The treatment of erectile dysfunction in patients with neurogenic disease
Introduction
Neurogenic erectile dysfunction (NED) is a traditional classification of erectile dysfunction (ED) encompassing disorders impairing erections via neurologic compromise or dysfunction. The disorders compromising erections may act centrally, peripherally or both. The prevalence of neurogenic ED has been suspected to be between 10% and 19% of all causes of ED (1,2). However, several classically defined neurogenic processes may affect several components of the normal pathway to achieve erection e.g., multiple sclerosis (MS), diabetes mellitus, iatrogenic surgical and spinal cord injury. Each disease state has its own unique characteristics that require acknowledgement to fully understand their effect on ED.
Much of the emphasis on erectile pathophysiology has been placed on penile smooth muscle function and cavernosal hemodynamics. The neuroanatomy and neurophysiology of erection can be characterized but its full extent is poorly understood. Neurologic disease does not always reproducibly affect erections in a uniform manner compared to other types of sexual dysfunction (SD). This offers many obstacles to understanding the role the nervous systems plays in SD and consequently obscures what treatment options readily optimize erections specific to the neurologic insult.
Treatment strategies for ED usually target the corporal smooth muscle to augment its relaxation or replace its function via prosthesis implantation. Nevertheless, to treat ED related to a neurologic disorder, assessments of function and disease related factors are recommended, as ED in these men is often multifactorial in origin.
Neuroanatomy and neurophysiology of erection
A comprehensive understanding of the neural pathways for erection is necessary for assessing whether neurogenic ED exists and how to appropriately address the ED. As stated previously, neurologic disease may affect multiple neural pathways leading to ED, sensation deficits and ejaculatory dysfunction.
Peripheral pathways
Nerves originating in the spinal cord and peripheral ganglia innervate the penis. There are autonomic (parasympathetic and sympathetic), and somatic separate and integrated pathways. The autonomic pathways neurons originate in the spinal cord and peripheral ganglia from the sympathetic and parasympathetic systems, respectively. They merge to form the cavernous nerves that travel alongside the prostate, enter the corpora cavernosa and corpus spongiosum to affect the neurovascular events required for tumescence and detumescence. The somatic nerves send sensory information from the penile skin, glans, and urethra via the dorsal penile nerve and pudendal nerve to the spinal cord. The somatic nerves also initiate contraction of the ischio- and bulbocavernosus muscles.
The sympathetic pathway originates from the 11th thoracic to the 2nd lumbar spinal segments and goes via the white rami to enter the sympathetic chain ganglia. Subsequently nerves travel through the lumbar splanchnic to inferior mesenteric and superior hypogastric nerves to the pelvic plexus. The T10 through T12 segments are most often the origin of sympathetic fibers, and the sympathetic chain ganglia that innervate the penis are located in the sacral and caudal ganglia (3).
Parasympathetic pathways originate from the intermediolateral cell columns of the 2nd, 3rd and 4th sacral spinal cord segments. Preganglionic fibers pass through the pelvic plexus where they coalesce with sympathetic fibers from the superior hypogastric plexus. The cavernous nerves that innervate the penis arise from the portion of the pelvic plexus. The pelvic plexus also contains nerves that innervate the rectum, bladder and urinary sphincter and the nerve projections can be damaged during radical excision of the bladder, prostate and rectum, leading to iatrogenic ED (4).
Induction of erection occurs after stimulation of the cavernous and pelvic nerve plexus. Conversely, stimulation of the sympathetic trunk leads to detumescence. The reflex erectile response requires that the sacral reflex arc remain intact. Tactile and sensory signals are received by the somatic sensory pathways and integrate with parasympathetic nuclei within the sacral spinal cord (S2-4) leading to induction of erection via cholinergic signaling. These reflexogenic erections remain intact with upper motor neuron injuries. Psychogenic erections do not require that the sacral reflex arc remain intact. In a cat models, spinal cord removal below L4/L5 led to absence of a reflexogenic erection but stimulation of the medial preoptic area (MPOA) or placement near a female cat in heat led to erection (5,6). Psychogenic erections occur via induction of central pathways traveling from the brain through the sympathetic chain. Non-penile sensory pathways induced by sight, sound, touch and smell travel through the MPOA to the erection centers within the cord T11-L2, and S2-S4 to induce erections (7). When a sacral lower motor neuron injury is present in men, below T12 these types of erections are more likely to occur (8). Spinal cord lesions above T9 are not associated with psychogenic erections (9). Rigidity of erections is less with psychogenic erections because the thoracolumbar sympathetic outflow may contain a decreased concentration of neurons compared to the parasympathetic outflow from the sacral spinal cord.
