Classification and definition of premature ejaculation
Introduction
Premature ejaculation (PE) is a poorly understood condition that effects up to 30% of the male population and is considered as the most common sexual disorder in men (1). The ambiguity surrounding PE is in part due to the difficulty in conducting and interpreting research in the absence of a standardised universal definition that adequately encompasses the characteristics of these patients (2). Perceptions regarding what truly is a “normal ejaculation time”, as well as variability of socioeconomic and cultural characteristics among men with the complaint of PE have hampered efforts to establish a universal definition and classification of the disease of PE (3).
An enhanced awareness of sexual dysfunction in the recent decades has lead to an increase in scientific research that has challenged the traditional paradigm regarding PE and has supported a possible physiological basis (4). Having previously been considered singly as a psychologically disorder, PE is now understood to be far more complex with multiple etiological factors playing a role in its pathogenesis (5). These advances in understanding PE necessitated the development of an evidence-based definition and classification to enable the scientific community to design methodologically rigorous studies on the topic.
Definition of PE
Since the first report of PE in the medical literature in 1887 (6), several definitions have been proposed, the most recent of which are summarized in Table 1.

Full table
The first recognisable definition of PE was proposed by Masters and Johnson in 1970, who defined the condition as “The inability of a man to delay ejaculation long enough for his partner to reach orgasm on 50% of intercourse attempts” (9). This definition, although a step in the right direction of raising awareness of the condition, suffered from an important limitation. It encompassed the role of the female partners and therefore could be confounded by the women’s ability to climax. Following this, professional bodies and individuals have proposed a number of definitions. Many of these were based on specialists’ opinions rather than evidence, lacked operational criteria and specificity, and had shortcomings in their interpretation by clinicians (10).
In 1980, the American Psychiatric Association (APA) released the Diagnostic and Statistical Manual of Mental Disorders 3rd edition (DSM-3), which was based on the recommendations of opinion leaders of the time (11). The use of ambiguous terminology (e.g., reasonable voluntary control) made the definition open to inter-observer variability and rendered it effectively unusable as a research tool. The subsequent iteration, DSM-IV, aimed to address this deficiency by including a time component with the phrase “short ejaculation time”, but removed control as an important element (12). Therefore, the DSM-IV definition was not specific enough to recommend an actual cut-off time to operationalize the ‘short ejaculation time’.
The International Statistical Classification of Disease 10th edition (ISCD-10) was released in 1994, and was the first definition to propose a time limit as part of the definition (13). This proposed that ejaculation 15 seconds or less after penetration constituted PE, although the evidence that supported this cut-off is unclear (14,15). Subsequent definitions have sought to include a suggested time limit to help standardise their application.
Early definitions of PE were criticized for being vague, open to multiple interpretations and for lacking operational criteria (10). Mounting pressure from regulators including the United States Food and Drug Administration (FDA), and general dissatisfaction with the heterogeneity of the definitions prompted a re-examination. In 2007 (10) and then 2013 (2), the International Society for Sexual Medicine (ISSM) convened a committee of internationally recognised experts to create a definition, which addressed the criticisms levied against previous attempts. They acknowledged that, although ‘lifelong’ and ‘acquired’ PE were different entities, they shared the same common constructs as identified above and therefore by using these, a unifying definition could be worked up. Out of this they identified three domains which appeared to underpin the majority of definitions: (I) short ejaculatory latency; (II) a perceived lack of control; (III) negative personal consequences including distress, frustration, avoidance of intercourse and interpersonal issues (10).
Short ejaculatory latency
The use of ejaculatory latency is an important component in creating a definition that satisfies the need to have an operationalized definition enabling uniformity in application and subsequent research. A number of papers support the use of intravaginal ejaculatory latency time (IELT) shown in Table 2.

Full table
Data by Waldinger et al. and later McMahon suggested that lifelong PE was characterised by an IELT of around 1 minute or less (16,17). Waldinger et al. examined 110 men with lifelong PE and demonstrated that 90% of them had IIELTs less than 1 minute. Only 10% of these men ejaculated between 1–2 minutes (16). McMahon found similarly that 77% of men with PE ejaculated within 1 minute (17).
A further paper by the Waldinger in 2005 examined the stopwatch IELT of a group of randomly unselected men across 5 counties, and after examining the 0.5 and 2.5 percentiles corresponded to an IELT of 0.9 and 1.3 minutes respectively (19). Consequently an IELT of 1 minute should capture 80–90% of patients with PE.
