA, Abrams P, Drutz HP, et al. Treatment of overactive bladder: long-term tolerability and efficacy of tolterodine. World J Urol 2001;19:141-7. [PubMed]
- McCoubrie R, Jeffrey D. Intravesical diamorphine for bladder spasm. J Pain Symptom Manage 2003;25:1-3. [PubMed]
- Marshall IC, Owen DE, Cripps TV, et al. Activation of vanilloid receptor 1 by resiniferatoxin mobilizes calcium from inositol 1,4,5-trisphosphate-sensitive stores. Br J Pharmacol 2003;138:172-6. [PubMed]
- Apostolidis A, Gonzales GE, Fowler CJ. Effect of intravesical Resiniferatoxin (RTX) on lower urinary tract symptoms, urodynamic parameters, and quality of life of patients with urodynamic increased bladder sensation. Eur Urol 2006;50:1299-305. [PubMed]
- Cruz CD, Charrua A, Vieira E, et al. Intrathecal delivery of resiniferatoxin (RTX) reduces detrusor overactivity and spinal expression of TRPV1 in spinal cord injured animals. Exp Neurol 2008;214:301-8. [PubMed]
- Apostolidis A, Brady CM, Yiangou Y, et al. Capsaicin receptor TRPV1 in urothelium of neurogenic human bladders and effect of intravesical resiniferatoxin. Urology 2005;65:400-5. [PubMed]
- Dinis P, Charrua A, Avelino A, et al. Intravesical resiniferatoxin decreases spinal c-fos expression and increases bladder volume to reflex micturition in rats with chronic inflamed urinary bladders. BJU Int 2004;94:153-7. [PubMed]
- de Sèze M, Wiart L, de Seze MP, et al. Intravesical capsaicin versus resiniferatoxin for the treatment of detrusor hyperreflexia in spinal cord injured patients: a double-blind, randomized, controlled study. J Urol 2004;171:251-5. [PubMed]
- Andersson KE. New pharmacologic targets for the treatment of the overactive bladder: an update. Urology 2004;63:32-41. [PubMed]
- Silva C, Ribeiro MJ, Cruz F. The effect of intravesical resiniferatoxin in patients with idiopathic detrusor instability suggests that involuntary detrusor contractions are triggered by C-fiber input. J Urol 2002;168:575-9. [PubMed]
- Dinis P, Silva J, Ribeiro MJ, et al. Bladder C-fiber desensitization induces a long-lasting improvement of BPH-associated storage LUTS: a pilot study. Eur Urol 2004;46:88-93. [PubMed]
- Lazzeri M, Beneforti P, Spinelli M, et al. Intravesical resiniferatoxin for the treatment of hypersensitive disorder: a randomized placebo controlled study. J Urol 2000;164:676-9. [PubMed]
- Xu XJ, Farkas-Szallasi T, Lundberg JM, et al. Effects of the capsaicin analogue resiniferatoxin on spinal nociceptive mechanisms in the rat: behavioral, electrophysiological and in situ hybridization studies. Brain Res 1997;752:52-60. [PubMed]
- Seki N, Ikawa S, Takano N, et al. Intravesical instillation of resiniferatoxin for neurogenic bladder dysfunction in a patient with myelodysplasia. J Urol 2001;166:2368-9. [PubMed]
- Fowler CJ. Intravesical treatment of overactive bladder. Urology 2000;55:60-4. [PubMed]
- Silva C, Rio ME, Cruz F. Desensitization of bladder sensory fibers by intravesical resiniferatoxin, a capsaicin analog: long-term results for the treatment of detrusor hyperreflexia. Eur Urol 2000;38:444-52. [PubMed]
- Kuo HC. Effectiveness of intravesical resiniferatoxin for anticholinergic treatment refractory detrusor overactivity due to nonspinal cord lesions. J Urol 2003;170:835-9. [PubMed]