Somatic pathways
The somatosensory pathways for erections originate in the penile skin, glans and urethra. Glans afferent sensory free nerve endings are 10-fold more than their corpuscular receptors, and are derived from Aδ and unmyelinated C fibers. The nerve endings coalesce to form the dorsal penile nerve along with other sensory nerve fibers. Through the pudendal nerve they enter the S2-4 nerve roots to terminate on spinal neurons and interneurons. The dorsal nerve is not purely somatic, however. Nerve bundles within the dorsal nerve contain nitric oxide (NO) synthase, found typically in autonomic nerves, and stimulation of the sympathetic chain can leak to evoked potentials from the dorsal nerve and vice versa (10-12).
Somatomotor penile innervation originates in Onuf’s nucleus in the S2-4 spinal segments. These nerves travel to the ischiocavernosus and bulbocavernosus muscles when activated lead to contraction necessary for the rigid-erection phase. Several animal studies show that stimulation of the somatomotor pathways may also be under sympathetic control, and adrenergic stimulation may lead to contraction of these muscles during ejaculation (13,14). Somatomotor spinal reflexes may also be initiated by genital stimulation. For instance, the well-known bulbocavernosus reflex is evidence this reflex exists; however the clinical significance of its absence in the neurological assessment of ED has not been substantiated (15).
Supraspinal centers and pathways
Erections are initiated and maintained via integration of afferent inputs in the supra sacral regions of the central nervous system. Regions of the brain cited to have key roles in the integration of signals include the medial amygdala, MPOA, periaqueductal gray matter, paraventricular nucleus (PVN), and ventral tegmentum among others (16). Studies in animal models, particularly in rats, have been paramount in identifying these key areas of signal integration and control. Electrostimulation of the MPOA, PVN and hippocampus lead to erection and lesions in these areas may prevent erection (17). Marson et al. injected labeled pseudorabies virus into rat corpora cavernosa and traced them to neurons in the spinal cord, brain stem and hypothalamus (18). Stimulation of the rat dorsal nerve led to increased firing in the MPOA not found elsewhere (19). Axonal tracing in animals have shows direct projections from the hypothalamus to the lumbosacral autonomic erection centers. Oxytocin and vasopressin have been identified as central neurotransmitters within the hypothalamic nuclei and may have a role in penile erection (17). These signaling studies identifying key areas of erectile response integration may explain how ED is associated with cerebrovascular accident (CVA), Parkinson’s, epilepsy and MS.
The supraspinal pathways are likely activated via central neural activation during sexual arousal.
Positron emission tomorgraphy (PET), and functional magnetic resonance imaging (fMRI) have led to a greater understanding to which center are activated during arousal. These imaging studies measure increases in cerebral blood flow or changes in cerebral activity on a real-time basis. Studies are performed when male subject are aroused by visual cues (usually sexual explicit photos or videos) and compared to images obtained during exposure to sexually neutral cues differences can be measured. Several studies have identified that the inferior frontal lobes, inferior temporal lobes and insular gyrus, and occipital lobes are involved with processing arousal cues, although each are likely to process different stimuli (20-23).
Central nervous system conditions
Spinal cord injury (SCI)
ED is a common occurrence after SCI, occurring in up to 80% of men, and results from disruption of the nerve pathways essential for erection (24,25). Different degrees of ED may occur depending on the spinal cord level of injury (LOI), extent of lesion and timing from injury. Reflexogenic erections can occur with lesions above L3 or L4 when the erectile spinal reflex arc remains intact. Psychogenic erections can occur with low lesions in the sacral and lumbar spinal cord but may not occur in complete lesions above T9 that can damage sympathetic outflow. Additionally, reflexogenic erections are not likely to occur in the spinal shock period that occurs after the initial cord trauma. Conversely, their occurrence may signal that the period of shock is over (26). Typically SCI affects younger men in their “sexual prime” and ED is associated with decreased quality of life (27).