Ejaculatory control
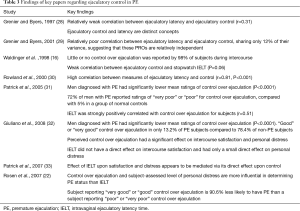
The inability to delay or control ejaculation is postulated to be an important factor in PE in a number of studies (see Table 3).
Full table
Patrick et al. found that low ratings for control over ejaculation were linked with shorter IELT (31). PE subjects were more likely to give ratings of “poor” or “very poor” control than their non-PE counterparts (72% vs. 5%; P<0.0001) (31). Of the patients with an IELT of <1 minute, 67.7% reported poor or very poor control compared with 10.2% with an IELT of >1 minute (31).
A number of studies have only demonstrated a moderate or no correlation between IELT and reported ejaculatory control. Grenier and Byers in 1997 and in 2001 demonstrated only a weak correlation between IELT and control, supporting that they were relatively independent factors (28,29).
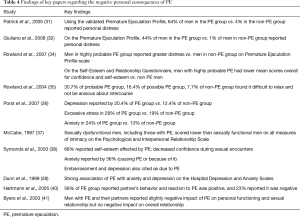
Negative personal consequences
PE clearly has an effect on the psyche of its sufferer, as well as their partners. A number of studies have examined the relationship of PE to negative personal consequences of which the key papers are listed in Table 4 with their findings. In one community-based study examining 1,587 subjects of which 207 were diagnosed using the DSM-IV-TR criteria for PE, 64% in the PE group vs. 4% in non-PE group (P≤0.0001) rated “quite a bit” or “extremely” for personal distress and 31% vs. 1% (P<0.0001) respectively for interpersonal difficulty (31). The negative effect of PE on patients’ wellbeing has been corroborated by data from McCabe and Rowland as well as others (34,37).
Full table
Unfortunately, a review of the available literature did not furnish further recommendations on a unifying evidence-based definition. However, after assimilation of data in 2008, an evidence-based definition of lifelong PE was formulated (10):
- Ejaculation that always or nearly always occurs prior to or within about 1 minute of vaginal penetration; or a clinically significant and bothersome reduction in latency time, often to about 3 minutes or less;
- Inability to delay ejaculation on all, or nearly all, vaginal penetrations;
- Negative personal consequences, such as distress, bother, frustration and/or the avoidance of sexual intimacy.
This definition is not without its own limitations and faults. The definition limited itself to focussing only on vaginal penetration and chose to disregard other sexual activities such as oral/anal sex and masturbation, as well as ignoring the needs of men that have sex with men (MSM). Furthermore, it placed men who complained of PE intermittently or only during a period of their life outside of the definition. These limitations underlined the need for a better understanding of the classification of PE.
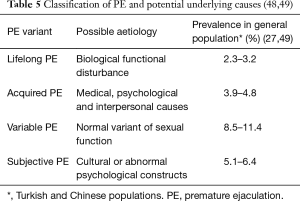
Classification of PE
The first attempt to classify PE was by Schapiro in 1943 who identified two groups of patients with PE: (I) type A—“hypotonic”, associated with erectile dysfunction and; (II) type B—“sexually hypertonic”, with a tendency to ejaculate rapidly from the first act of intercourse (42). These two groups were later relabelled as ‘primary or lifelong’ and ‘secondary or acquired’ (43).
The terms ‘psychogenic PE’ and ‘biogenic PE’ with further sub-characterisation have also been used, but have failed to gain traction in scientific publications (44,45).
Waldinger and Schweitzer identified a disparity in the prevalence of objectively measured PE i.e., IELTs of <1 minute in the general population (~2.5%) and the subjective self reporting of men with PE with IELT greater than 1 minute in other studies being much higher (19,31,32,46). As a consequence of this, they attempted to rationalise this difference by adding two new subtypes on top of the pre-existing lifelong and acquired PE: variable PE and subjective PE (14,47). Each of these subtypes appears to have a different aetiology and prevalence rates as shown in Table 5.
