Commentary on the myths of Peyronie’s disease
Peyronie’s disease refers to an acquired curvature, narrowing or shortening of the penis. Prevalence rates of 0.4-20% have been published (1). Development of Peyronie’s disease is likely related to minor injury to the tunica albuginea, septum or intracavernous struts. In some men, the resulting inflammation is trapped between layers of the collagen bundles and becomes progressive. This leads to an inflammatory mass (lump) formation in the early stage. Continuing inflammation produces profibrotic cytokines such as transforming growth factor beta and deposition of large amount of collagen fibers. The inflammation can also produce metalloproteinases that break the elastic fibers. The irregularly compacted collagen fibers and disrupted elastic fibers create an inelastic “plaque,” the “incurable” component of Peyronie’s disease. The loss of elasticity produces curvature, shortening, narrowing, distal flaccidity and erectile dysfunction depending on the location of the fibrotic process (2). In this article, we discuss the variable clinical presentation of and management of Peyronie’s disease, illustrated by three cases. Up to now, Peyronie’s disease has been considered an “incurable” disease because there is no medical treatment that can return the penis to its premorbid state. Nevertheless, we would like to revisit the anatomy of the disease, and propose a treatment to arrest the disease in its early stages. In more advanced stages, we recommend a combination of medication and physical force to restore penile anatomy, improve erectile function, and, thus, reduce the psychological devastation affecting the patient (3).
Case 1
A 60 year-old man presented to the Urology clinic with a complaint of three months of sudden onset painless penile deformity with curvature upwards and to the right. He denies any known history of trauma. He notes that he has 100% rigid erections, but is only able to penetrate 75% of the time due to his penile deformity (Comment 1). His past medical history includes depression, anxiety, herpes, and asthma. His surgical history includes orthopedic procedures to his right femur, and an appendectomy. He states that he is not in a stable relationship currently. He does not smoke or use any recreational drugs, and he drinks with moderation.
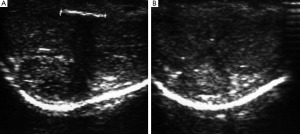
On physical examination, he had an uncircumcised phallus, and a normal meatus. His testicles were bilaterally descended, and normal in size. A dorsal firm plaque could be palpated, about 2 cm in length. Further evaluation with penile ultrasound (GE logiq P5 device, 12 MHz) revealed a dorsal, midline plaque measuring 2 cm × 1.5 cm with associated calcification measuring 1.3 cm × 0.9 cm (Comment 2). During examination, his penis was partially erect, and a 30 degree dorsal and rightward curvature was noted.
The patient was placed on pentoxifylline 400 mg PO TID. He did have some dyspepsia in response to this dose, and he was thus reduced to 400 mg PO BID. He continued on this dose for 8 months. Upon follow up, he noted improved curvature, from 30 degrees to 10 degrees. A dorsal plaque could still be palpated. Upon ultrasound evaluation of the penis, dorsal fibrosis was still evident, but the calcification had completely resolved (Figure 1).
Case 2
This is a 51 year-old man who presented with penile deformity and shortening. He recalled a minor penile injury during sexual intercourse about 1 year ago. There was no ecchymosis or urethral bleeding at that time (comment 3). The pain subsided after a few hours. Shortly after, he noted a lump in the middle of his penis. Subsequently over the next several months, he developed progressive dorsal penile curvature and penile shortening with erections. Erections were also painful. Upon consultation with his local Urologist, he was told that he had Peyronie’s disease and that this would resolve spontaneously. He was told to return in one year if the curvature persisted (Comment 4). However, the progressive shortening made sexual intercourse difficult and greatly affected his confidence, leading to cessation of intercourse with his female partner. About one year after his initial injury, he presented to our clinic, quite distressed about this issue, as is often seen in patients with Peyronie’s disease (3). He noted that he had lost about 2 inches (5 cm) of length in the past year, and he provided a photograph confirming a 60 degree dorsal curvature. He was otherwise healthy and had not had any past surgeries.
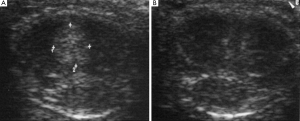
On physical exam, he had an extensive palpable plaque along the dorsum of his penis. His testicles were normal in size, and were descended bilaterally. Penile ultrasound revealed a small ventral plaque and an extensive dorsal plaque with large calcification (Figure 2).

