Urethral catheters and medical malpractice: a legal database review from 1965 to 2015
Introduction
Medical malpractice lawsuits have increased in United States (US) over the last 150 years (1). Prior to 1840, medical malpractice suits were mainly limited to cases that result in severe injury and death (1,2). The increase in medical malpractice claims has prompted physicians to practice “defensive medicine” which is defined as the deviation from standard medical practices induced by fear from liability (3). This may affect the quality of patient care and promote overuse of health services (4).
Urethral catheters (UCs) are one of the most commonly used medical devices since their invention in the 1930s (5). It is estimated that 25% of hospital inpatients have UCs inserted during their hospital stay (6). Despite widespread usage of UCs, providers are unaware of UC placement in 28% of their patients (7). Furthermore, UCs may be inserted for inappropriate reasons such as monitoring urine output in non-critical patients (7-10). UC complications, including catheter associated urinary tract infections (CAUTIs), non-infectious catheter related complications, and device malfunction are common (11-13). Given the prevalence of UC usage and related complications, healthcare providers are vulnerable to medical liability. Our objective is to characterize UC-related litigation over the past 50 years using a robust legal database.
Methods
Medical legal cases processed at the state and federal courts are routinely archived in LexisNexis—one of the largest legal databases in the US. The database maintains law reviews from more than 800 journals, US Supreme Court decisions, US Circuit Courts of Appeals decisions, and US District Courts decisions for all 50 US states and territories (14).
LexisNexis was queried for medical malpractice claims surrounding the placement, management, or removal of UCs. The search was limited to all state and federal cases from January 1965 through October 2015. The following search terms were utilized to build our query: “urethral catheter” or “Foley catheter” in combination with “medical malpractice”, “negligence”, “medical error”, and “trauma”. We included legal cases whereby the UC was primarily implicated as the main cause of harm reported by the plaintiff. We excluded cases in which a UC was merely mentioned in the claim however it was not central to the plaintiff’s claim.
Using our selected search terms, we reviewed legal cases for: date of trial, state location, plaintiff(s)’ gender, plaintiff(s)’ and defendant(s)’ identity, the identity of medical personnel inserting the UC, alleged causes of medical malpractice, damages claimed by plaintiffs, trial outcomes including the indemnity amount awarded by the jury and out of court settlement amounts. Case details were extracted through a review of court proceedings by two independent urologists (MAA and ECO). Statistical analysis was performed with STATA v14 (College Station, TX, USA). Descriptive statistics were primarily utilized.
Results
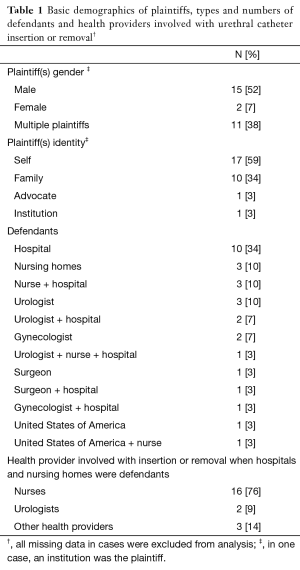
Of state and federal cases in LexisNexis database, 324 medical legal cases were found using the defined search terms. Of these, 29 cases met the inclusion criteria whereby UC usage was central to the plaintiff’s claim. Court proceedings took place in 18 different states within the US. Demographics of plaintiffs, defendants and healthcare providers involved with UC insertion or removal are summarized in Table 1. Overall, when individuals were named, the plaintiffs were most commonly males (52%). Hospitals alone or in combination with healthcare providers were most often named in UC-related litigation (18/29, 62%). Of the healthcare providers implicated, urologists (6/16, 38%) were the most common provider involved. Urologists were successful in defending all of their cases, and hospitals were involved with them as defendants in half of the time. When hospitals or nursing homes were involved either alone or with different healthcare providers, nurses were most often the providers involved with placing or removing the catheter (16/21, 76%). No nurses were cited as defendants solely.
Full table
The characteristics of each case are presented in Table 2. In these cases, the UC was primarily inserted for monitoring of urine output, or treatment of urinary retention, followed by routine post-operative care. The most common claim for a breach in medical practice was a traumatic insertion, followed by UC removal related errors. Pain was the most common complaint claimed by plaintiffs, followed by urinary tract infection (UTI) and fistula. Plaintiffs claimed death from urosepsis in cases. Six cases involved a second plaintiff. Each second plaintiff was a spouse and all claimed loss of consortium (deprivation of the benefits of a family relationship due to injuries caused by a tortfeasor). A verdict favoring the defendant was achieved in (19/29, 66%) cases, while (8/29, 28%) cases delivered an indemnity award for the plaintiffs, all of which involved institutions solely as defendants without any health care providers. Two (2/29, 7%) cases were settled out of court. The mean indemnity award paid to plaintiffs was $112,991 (median $35,100, range $4,000–$325,000). The mean settlement received by plaintiffs was $55,750 (median $55,750, range $25,000–$86,500). A detailed summary of cases included are presented in Table 3.