Conclusions
PE is a complex condition, which still remains incompletely characterised despite advances in our understanding over the last decade. As a consequence, the ability to define and classify the condition has been difficult. A move to a more evidence based approach as applied by the ISSM has improved the clinicians’ ability to define those who need treatment, as well as perform further research in this complex condition.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Curr Psychiatry Rep 2000;2:189-95. [Crossref] [PubMed]
- Serefoglu EC, McMahon CG, Waldinger MD, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. Sex Med 2014;2:41-59. [Crossref] [PubMed]
- Althof SE, McMahon CG, Waldinger MD, et al. An Update of the International Society of Sexual Medicine's Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). Sex Med 2014;2:60-90. [Crossref] [PubMed]
- Waldinger MD. The neurobiological approach to premature ejaculation. J Urol 2002;168:2359-67. [Crossref] [PubMed]
- Saitz TR, Serefoglu EC. Advances in understanding and treating premature ejaculation. Nat Rev Urol 2015;12:629-40. [Crossref] [PubMed]
- Gross S, editor. Practical treatise on impotence and sterility and allied disorders of the male sexual organs. Edinburg: YJ Pentland, 1887.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA: American Psychiatric Publishing, 2013.
- International Statistical Classification of Diseases and Related Health problems 10th Revision. Available online: http://apps.who.int/classifications/icd10/browse/2016/en
- Masters WH, Johnson VE, editors. Human sexual inadequacy. London; Boston: Churchill; Little, Brown, 1970.
- McMahon CG, Althof SE, Waldinger MD, et al. An evidence-based definition of lifelong premature ejaculation: report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J Sex Med 2008;5:1590-606. [Crossref] [PubMed]
- Diagnostic and Statistical Manual of Mental Disorders. 3rd (DSM III) edition. Washington: American Psychiatric Association, 1980.
- Diagnostic criteria from DSM-IV-TR. Washington, DC: American Psychiatric Association, 2000.
- Janca A, Ustün TB, Early TS, et al. The ICD-10 symptom checklist: a companion to the ICD-10 classification of mental and behavioural disorders. Soc Psychiatry Psychiatr Epidemiol 1993;28:239-42. [PubMed]
- Waldinger MD, Schweitzer DH. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part II--proposals for DSM-V and ICD-11. J Sex Med 2006;3:693-705. [Crossref] [PubMed]
- Waldinger MD, Schweitzer DH. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part I--validity of DSM-IV-TR. J Sex Med 2006;3:682-92. [Crossref] [PubMed]
- Waldinger MD, Hengeveld MW, Zwinderman AH, et al. An empirical operationalization study of DSM-IV diagnostic criteria for premature ejaculation. Int J Psychiatry Clin Pract 1998;2:287-93. [Crossref] [PubMed]
- McMahon CG. Long term results of treatment of premature ejaculation with serotonin re-uptake inhibitors. Int J Imp Res 2002;14:S19.
- Waldinger MD, Zwinderman AH, Olivier B, et al. The majority of men with lifelong premature ejaculation prefer daily drug treatment: an observation study in a consecutive group of Dutch men. J Sex Med 2007;4:1028-37. [Crossref] [PubMed]
- Waldinger MD, Quinn P, Dilleen M, et al. A multinational population survey of intravaginal ejaculation latency time. J Sex Med 2005;2:492-7. [Crossref] [PubMed]
- Althof SE, Levine SB, Corty EW, et al. A double-blind crossover trial of clomipramine for rapid ejaculation in 15 couples. J Clin Psychiatry 1995;56:402-7. [PubMed]
- Pryor JL, Broderick GA, Ho KF, et al. Comparison of estimated vs. measured intravaginal ejaculatory latency time (IELT) in men with and without premature ejaculation (PE). J Sex Med 2005;3:54.