The patient underwent tunica-sparing excision of the ossified plaque (4), and a 16-dot plication (5) to correct the penile curvature. Post-operatively, he was given pentoxifylline. Six weeks post-operatively, he was instructed to perform penile stretching with a vacuum device. Five months later, his painful erections and his erectile dysfunction resolved (comment 5). He was able to gain 1 inch (2.5 cm) in penile length after 6 months of stretching. At one year of follow up, the patient noted that while his erections were not as strong as before Peyronie’s disease, he was able to have painless, regular, sexual intercourse without the need for phosphodiesterase 5 inhibitors, and his mood had significantly improved.
Case 3
A 55-year-old man presented with 18 months of progressive penile deformity and erectile dysfunction (ED). The patient did not recall history of penile injury. At the present, the penis curved upwards and to the left with erections. However, the patient also noted distal penile flaccidity, refractory to maximal dosages of phosphodiesterase 5 inhibitors. He was otherwise healthy and had not had any past surgeries.
Physical examination revealed extensive dorsal plaque and penile fibrosis, more severe on the left side. Penile ultrasound showed two dorsal plaques and distal intracavernous diffuse coarse echogenic spots consistent with fibrosis of the intracavernous struts (comment 6, Figure 3). An intracavernous injection test confirmed 45 degree dorsal, 30 degree left lateral curvature and distal flaccidity about 3 cm long (comment 7).

After extensive consultation regarding various medical and surgical options, the patient elected to under to implantation of an inflatable penile prosthesis. The penis became straight without the need for graft or plication sutures after dilation and implantation of the prosthesis (comment 8). He had an uneventful recovery and was able to resume sexual intercourse with a straight penis 5 weeks after surgery.
Case comments
I. Although the patient only began to notice penile deformity three months prior to presentation, it is likely that the process of inflammation and fibrosis began long before, given the finding of calcification.
II. In our experience, calcification occurs in about 31% of patients (6). If the calcification is less than 1.5 cm, 400-800 mg pentoxifylline tid has a more than 90% chance arresting or eliminating the calcification (7). Larger ones do not respond to pentoxifylline and surgical excision may be needed if the patient has persistent pain, severe shortening or curvature.
III. Ecchymosis occurs when blood escapes from the corpora cavernosa to the subcutaneous space through ruptured lateral or ventral tunica albuginea while urethral bleeding occurs if the tunica ruptures to the urethra. Since the dorsal tunica is much thicker, rupture rarely occurs. Instead, this type of injury often disrupts the junction between the septum and dorsal tunica, or septum itself, resulting in a dorsal plaque or septal fibrosis. No ecchymosis or urethral bleeding occured because the tunica albuginea was intact.
IV. Spontaneous resolution of Peyronie’s disease occurs in less than 13% (8). Since no single “effective” medical treatment has been proven, patients are usually told to wait for a year and see if the disease resolves by itself. Unfortunately, for many patients, waiting results in more advanced disease, which has less response to medical therapy.
V. Surgical options for patients with large calcification/ossification include plication only, plaque excision with grafting, or subtunical ossified plaque excision and plication. Owing to the high incidence of ED after large plaque excision and grafting (9) as well as the patient’s severe depression, we elected to perform subtunical ossified plaque excision and plication (4). Since neither neurovascular dissection nor grafting is needed, the chance of penile numbness and ED is reduced. For patients with penile shortening or narrowing, we recommend a combination of pentoxifylline and penile stretching with a vacuum device daily for 6 months, similar to regimens advised by Levine’s group (10,11).
VI. The intracavernous fibrosis is most likely a result of thickening/fibrosis of the intracavernous struts because there is no reason for smooth muscle atrophy with intracavernous fibrosis in this case. Another typical finding is a smaller diameter of the corpus cavernosum from fibrosis of the struts.
VII. The senior author has good results in correcting hour glass deformities or localized indentations of less than 1 cm with grafts placed on the lateral aspect of the penis. However, most patients develop ED after placement of grafts to correct distal flaccidity of longer length. The authors suspect that the failure is likely due to the inability of tunica graft to correct the contracted intracavernous struts.
