Psychosexual therapy for premature ejaculation
Introduction
Premature ejaculation (PE) is a male sexual dysfunction that creates considerable anguish for the man, his partner and their relationship (1). The precise etiology of PE is unknown although it is likely to include both biological (genetic, somatic and neurobiological) and psychological (interpersonal issues, performance anxiety, cognitive distortions) components (2). This article focuses on psychotherapy and combined pharmacological and psychological interventions for men with lifelong, acquired, natural VPE and SPE. The reader is referred to Drs. Hisasue and McMahon’s manuscripts on pharmacotherapy for PE, also found in this volume of TAU.
Definitions and premature ejaculation (PE) subtypes
The definition of PE has gone through several iterations beginning with expert based definitions that were vague, imprecise, and subjective as well as being unreliable from one clinician to the next (3). The most recent evidenced based definition appearing in the Diagnostic and Statistical Manual of Mental Disorders-5th Edition (DSM-5) is as follows (4):
PE (302.75)
- A persistent or recurrent pattern of ejaculation occurring during partnered sexual activity within approximately 1 minute following vaginal penetration and before the individual wishes it;
- The symptom in Criterion A must have been present for at least six months and must be experienced on almost all or all (approximately 75–100%) occasions of sexual activity (in identified situation contexts or, if generalized, in all contexts);
- The symptom in Criterion A causes clinically significant distress in the individual;
- The sexual dysfunction is not better explained by a nonsexual mental disorder or as a consequence of severe relationship distress or other significant stressors and is not attributable to the effects of a substance/medication or another medical condition.
- Specify
- Lifelong vs. acquired;
- Generalized vs. situational;
- Severity: mild, moderate or severe.
There are several strengths and weaknesses of the DSM-5 definition. Its greatest strength is the clear, objective criterion, particularly the evidenced based cutoff for intravaginal ejaculatory latency time (IELT). The previous definition which appeared in DSM-IV-TR was vague, non-specific and subjective (5). For instance, as regards ejaculatory latency DSM-IV characterized it as ejaculation “on, or shortly after penetration and before the person wishes it.” The precision of DSM-5 criterion will improve the reliability between clinicians and consistency amongst those conducting research on ejaculatory dysfunctions.
One of the weaknesses of the DSM-5 definition is that it applies to both lifelong and acquired forms of PE. Population based studies have been conducted on the IELT in men with lifelong PE (6,7); however, evidenced-based studies on the IELT reduction for acquired PE are lacking. Controversy remains as to whether equivalent or different IELT cutoffs should apply to lifelong and acquired subtypes of PE. The salient issue for acquired PE is at what point does the IELT reduction from “normal” to dysfunctional occur. DSM-5 suggests equivalency; however, the International Society for Sexual Medicine (ISSM) PE Guidelines Committee offered an alternative recommendation defining acquired PE as a clinically significant and bothersome reduction in latency time often to about 3 minutes or less (8). Future research will determine the soundness of the DSM-5, ISSM or a yet to be determined alternative definition of acquired PE definition.
Another weakness of the DSM-5 definition is the heterosexist bias in that it only refers to intravaginal intercourse and neglects men having sex with men or other forms of sexual activity. In general, correlations between coital, oral sex and masturbatory latencies are not consistently high.
In addition to lifelong and acquired forms of PE, Waldinger proposed two other subtypes of PE: VPE and SPE (9,10). These subtypes should be considered provisional but they characterize men who do not meet the DSM-5 or ISSM criterion but are distressed and seeking help for their ejaculatory concerns. VPE is identified by a short ejaculatory latency which occurs irregularly and inconsistently with some subjective sense of diminished control of ejaculation. This subtype is not considered a sexual dysfunction but rather a normal variation in sexual performance. SPE is characterized by one or more of the following: (I) subjective perception of consistent or inconsistent short IELT; (II) preoccupation with an imagined short ejaculatory latency or lack of control over the timing of ejaculation; (III) actual IELT in the normal range or even of longer duration (i.e., an ejaculation that occurs after 5 minutes); (IV) ability to control ejaculation (i.e., to withhold ejaculation at the moment of imminent ejaculation) that may be diminished or lacking and; (V) the preoccupation that is not better accounted for by another mental disorder.