Cerebrovascular accident (CVA/stroke)
A CVA can occur anywhere through the brain, midbrain, brainstem and spinal cord leading to varying degrees of SD depending on location. A decline in libido, erection and ejaculation are frequent in men who have had a CVA, with a reported prevalence of ED that varies from 17% to 48% (28,29). Right hemispheric infarcts seem to affect erections more so than left-sided ones. The exact effects of CVA on sexual function are complex and multifactorial, as disability, psychological and emotional status can affect sexual function aside from the location of the CVA.
Epilepsy
ED varies in men with seizure disorders, occurring in 3% to 58% of men with epilepsy (30). The cause of ED is likely multifactorial, with neurologic, endocrine, iatrogenic, psychiatric and psychosocial factors leading to varying degrees of ED (31). ED can occur in periods surrounding active seizures (ictal) or in the periods unrelated to seizure activity (post-ictal) as well (32).
Multiple sclerosis (MS)
ED occurs in up to 70% of men with MS, and MS is one of the most prevalent neurological disorders that affect the younger adult population worldwide (33-35). The mean time for SD and ED to develop is about 9 years and is rarely a presenting symptom of MS (36). Men with MS and ED may continue to have nocturnal erections, and psychogenic erections; however, this does not mean they have psychogenic ED but could be an indicator that MS involves the spinal cord (37).
SD in MS can be classified into three categories. Primary SD is due directly due to MS-related neurological deficits, secondary SD is related to physical impairments and symptoms or drugs used for MS treatment, and tertiary SD is due to the psychological, social and cultural problems attributed to MS (38). These classifications are important, and underscore the importance of addressing all the issues leading to SD not just the neurologic impairment.
Parkinson’s disease (PD)
PD is a chronic neurodegenerative disease characterized by “motor” and “non-motor” symptoms that lead to progressive disability. Erectile and SD are “non-motor” symptoms and can occur in 50–69% of males with PD (39-42). Ejaculatory and orgasmic function are also impaired. PD affects the dopaminergic pathways leading to erection and arousal. Dopaminergic therapy for PD can improve ED, and sometimes therapy may lead to hypersexuality (43,44). A comparison of married men with PD to age matched controls with non-neurologic chronic disease such as arthritis did not show any discrepancy in ED rates (45). This suggests that ED in certain groups with PD may occur from disease related factors common in chronic illness, in general.
Multiple system atrophy (MSA)
MSA is a neurodegenerative disease of undetermined etiology, where ED is an early prominent sign occurring in 40% of men at the time of diagnosis (46,47). ED occurs in the majority of patients and the exact cause of it is unknown (48). Like PD, MSA likely affects the dopaminergic pathways within the brain essential for arousal (49). Orthostatic hypotension (OH) as a causal factor has been refuted by evidence that sildenafil can overcome reduced filling pressures, and the ED usually precedes the development of OH (46,49,50). Similar to other neurologic disorders that lead to ED, other disease related factors such as psychosocial stress, the burden of chronic illness, changed appearance, fatigue, decreased fine motor movement of fingers, immobility and diminished self-esteem due to loss of independence may contribute as well (51).
Spina bifida (SB)
SB is a group of developmental abnormalities resulting from neural tube closure defects, and affects less than 1/1,000 live births (52). With appropriate medical and surgical therapy, men with SB have increased life expectancy into adulthood where sexual function becomes an important part of life (53). ED exists in approximately 75% of men with SB and is dependent upon the level of the neurologic lesion (54). The level of the neurologic lesions usually corresponds to sensation and penile sensation indicates pudendal nerve signaling. With absent sacral reflexes ED is variable. Furthermore, Diamond et al. reported that 64% of men with lesions below T10 obtained erections versus 14% with a lesion above T10 (55). It has also been suggested that ED may be underreported due to lack of sexual education even in men without associated cognitive impairment (56).