VIII. Most implant surgeons have observed the decrease in the curvature of the penis after corporal dilation and placement of penile prosthesis. Since, the length of the contracted tunica albuginea was not altered, the only explanation is the disruption of the contracted struts or disconnection of the struts from the tunica albuginea. This would then allow the inflatable penile prosthesis to inflate and lengthen/widen the corpora cavernosa.
Expert opinion
The non-surgical management of Peyronie’s disease has significantly advanced, but despite multiple randomized trials and uncontrolled case series, one treatment alone has not been found to be definitively superior. Proposed oral therapy has included pentoxifylline, colchicine, and potassium para-aminobenzoate (12-14). In cases where the Peyronie’s lesion is readily accessible, intralesional administration of Verapamil, Interferon, and Collagenase have all been tried with some success (15-17). In uncontrolled studies, traction devices and vacuum devices have been shown to result in some benefit to curvature (18,19).
The mechanisms of Peyronie’s plaque formation have not been fully defined, but likely begins with an inflammatory process, possibly from trauma, which then leads to fibrosis, decreased elasticity and excess collagen deposition (20,21). Oral therapies, such as pentoxifylline may act on inflammation and early fibrosis. Indeed, pentoxifylline has been shown to inhibit fibrosis induced by Transforming Growth Factor (TGF) Beta-1 (22).
Intralesional therapies, such as interferon alpha-2b, may also limit inflammation and early fibrosis by decreasing fibroblast proliferation, extracellular matrix production, and collagen production from fibroblasts (17). Clostridial collagenase is a purified bacterial enzyme that selectively breaks up collagen, and thus may help further with late fibrotic scars, rich in collagen (16,23).
However, when working with intralesional therapies, it is important to be able to target the lesion. Thus, while plaques on the dorsum of the penis are readily accessible, patients with ventral plaques, intracorporal or septal fibrosis (Figure 4) and large calcifications may be less treatable with this method. Indeed, in a review of 891 men receiving penile ultrasonography for Peyronie’s disease, Chung et al. found that 43% of patients had septal fibrosis (24).
The “incurable” component of the Peyronie’s disease is the late dense fibrosis and “loss of elasticity” that is refractory to medical treatments including the most powerful therapy, the intralesional injection of collagenase. Dissolving or softening the plaque alone does not straighten the penis fully, as evidenced by recent clinical trials (8,23). The best results are in patients who have had a “modeling” procedure where the physician forcefully stretches the softened plaque after several injections of collagenase. Penile traction and vacuum erection devices help address the issue of loss in elasticity. These therapies will mechanically stretch the tunica to help straighten the penis. Levine’s group has shown previously that therapy combining oral or intralesional therapy with penile traction provides both length and reduction in curvature (10).
Given the multiple components of Peyronie’s disease (inflammation, fibrosis, and loss of elasticity), we typically recommend combination therapy for patients with moderate-to-severe curvatures or shortening, utilizing pentoxifylline and a vacuum device (Table 1). With vacuum therapy alone, inflammation from trauma would continue, and fibrosis would likely recur. In the case of more severe curvatures, pentoxifylline alone is unlikely to overcome the overall loss in elasticity, and thus minimal benefit will be seen with regards to straightening.
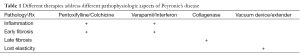
Full table
Decisions to pursue surgery should be patient centered. Indications to pursue surgical intervention include disease refractory to medical therapy alone, moderate-to-severe curvature. Curvature alone may typically be managed successfully with plication alone (25). Patients with hour-glass deformities or large areas of calcification may benefit from tunical excision and grafting, but these patients must be counseled on the high risk of subsequent ED. Alternatively, a subtunical excision of ossified portion of plaque and plication may achieve the same goal with minimal risk of penile numbness and ED (4).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Dibenedetti DB, Nguyen D, Zografos L, et al. A Population-Based Study of Peyronie’s Disease: Prevalence and Treatment Patterns in the United States. Adv Urol 2011;2011:282503.