- Rosen RC, McMahon CG, Niederberger C, et al. Correlates to the clinical diagnosis of premature ejaculation: results from a large observational study of men and their partners. J Urol 2007;177:1059-64. [Crossref] [PubMed]
- Porst H, McMahon CG, Althof SE, et al. Baseline characteristics and treatment outcomes for men with acquired or lifelong premature ejaculation with mild or no erectile dysfunction: integrated analyses of two phase 3 dapoxetine trials. J Sex Med 2010;7:2231-42. [Crossref] [PubMed]
- McMahon CG, Giuliano F, Dean J, et al. Efficacy and safety of dapoxetine in men with premature ejaculation and concomitant erectile dysfunction treated with a phosphodiesterase type 5 inhibitor: randomized, placebo-controlled, phase III study. J Sex Med 2013;10:2312-25. [Crossref] [PubMed]
- Serefoglu EC, Cimen HI, Atmaca AF, et al. The distribution of patients who seek treatment for the complaint of ejaculating prematurely according to the four premature ejaculation syndromes. J Sex Med 2010;7:810-5. [Crossref] [PubMed]
- Zhang X, Gao J, Liu J, et al. Distribution and factors associated with four premature ejaculation syndromes in outpatients complaining of ejaculating prematurely. J Sex Med 2013;10:1603-11. [Crossref] [PubMed]
- Gao J, Zhang X, Su P, et al. Prevalence and factors associated with the complaint of premature ejaculation and the four premature ejaculation syndromes: a large observational study in China. J Sex Med 2013;10:1874-81. [Crossref] [PubMed]
- Grenier G, Byers ES. The relationships among ejaculatory control, ejaculatory latency, and attempts to prolong heterosexual intercourse. Arch Sex Behav 1997;26:27-47. [Crossref] [PubMed]
- Grenier G, Byers S. Operationalizing premature or rapid ejaculation. J Sex Res 2001;38:369-78. [Crossref]
- Rowland DL, Strassberg DS, de Gouveia Brazao CA, et al. Ejaculatory latency and control in men with premature ejaculation: an analysis across sexual activities using multiple sources of information. J Psychosom Res 2000;48:69-77. [Crossref] [PubMed]
- Patrick DL, Althof SE, Pryor JL, et al. Premature ejaculation: an observational study of men and their partners. J Sex Med 2005;2:358-67. [Crossref] [PubMed]
- Giuliano F, Patrick DL, Porst H, et al. Premature ejaculation: results from a five-country European observational study. Eur Urol 2008;53:1048-57. [Crossref] [PubMed]
- Patrick DL, Rowland D, Rothman M. Interrelationships among measures of premature ejaculation: the central role of perceived control. J Sex Med 2007;4:780-8. [Crossref] [PubMed]
- Rowland DL, Patrick DL, Rothman M, et al. The psychological burden of premature ejaculation. J Urol 2007;177:1065-70. [Crossref] [PubMed]
- Rowland D, Perelman M, Althof S, et al. Self-reported premature ejaculation and aspects of sexual functioning and satisfaction. J Sex Med 2004;1:225-32. [Crossref] [PubMed]
- Porst H, Montorsi F, Rosen RC, et al. The Premature Ejaculation Prevalence and Attitudes (PEPA) survey: prevalence, comorbidities, and professional help-seeking. Eur Urol 2007;51:816-23; discussion 824. [Crossref] [PubMed]
- McCabe MP. Intimacy and quality of life among sexually dysfunctional men and women. J Sex Marital Ther 1997;23:276-90. [Crossref] [PubMed]
- Symonds T, Roblin D, Hart K, et al. How does premature ejaculation impact a man s life? J Sex Marital Ther 2003;29:361-70. [Crossref] [PubMed]
- Dunn KM, Croft PR, Hackett GI. Association of sexual problems with social, psychological, and physical problems in men and women: a cross sectional population survey. J Epidemiol Community Health 1999;53:144-8. [Crossref] [PubMed]
- Hartmann U, Schedlowski M, Kruger TH. Cognitive and partner-related factors in rapid ejaculation: differences between dysfunctional and functional men. World J Urol 2005;23:93-101. [Crossref] [PubMed]
- Byers ES, Grenier G. Premature or rapid ejaculation: heterosexual couples' perceptions of men's ejaculatory behavior. Arch Sex Behav 2003;32:261-70. [Crossref] [PubMed]
- Shapiro B. Premature ejaculation: A review of 1130 cases. J Urol 1943;50:374-9.
- Godpodinoff ML. Premature ejaculation: clinical subgroups and etiology. J Sex Marital Ther 1989;15:130-4. [Crossref] [PubMed]
- Metz ME, Pryor JL, Nesvacil LJ, et al. Premature ejaculation: a psychophysiological review. J Sex Marital Ther 1997;23:3-23. [Crossref] [PubMed]
- Metz ME, Pryor JL. Premature ejaculation: a psychophysiological approach for assessment and management. J Sex Marital Ther 2000;26:293-320. [Crossref] [PubMed]
- Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med 2009;6:2888-95. [Crossref] [PubMed]
- Waldinger MD, Schweitzer DH. The use of old and recent DSM definitions of premature ejaculation in observational studies: a contribution to the present debate for a new classification of PE in the DSM-V. J Sex Med 2008;5:1079-87. [Crossref] [PubMed]
- Waldinger MD. History of Premature Ejaculation. In: Jannini EA, McMahon GG, Waldinger ED, editors. Premature Ejaculation: From Etiology to Diagnosis and Treatment. New York: Springer, 2013:5-24.
- Serefoglu EC, Yaman O, Cayan S, et al. Prevalence of the complaint of ejaculating prematurely and the four premature ejaculation syndromes: results from the Turkish Society of Andrology Sexual Health Survey. J Sex Med 2011;8:540-8. [Crossref] [PubMed]