General considerations regarding the psychotherapy of premature ejaculation (PE)
Present day psychotherapy for PE is an integration of psychodynamic, systems, behavioral and cognitive approaches within a short-term psychotherapy model (11-13). The guiding principles of treatment are to learn to control ejaculation and manage and resolve the ever expanding snowball effect that PE has on the man, partner and couple. Often these snowball effects include the development of performance anxiety, diminished self-esteem, avoidance of sexual activity, partner’s anger and hostility and a significant decrease in the quality of the interpersonal relationship.
Clinicians of different theoretical training have diverse explanations as to why a man suffers from PE. Psychodynamic clinicians highlight unconscious hostile emotional states toward women, excessive narcissism, fears of the vagina causing them harm, a passive pleasure in losing control of urination and soiling or debasing women (14-19). Behavioral clinicians understand PE as due to lack of sensory awareness (not cueing in to their levels of sexual excitement) or responses conditioned by early learned experiences (e.g., hasty and nervous lovemaking in the back seat of a car) (16,20,21). Cognitive therapists examine the distortions in thinking that maintain or worsen the PE (e.g., catastrophizing, overgeneralization, mind reading, etc.) (22,23). Family/relationship therapists emphasize the dynamics of the relationship, power and control issues, and each partner’s management of emotional and sexual intimacy. Most psychotherapists/sex therapists blend ideas from different theoretical schools and offer men or couples an integrated psychological treatment format.
Donahey and Miller describe three common factors that make psychotherapy effective (24). These include: (I) empowering the patient to experience themselves as having the ability to create change and impact contextual factors; (II) providing a safe and empathic environment where the patient can explore obstacles, choices and meanings of his psychological and behavioral dilemmas and; (III) and conveying hopefulness and realistic expectations regarding outcomes. These three components should be included in the psychological treatment of men and couples suffering from PE.
Psychotherapeutic interventions for lifelong, acquired, natural and subjective premature ejaculation (PE)
The psychological treatment of PE has multiple goals. These include: (I) learning techniques to control and/or delay ejaculation; (II) gaining confidence in their sexual performance; (III) lessening performance anxiety; (IV) modifying rigid sexual repertoires; (V) surmounting barriers to intimacy; (VI) resolving interpersonal issues that precipitate and maintain the dysfunction; (VII) coming to terms with feelings/thoughts that interfere with sexual function and; (VIII) increasing communication (12).
Psychotherapy for sexual problems is commonly referred to as sex therapy (25). In treating PE, sex therapists employ specific behavioral techniques like stop-start exercises or the squeeze technique. However, sex therapy is more than an amalgam of behavioral techniques; clinicians must also address relevant relationship factors, performance anxiety and partner concerns. Psychotherapy/sex therapy for PE can be conducted in either a couple’s, individual or group format. There are also experimental programs that offer psychoeducational treatment on the Internet or via telephone (26).
The ISSM PE Guidelines Committee recommended specific forms of treatment intervention for lifelong, acquired, natural and subjective types of PE (2). While there is clearly overlap between the four subtypes in the manner in which men, partners and couples subjectively experience PE there are also important differences between the subtypes. For example, men with lifelong PE have never, or rarely, experienced an extended intercourse while men with acquired PE had previously experienced normal intercourse latencies. In many instances the acquired men are more distressed because they know what they and their partners are missing. Lifelong men have accommodated to their situation, albeit with considerable distress for them and their partners. Men with subjective PE believe they suffer from PE in spite of having extended intercourse latencies. It is not the timing but the meaning they place on their experience. And finally, natural PE suffers fail to recognize the normal variation in their ejaculatory latencies and are excessively critical of themselves when they experience a rapid ejaculation. These differences between subtypes require clinicians to tailor their psychological interventions to the overall and specific experiences of men and their partners with each subtype of PE.