Full table

Full table
Discussion
In this study we reviewed medical malpractice cases that have been filed from 1965 through 2015 at the state and federal level in the US. Defendants named in these cases ranged from institutions, such as hospitals and nursing homes, as well as individuals, particularly urologists and nurses. Among individuals, urologists were most commonly implicated, however urologists were always successful in defending their cases in UC-related lawsuits. Overall, hospitals were most likely to be named in UC-related lawsuits.
Among inpatients, UCs are among the most commonly used medical devices with 25% of inpatients requiring a catheter during their hospitalization (6). With 36.5 million hospital stays in the US per year, there are over 9 million UCs placed annually (15). Given the yearly volume of UC placement, the potential for UC-related complications arise (16). As such, there is a concern that malpractice cases pertaining to UC-related complications may contribute to the burden of lawsuits faced by many healthcare providers.
Medical malpractice lawsuits are a concern and burden for all health care providers. A recent comprehensive review on urology malpractice studies as well as analysis of claims data from companies of the Physicians Insurers Association of America (PIAA) have shown that it is common for urologists to face malpractice litigation at some point in their career. However, as in our study, only a minority lose their cases (17). When faced with malpractice, urologists reported spending an average of 21.8 days away from work defending their first lawsuit. This results in reduced access to care for patients seeking urologic care (18). Previous studies suggest that urologists average around two lawsuits during their careers, irrespective of their professional reputation (19). Information regarding a history of malpractice litigation, even when favorably resolved, must be reported on various applications indefinitely. This information is now publicly available to facilitate total transparency within the medical profession. On a psychological level, the impact can be personally devastating. The physician may feel personally attacked and betrayed. Another aspect commonly ignored in malpractice litigation is the time it takes to resolve cases. In a recent study of testicular torsion malpractice cases, the average time from patient presentation to final verdict was 5 years (20). Understanding the characteristics of cases that have been both successfully and unsuccessfully litigated by institutions and practitioners alike may help urologists reduce their practice of “defensive medicine”.
Types of defendants
As individuals, urologists are the most common defendant in UC-related lawsuits. Over the 50-year period of our study, urologists were always successful in defending UC-related litigation at the state and federal levels. Other studies examining medical malpractice cases found that urologists are successful among 60% of defenses for cases dealing with endourology, 57.5% of defenses for penile prosthesis litigation, and 66% of defenses for litigation on testicular torsion (21-23). We demonstrate that UC litigation favors the defendant who is a urologist. This is reassuring for urologists, but it is important to examine how such lawsuits might be prevented.
When urologists were named as the sole defendant, common allegations were: a lack of informed consent, inadvertent UC removal, premature UC removal, UC-related trauma, and a retained UC fragment. Although most hospitals do not require a written consent form for placement of UCs (24), an informed discussion of the procedure, the reason for insertion, and its possible complications in conjunction with documentation may prevent misunderstandings between patients and urologists.
Institutions, usually hospitals but also nursing homes, were named in the majority of cases involving UC. Hospitals were named as defendants in (18/29, 62%) of lawsuits. Nurses were most commonly involved with the insertion and removal of catheters when hospitals or nursing homes were sued. Nurses were named in (5/29, 17%) lawsuits related to UCs. Notably, if they were named, nurses were never the sole defendant and the outcomes favored the defendant in all cases. The lawsuits involving nurses as defendants focused on specific behaviors by individual nurses involving UC placement, UC care, and UC removal.
Outcomes in favor of plaintiff
For UC-related lawsuits that resulted in indemnity payments to plaintiffs, the reasons for the lawsuits involved four UC removal-related cases (Table 3: Cases #1, 4, 5 and 6), three UC trauma or improper insertion cases (Cases #3, 7 and 9), two lack of patient consent cases (Cases #2 and 8), and one UC mechanical failure case (Case #10).
Cases of urethral trauma from UC placement and/or removal are often decided in favor of the plaintiff. Incomplete balloon deflation or premature balloon inflation causing prostatic or urethral trauma was also a common reason that plaintiffs won indemnity payments or settlements—4/5 cases were decided in favor of plaintiffs (Case #4, 5, 6, 9). The standard practice of using catheter securing devices and training staff on safe UC placement and removal techniques has been shown to reduce catheter-related trauma by 78.6% (25,26). We also identified a lawsuit whereby a portion of the UC being left in the bladder. Training for hospital personnel who remove UCs should include inspecting it grossly and documenting whether the catheter was removed intact.