- Lue TF. Peyronie’s disease: an anatomically-based hypothesis and beyond. Int J Impot Res 2002;14:411-3. [PubMed]
- Nelson CJ, Mulhall JP. Psychological impact of Peyronie's disease: a review. J Sex Med 2013;10:653-60. [PubMed]
- Eisenberg ML, Smith JF, Shindel AW, et al. Tunica-sparing ossified Peyronie’s plaque excision. BJU Int 2011;107:622-5. [PubMed]
- Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002;167:2066-9. [PubMed]
- Smith JF, Brant WO, Fradet V, et al. Penile sonographic and clinical characteristics in men with Peyronie’s disease. J Sex Med 2009;6:2858-67. [PubMed]
- Smith JF, Shindel AW, Huang YC, et al. Pentoxifylline treatment and penile calcifications in men with Peyronie’s disease. Asian J Androl 2011;13:322-5. [PubMed]
- Hatzimouratidis K, Eardley I, Giuliano F, et al. EAU guidelines on penile curvature. Eur Urol 2012;62:543-52. [PubMed]
- Flores S, Choi J, Alex B, et al. Erectile dysfunction after plaque incision and grafting: short-term assessment of incidence and predictors. J Sex Med 2011;8:2031-7. [PubMed]
- Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie’s disease. J Sex Med 2012;9:288-95. [PubMed]
- Rybak J, Papagiannopoulos D, Levine L. A retrospective comparative study of traction therapy vs. no traction following tunica albuginea plication or partial excision and grafting for Peyronie’s disease: measured lengths and patient perceptions. J Sex Med 2012;9:2396-403. [PubMed]
- Brant WO, Dean RC, Lue TF. Treatment of Peyronie's disease with oral pentoxifylline. Nat Clin Pract Urol 2006;3:111-5. [PubMed]
- Weidner W, Hauck EW, Schnitker J. Potassium paraaminobenzoate (POTABA) in the treatment of Peyronie’s disease: a prospective, placebo-controlled, randomized study. Eur Urol 2005;47:530-5. [PubMed]
- Kadioglu A, Tefekli A, Köksal T, et al. Treatment of Peyronie’s disease with oral colchicine: long-term results and predictive parameters of successful outcome. Int J Impot Res 2000;12:169-75. [PubMed]
- Shirazi M, Haghpanah AR, Badiee M, et al. Effect of intralesional verapamil for treatment of Peyronie’s disease: a randomized single-blind, placebo-controlled study. Int Urol Nephrol 2009;41:467-71. [PubMed]
- Gelbard MK, James K, Riach P, et al. Collagenase versus placebo in the treatment of Peyronie’s disease: a double-blind study. J Urol 1993;149:56-8. [PubMed]
- Hellstrom WJ, Kendirci M, Matern R, et al. Single-blind, multicenter, placebo controlled, parallel study to assess the safety and efficacy of intralesional interferon alpha-2B for minimally invasive treatment for Peyronie’s disease. J Urol 2006;176:394-8. [PubMed]
- Levine LA, Newell M, Taylor FL. Penile traction therapy for treatment of Peyronie’s disease: a single-center pilot study. J Sex Med 2008;5:1468-73. [PubMed]
- Raheem AA, Garaffa G, Raheem TA, et al. The role of vacuum pump therapy to mechanically straighten the penis in Peyronie’s disease. BJU Int 2010;106:1178-80. [PubMed]
- Brock G, Hsu GL, Nunes L, et al. The anatomy of the tunica albuginea in the normal penis and Peyronie’s disease. J Urol 1997;157:276-81. [PubMed]
- El-Sakka AI, Hassoba HM, Pillarisetty RJ, et al. Peyronie’s disease is associated with an increase in transforming growth factor-beta protein expression. J Urol 1997;158:1391-4. [PubMed]
- Valente EG, Vernet D, Ferrini MG, et al. L-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie’s fibrotic plaque and related fibroblast cultures. Nitric Oxide 2003;9:229-44. [PubMed]
- Jordan GH. The use of intralesional clostridial collagenase injection therapy for Peyronie’s disease: a prospective, single-center, non-placebo-controlled study. J Sex Med 2008;5:180-7. [PubMed]
- Chung E, Yan H, De Young L, et al. Penile Doppler sonographic and clinical characteristics in Peyronie’s disease and/or erectile dysfunction: an analysis of 1500 men with male sexual dysfunction. BJU Int 2012;110:1201-5. [PubMed]
- Hudak SJ, Morey AF, Adibi M, et al. Favorable patient reported outcomes after penile plication for wide array of peyronie disease abnormalities. J Urol 2013;189:1019-24. [PubMed]