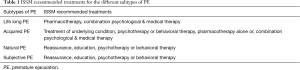
Table 1 is a summary of the PE treatment recommendations promulgated by the ISSM Guidelines Committee for all four subtypes of PE (2). Because lifelong PE is thought to have a primarily neurobiological basis pharmacotherapy is generally a first line recommendation. Again, I refer the reader to Drs. Hisasue and McMahon’s manuscripts in this volume for a more comprehensive review of pharmacotherapy for PE. Conversely, because no biological factors are thought to underlie natural and subjective PE, pharmacotherapy is not recommended.
Full table
Acquired PE may have some associated biological factors such as ED, prostatitis and hyperthyroidism. These conditions should be treated first. Should the PE persist after treating these biological factors, the patient and clinician should consider pharmacotherapy, psychotherapy or a combination of pharmaco- and psychotherapy. Reassurance, education and psychotherapy are the recommended interventions to treat natural and subjective PE.
Combination treatment involves stepwise or simultaneous use of both pharmacological and psychological/behavioral interventions (27,28). Combined therapy provides men with a medication to delay ejaculation while they learn behavioral techniques to delay ejaculation and address the relevant psychological and interpersonal issues. If possible, the medication is weened after six weeks or more as men have demonstrated reliable gains in IELT.
The most convincing combination therapy study compared men given dapoxetine 30 mg (a drug approved in over 60 countries to treat PE) to men receiving dapoxetine 30 mg plus a brief psychological intervention (29). After 24 weeks, the dapoxetine only group demonstrated a 2-fold IELT increase while the combination group increased almost four-fold. There are four additional studies that confirm the superiority of combination treatment versus drug treatment alone for men with PE (30-33).
Despite the evidence, clinicians are reluctant to abandon established practice patterns and integrate methods from different disciplines without receiving formal training. In my opinion sexual medicine will embrace combination therapy approaches as they gain in recognition and attractiveness.
Specific behavioral and cognitive techniques
Men with PE fear focusing on their sexual excitement, believing it will cause them to ejaculate even more quickly. They employ clever distraction techniques such as: performing complex mathematical computations, thinking about stock market investments, the win/loss record of sports teams or statistics on their favorite athletes. Men will also excessively drink alcohol hoping to diminish their sexual excitement; should they judge their alcohol intake incorrectly they need not worry about PE as they will likely not be able to achieve or maintain an erection. PE suffers will also use multiple condoms, desensitizing ointments or sprays or repeatedly masturbate prior to intercourse. These tactics, however creative, curtail the pleasures of lovemaking and are generally unsuccessful.
In partnered sexual situations, because of their fear of sexual excitement, these men will restrict their partners from touching them and provide little stimulation to their partners. Research on the distress of female partners of PE men highlight his lack of attention to the partner, his excessive focus on performance, short IELT, and lack of ejaculatory control (34).
Given their fear and lack of focus on their sexual excitement PE men typically describe themselves as having two points on the sexual excitement continuum- no excitement and the point of ejaculatory inevitability. Behavioral interventions, such as the stop-start technique, aim to help men attend to their level of arousal without fear and learn to linger in the mid-range of sexual excitement. By utilizing graduated behavioral exercises, they are taught to identify and become familiar with intermediate levels of sexual excitement. Successively, beginning with masturbation and moving progressively through foreplay and intercourse, they master the ability to linger in a mid-range level of excitement, thereby delaying ejaculation.