In our study, (7/29, 24%) cases were complicated by a CAUTI; four were closed with an indemnity payment to the plaintiffs. UCs may contribute up to 80% of healthcare-associated UTIs leading to extended hospital stays, increased health care costs, and patient morbidity and mortality (27). Monitoring urine output was the leading cause for UC insertion in our malpractice population. The risk of a CAUTI can be prevented by minimizing unnecessary and prolonged use of UCs (10,28,29). Hospitals should take advantage of on-line tools designed to increase awareness of and to prevent CAUTI (30-32). Furthermore, adhering to UC hospital policies may help hospital defendants defend instances of appropriate catheter use. A study done by Gokula et al. showed that staff education and an indication checklist for each UC placement reduced the total number of unnecessary UCs used (33).
It has been found that catheterization in older patients without specific indications is associated with greater risk of death and a longer hospital stay (34). In (4/29, 14%) cases in our study, serious complications and even death from urosepsis were claimed with two cases favoring the plaintiff and an average of $317,500 was awarded in indemnity payments. While minimizing risk of UTI is usually focused on removing unnecessary catheters, in Case #7 the UTI and subsequent death of the patient was attributed to a delay in UC placement for a patient in urinary retention.
Indemnity payments
In this study, plaintiffs were more likely to win if the defendant was a hospital or nursing home. No indemnity payments were awarded to plaintiffs when defendants were individual physicians. With a small sample size, it is unclear if being a urologist is protective against UC-related litigation. The mean indemnity award paid to plaintiffs was $112,991 in catheter-related litigation, which is lower than estimated average medical malpractice indemnity payments in endourology ($364,722) and penile prosthesis malpractice suits ($831,050), although these studies used other legal databases than LexisNexis (21,23). Moreover, institutions, such as hospitals and nursing homes, rather than urologists, have been historically responsible for all indemnity payments.
Our study has limitations. Given how UC usage are exceedingly common, our sample size is relatively small and derived over a long time period. Although the LexisNexis database includes most state and federal cases, it does not give the total number of claims filed and the percentage of claims closed with or without indemnity payments. It does not give the total number of patients undergoing UC placement. Furthermore, it captures incomplete data about trial verdict outcomes and lacks data on settlements before trial. Presumably, many smaller cases are likely settled or resolved outside of court. These parameters are essential to accurately assess the true unbiased risk of UC liability. Some variables that could affect malpractice litigation were not included in the study due to varying availability in each case in the database such as physical exam findings, plaintiffs’ demographic characteristics or provider counseling role.
Despite these limitations, we believe that this study best characterizes the litigation surrounding UC use in medicine. Based on cases that ended in favor of plaintiffs in this study, our recommendations to all healthcare providers are as follows: (I) all healthcare providers should be well trained in UC insertion and proper technique prior to initiating placement; (II) providers should assess the integrity of UC and balloon prior to insertion; (III) providers should ensure that the UC is properly secured to prevent trauma; (IV) providers should periodically review the necessity of UCs and always remove them when no longer indicated; (V) providers should ensure that the UC balloon is fully deflated prior to removal. Perhaps if these six suggestions had been followed by providers, the prevalence of UC-related litigation would be even lower.
Finally, we believe that by understanding the defendant and claim characteristics of UC-related litigation, our results are reassuring to practicing urologists whom historically are not faulted in UC-related litigation. Future areas of research should focus on examining litigation correlating legal verdicts with patient’s perception of care to understand drivers of patient satisfaction.
Conclusions
Despite widespread usage of UCs over a 50-year period, state and federal lawsuits involving UC misuse are rare. Of litigated cases, urologists are commonly involved yet have successful defenses in both state and federal courts. Counseling healthcare providers on pitfalls of UCs use may be beneficial to prevent injury and malpractice litigation.
Acknowledgements
This work was supported by the Alafi Foundation .
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mohr JC. American medical malpractice litigation in historical perspective. JAMA 2000;283:1731-7. [Crossref] [PubMed]
- De Ville K. Medical malpractice in nineteenth-century America: origins and legacy. New York: NYU Press, 1992.