It is also helpful to address the cognitive alterations that help maintain the dysfunction. Rosen et al. list describes the following cognitive distortions: (I) all or nothing thinking, e.g., “I am a complete failure because I come quickly”; (II) overgeneralization, e.g., “If I had trouble controlling my ejaculation last night, I won’t be able to this morning”; (III) disqualifying the positive, e.g., “My partner says our lovemaking is satisfying because she doesn’t want to hurt my feelings”; (IV) mind reading, e.g., “I don’t need to ask, I know how she felt about last night”; (V) fortune telling, e.g., “I am sure things will go badly tonight”; (VI) emotional reasoning, e.g., “Because a man feels something is true, it must be”; (VII) categorical imperatives, i.e., ‘shoulds’, ‘ought to’ and ‘musts’ dominate the man’s cognitive processes and; (VIII) catastrophizing, e.g., “If I fail tonight my girlfriend will dump me.” (22).
Interpersonal issues
Which came first?—did the PE cause the interpersonal concerns or did interpersonal issues cause the PE. In my experience the effects are bi-directional. In some circumstances the PE has resulted from interpersonal conflict; in others the PE exists in a secure, stable and loving relationship. PE however, generally negatively impacts the relationship.
Men feel diminished by their PE. Some blame their partners (e.g., she’s too sexy, I can’t help it), others worry that their partners will have affairs, some try incessantly to please their partners via non-coital behaviors, only to be rejected in their attempts. Female partners are distressed that the man has been unable or unwilling to fix the problem and resent his preoccupation with his performance during lovemaking. Additionally, female partners dislike the abrupt cessation in emotional intimacy that occurs when the man ejaculates. He feels ashamed and turns away from her; she is left feeling abandoned and angry. As mentioned previously these issues continue to grow and snowball into more chronic contentious issues.
Therapists seek to help couples reclaim their sexual and emotional intimacy while decreasing the hostility and withdrawal from one another. Helping couples to surmount these obstacles, finding rational solutions to their conflicts and working constructively together to solve the issues are the primary goals of relationship therapy for PE.
Psychotherapy outcome
The majority of psychotherapy outcome studies do not meet the standard for evidenced-based medicine. They tend to be uncontrolled (no wait list or sham intervention), employ small sample sizes without adequate follow-up, and because of definitional controversies are studying very different groups of PE men (e.g., in some PE groups the IELT is 2 minutes; in others, it is 6 or more minutes). Due to the inadequate quality of the research, meta-analytic studies include very few studies in their reviews. One meta-analytic review concluded that there is limited evidence that physical behavioral techniques improve IELT and other outcomes over waitlist controls (35); two other meta-analyses found that there was weak and inconsistent evidence for psychological interventions for PE (36,37). All three meta-analysis concluded that there is good evidence for the use of combination therapy (more efficacious than drug alone).
There are however, two psychotherapy studies of modest sample size that provide useful data. De Carufel and Trudel demonstrated an eightfold increase in IELT among men treated with psychological intervention (education on sensuality, movement of the body, speed of sexual activity, muscular tension and breathing, squeeze and stop/start techniques) compared with a wait-list control condition (38). Masters and Johnson reported the results of using the squeeze technique, sensate focus, individual and conjoint therapy as well as sexual skills and communication training (21). Their “failure rates” were 2.2% and 2.7% immediately post therapy and at a 5-year follow-up respectively (21). Clearly, more research employing better sampling, statistical and outcome methods needs to be conducted.
Discussion
In general, psychological interventions offer promising treatment options for sexual dysfunctions. As regards PE, psychological therapies address both the rapidity of the ejaculatory response and the burden that the dysfunction has on the man, partner and couple. Combination pharmaco- and psychotherapy offers superior efficacy to drug alone. This is because men and couples learn sexual skills, address the intrapsychic, interpersonal and cognitive issues that precipitate and maintain the dysfunction.
Additionally, we now have improved outcome measures [Index of Premature Ejaculation, Premature (39) Ejaculation Profile (40) and Premature Ejaculation Diagnostic Tool (41)] that allow researchers to better examine the efficacy of their interventions on subjects. Likewise we also have agreement on who does and does not suffer from PE so moving forward there should be increased homogeneity of treatment groups.
Sexual skills training, couples, and cognitive therapy, are all helpful in alleviating the anguish of men, partners and couples who suffer from PE. Hopefully more studies will be conducted and included in future meta-analysis to better judge the quality of psychological interventions.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Althof is a consultant or Advisory Board Member to: Allergan, Aytu, Astellas, Ixchelsis, Eli Lilly, Palatin, Pfizer, Promescent, Sprout, S1, Strategic Science Technologies and Valeant. He conducts clinical trials for Allergan, Ixchelsis, Evidera, Palatin and Trimel.
References
- Rowland DL, Patrick DL, Rothman M, et al. The psychological burden of premature ejaculation. J Urol 2007;177:1065-70. [Crossref] [PubMed]
- Althof SE, McMahon CG, Waldinger MD, et al. An update of the International Society of Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE). J Sex Med 2014;11:1392-422. [Crossref] [PubMed]
- McMahon CG, Althof SE, Waldinger MD, et al. An evidence-based definition of lifelong premature ejaculation: report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J Sex Med 2008;5:1590-606. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Fifth Edition. Washington, DC: American Psychiatric Association, 2013.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Washington, DC: American Psychiatric Association, 2000.
- Giuliano F, Patrick DL, Porst H, et al. Premature ejaculation: results from a five-country European observational study. Eur Urol 2008;53:1048-57. [Crossref] [PubMed]
- Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med 2009;6:2888-95. [Crossref] [PubMed]
- Serefoglu EC, McMahon CG, Waldinger MD, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. J Sex Med 2014;11:1423-41. [Crossref] [PubMed]
- Waldinger MD. Premature ejaculation: different pathophysiologies and etiologies determine its treatment. J Sex Marital Ther 2008;34:1-13. [Crossref] [PubMed]
- Waldinger M. Pathophysiology of Lifelong Premature Ejaculation. In: Jannini EA, McMahon CG, Waldinger MD. editors. Premature Ejaculation From Etiology to Diagnosis and Treatment. Springer-Verlag Italia, 2013:71-80.
- Althof SE. Psychological treatment strategies for rapid ejaculation: rationale, practical aspects, and outcome. World J Urol 2005;23:89-92. [Crossref] [PubMed]
- Althof SE. Psychological approaches to the treatment of rapid ejaculation. The Journal of Men's Health & Gender 2006;3:180-6. [Crossref]
- Althof SE. Treatment of Premature Ejaculation: Psychotherapy, Pharmacotherapy, and Combined Therapy. Binik YM, Hall KS. Principles and Practice of Sex Therapy, Fifth Edition. New York: Guilford Press, 2014:112-37.
- Bergler E. Some special varieties of ejaculatory disturbance not hitherto described. International Journal of Psychoanalysis 1935;16:84-95.
- Fenichel O. The Psychoanalytic Theory of Neurosis. New York: Norton, 1945.
- Kaplan HS. The New Sex Therapy. New York: Brunner/Mazel, 1974.
- Levine SB. Marital sexual dysfunction: ejaculation disturbances. Ann Intern Med 1976;84:575-9. [Crossref] [PubMed]
- Ovesey L, Meyers H. Retarded ejaculation. Psychodynamics and psychotherapy. Am J Psychother 1968;22:185-201. [PubMed]
- Schapiro B. Premature ejaculation, a review of 1130 cases. J Urol 1943;50:374-9.
- Bancroft J. Human Sexuality and its Problems, 3rd Edition. Churchill Livingstone, 2008.
- Masters WH, Johnson VE. Human Sexual Inadequacy. Boston: Little, Brown, 1970.
- Rosen RC, Leiblum SR, Spector IP. Psychologically based treatment for male erectile disorder: a cognitive-interpersonal model. J Sex Marital Ther 1994;20:67-85. [Crossref] [PubMed]
- McCarthy BW. Cognitive-behavioral strategies and techniques in the treatment of early ejaculation. In: Leiblum SR, Rosen RC. editors. New York: Guilford, 1990:141-67.