- Hershey N. The defensive practice of medicine. Myth or reality. Milbank Mem Fund Q 1972;50:69-98. [Crossref] [PubMed]
- Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005;293:2609-17. [Crossref] [PubMed]
- Feneley RC, Hopley IB, Wells PN. Urinary catheters: history, current status, adverse events and research agenda. J Med Eng Technol 2015;39:459-70. [Crossref] [PubMed]
- Haley RW, Hooton TM, Culver DH, et al. Nosocomial infections in U.S. hospitals, 1975-1976: estimated frequency by selected characteristics of patients. Am J Med 1981;70:947-59. [Crossref] [PubMed]
- Saint S, Wiese J, Amory JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med 2000;109:476-80. [Crossref] [PubMed]
- Fernández-Ruiz M, Calvo B, Vara R, et al. Inappropriate use of urinary catheters in patients admitted to medical wards in a university hospital. Enferm Infecc Microbiol Clin 2013;31:523-5. [Crossref] [PubMed]
- Munasinghe RL, Yazdani H, Siddique M, et al. Appropriateness of use of indwelling urinary catheters in patients admitted to the medical service. Infect Control Hosp Epidemiol 2001;22:647-9. [Crossref] [PubMed]
- Stamm WE, Martin SM, Bennett JV. Epidemiology of nosocomial infection due to Gram-negative bacilli: aspects relevant to development and use of vaccines. J Infect Dis 1977;136 Suppl:S151-60. [Crossref] [PubMed]
- Tambyah PA, Oon J. Catheter-associated urinary tract infection. Curr Opin Infect Dis 2012;25:365-70. [Crossref] [PubMed]
- Hollingsworth JM, Rogers MA, Krein SL, et al. Determining the noninfectious complications of indwelling urethral catheters: a systematic review and meta-analysis. Ann Intern Med 2013;159:401-10. [Crossref] [PubMed]
- Gonzalgo ML, Walsh PC. Balloon cuffing and management of the entrapped Foley catheter. Urology 2003;61:825-7. [Crossref] [PubMed]
- LexisNexis Academic Brochure. 2015; Available online: http://www.lexisnexis.com/pdf/academic/LexisNexis_Academic_Brochure_2015.pdf
- Weiss AJ, Elixhauser A. Statistical Brief 2012;180:2016.
- Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2014;23:277-89. [Crossref] [PubMed]
- Sherer BA, Coogan CL. The Current State of Medical Malpractice in Urology. Urology 2015;86:2-9. [Crossref] [PubMed]
- Sobel DL, Loughlin KR, Coogan CL. Medical malpractice liability in clinical urology: a survey of practicing urologists. J Urol 2006;175:1847-51. [Crossref] [PubMed]
- Kaplan GW. Malpractice risks for urologists. Urology 1998;51:183-5. [Crossref] [PubMed]
- Gaither TW, Copp HL. State appellant cases for testicular torsion: Case review from 1985 to 2015. J Pediatr Urol 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Sunaryo PL, Colaco M, Terlecki R. Penile prostheses and the litigious patient: a legal database review. J Sex Med 2014;11:2589-94. [Crossref] [PubMed]
- Colaco M, Heavner M, Sunaryo P, et al. Malpractice Litigation and Testicular Torsion: A Legal Database Review. J Emerg Med 2015;49:849-54. [Crossref] [PubMed]
- Duty B, Okhunov Z, Okeke Z, et al. Medical malpractice in endourology: analysis of closed cases from the State of New York. J Urol 2012;187:528-32. [Crossref] [PubMed]
- Manthous CA, DeGirolamo A, Haddad C, et al. Informed consent for medical procedures: local and national practices. Chest 2003;124:1978-84. [Crossref] [PubMed]
- Kashefi C, Messer K, Barden R, et al. Incidence and prevention of iatrogenic urethral injuries. J Urol 2008;179:2254-7; discussion 2257-8. [Crossref] [PubMed]
- Manalo M Jr, Lapitan MC, Buckley BS. Medical interns' knowledge and training regarding urethral catheter insertion and insertion-related urethral injury in male patients. BMC Med Educ 2011;11:73. [Crossref] [PubMed]
- Kleinpell RM, Munro CL, Giuliano KK. Targeting Health Care–Associated Infections: Evidence-Based Strategies. In: Hughes RG. editor. SourcePatient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US), 2008. Chapter 42.
- Daifuku R, Stamm WE. Association of rectal and urethral colonization with urinary tract infection in patients with indwelling catheters. JAMA 1984;252:2028-30. [Crossref] [PubMed]
- Umscheid CA, Mitchell MD, Doshi JA, et al. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol 2011;32:101-14. [Crossref] [PubMed]
- CDC CAUTI Prevention Guidlines. Available online: (April 26, 2016).http://www.cdc.gov/HAI/ca_uti/uti.html
- American Nurses Association CAUTI Prevention Tool. Available online: (April 27, 2016).http://nursingworld.org/ANA-CAUTI-Prevention-Tool
- Catheter-associated Urinary Tract Infection (CAUTI) Toolkit. Available online: (April 27, 2016).http://www.cdc.gov/HAI/pdfs/toolkits/CAUTItoolkit_3_10.pdf
- Gokula RM, Smith MA, Hickner J. Emergency room staff education and use of a urinary catheter indication sheet improves appropriate use of foley catheters. Am J Infect Control 2007;35:589-93. [Crossref] [PubMed]
- Holroyd-Leduc JM, Sen S, Bertenthal D, et al. The relationship of indwelling urinary catheters to death, length of hospital stay, functional decline, and nursing home admission in hospitalized older medical patients. J Am Geriatr Soc 2007;55:227-33. [Crossref] [PubMed]