- Donahey KM, Miller SD. What works in sex therapy: a common factors perspective. In: Klein-platz PJ. editor. New directions in sex therapy: innovations and alternatives. Philadelphia: Bruner Routledge, 2001:210-33.
- Althof SE. Sex therapy and combined (sex and medical) therapy. J Sex Med 2011;8:1827-8. [Crossref] [PubMed]
- van Lankveld JJ, Leusink P, van Diest S, et al. Internet-based brief sex therapy for heterosexual men with sexual dysfunctions: a randomized controlled pilot trial. J Sex Med 2009;6:2224-36. [Crossref] [PubMed]
- Perelman MA. Sex coaching for physicians: combination treatment for patient and partner. Int J Impot Res 2003;15 Suppl 5:S67-74. [Crossref] [PubMed]
- Perelman MA. A new combination treatment for premature ejaculation: a sex therapist's perspective. J Sex Med 2006;3:1004-12. [Crossref] [PubMed]
- Cormio L, Massenio P, La Rocca R, et al. The Combination of Dapoxetine and Behavioral Treatment Provides Better Results than Dapoxetine Alone in the Management of Patients with Lifelong Premature Ejaculation. J Sex Med 2015;12:1609-15. [Crossref] [PubMed]
- Li P, Zhu GS, Xu P, et al. Interventional effect of behaviour psychotherapy on patients with premature ejaculation. Zhonghua Nan Ke Xue 2006;12:717-9. [PubMed]
- Tang W, Ma L, Zhao L, et al. Clinical efficacy of Viagra with behavior therapy against premature ejaculation. Zhonghua Nan Ke Xue 2004;10:366-7, 370. [PubMed]
- Yuan P, Dai J, Yang Y, et al. A comparative study on treatment for premature ejaculation: citalopram used in combination with behavioral therapy versus either citalopram or behavioral therapy alone Chinnese Journal of Andrology 2008;22:35-8. [Chinese].
- Shao X, Li J. Clinical study on treatment of premature ejaculation with Paroxetine and behavior-therapy. Chinese Journal of Andrology 2008;22:18-20.
- Burri A, Giuliano F, McMahon C, et al. Female partner's perception of premature ejaculation and its impact on relationship breakups, relationship quality, and sexual satisfaction. J Sex Med 2014;11:2243-55. [Crossref] [PubMed]
- Cooper K, Martyn-St James M, Kaltenthaler E, et al. Behavioral Therapies for Management of Premature Ejaculation: A Systematic Review. Sex Med 2015;3:174-88. [Crossref] [PubMed]
- Frühauf S, Gerger H, Schmidt HM, et al. Efficacy of Psychological Interventions for Sexual Dysfunction: A Systematic Review and Meta-Analysis. Arch Sex Behav 2013;42:915-33. [Crossref] [PubMed]
- Melnik T, Althof S, Atallah ÁN, et al. Psychosocial interventions for premature ejaculation. Cochrane Database Syst Rev 2011.CD008195. [PubMed]
- De Carufel F, Trudel G. Effects of a new functional-sexological treatment for premature ejaculation. J Sex Marital Ther 2006;32:97-114. [Crossref] [PubMed]
- Althof S, Rosen R, Symonds T, et al. Development and validation of a new questionnaire to assess sexual satisfaction, control, and distress associated with premature ejaculation. J Sex Med 2006;3:465-75. [Crossref] [PubMed]
- Patrick DL, Giuliano F, Ho KF, et al. The Premature Ejaculation Profile: validation of self-reported outcome measures for research and practice. BJU Int 2009;103:358-64. [Crossref] [PubMed]
- Symonds T, Perelman MA, Althof S, et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol 2007;52:565-73. [Crossref] [PubMed]