Peripheral neurologic impairment
ED may also occur for damage to the peripheral nerves from pelvic and prostate surgery, as well as diabetes mellitus. These topics are quite broad, deserve their own discussion and are out of the scope of this review.
Management of neurogenic erectile dysfunction (ED)
PDE5 inhibitors (PDE5i)
The American Urological Association Guideline on the Management of ED states oral PDE5i are considered first line therapy for the treatment of ED, unless contraindicated (57). Sildenafil, the first oral PDE5i, was introduced in 1998 and has revolutionized ED therapy due to its broad applicability, effectiveness and safety profile. PDE5i work by preventing hydrolysis of cGMP by the PDE5 enzyme in the smooth muscle of the corpora cavernosa. cGMP degradation typically leads to smooth muscle contraction and detumescence prevented by PDE5i administration. Two other PDE5i, vardenafil and tadalafil are other PDE5i with different pharmacokinetics, PDE receptor selectivity and side effect profiles.
Oral therapies via the PDE5i sildenafil, vardenafil, and tadalafil have been proven to be generally safe and effective in select NED populations. The majority of the treatment effectiveness data has been generated in the SCI population. Data regarding the use of PDE5i outside of the SCI population is lacking (58). Furthermore, the ED that exists in the population with neurologic disorders is often multifactorial and may be caused by psychogenic, psychosocial, hormonal, medication-related and disability-related factors. A careful evaluation of each patient must be performed to isolate these factors prior to initiating vasoactive therapy.
Spinal cord injury (SCI)
Oral PDE5i remains the first line treatment for NED from SCI. Three of the four PDE5i currently available in the U.S., avanafil excluded, have been investigated in the SCI, and all of the more recent studies have shown improvements in erectile function based on IIEF score compared to placebo when included (59-63). Other studies have also shown significant improvements in the IIEF score when compared to baseline (64-69). Furthermore, treatment efficacy when compared to placebo occurs despite LOI or American Spinal Injury Association (ASIA) score characterizing impairment related to the injury (59,61).
Moemen et al. compared the effectiveness and satisfaction associated with use of several ED therapies including sildenafil alone, intracavernosal injections (ICI) followed by sildenafil after ICI discontinuation and vacuum erections devices (VED) followed by sildenafil therapy after VED discontinuation (60). Seventy percent of men receiving vasoactive medications preferred sildenafil to ICI, even though rigidity was superior in the ICI group. All men using VEDs were dissatisfied with that form of therapy.
The duration of erections is also improved by sildenafil in men with SCI. Gans et al. showed that sildenafil use increased the duration of erections from 8.4 to 10 minutes when compared to baseline. Men using sildenafil were also more confident that they could maintain their erection compared to prior therapies such as VEDs (65).
Soler et al. compared sildenafil to vardenafil and tadalafil (69). Sildenafil was effective in 85% of SCI patients, 74% of the patients on vardenafil and 72% of the patients on tadalafil. Sildenafil was associated with more rigid and longer lasting erections. Additionally, 50 mg of sildenafil was effective in 55% of patients compared to more than 70% of the patients on vardenafil and tadalafil requiring 20 mg for a similar response. Men who used tadalafil were able to achieve erections 24 hours after administration, improving overall satisfaction related to the possible spontaneity of sexual encounters. Del Popolo also evaluated the time/duration effectiveness of PDE5i sildenafil 50 mg versus tadalafil 10 mg (64). Tadalafil 10 mg significantly increased the percentage of successful intercourse attempts at 12–24 hours compared with sildenafil. One can suspect that vardenafil, which has a longer half-life than sildenafil, could offer a similar benefit but a study investigating this occurrence has yet to be performed.
Sildenafil use has led to increased patient satisfaction and partner satisfaction after initiating therapy (67). Sánchez Ramos et al. showed that 88.2% of patients, and 85% of partners reported significantly improved sexual satisfaction and overall satisfaction regardless of pretreatment degree of ED or LOI.
Several pre-treatment factors have been described that may indicate success with PDE5i therapy. The presence of an upper motor neuron lesion up to T12 suggests a successful response, as well as requirement for a lower dosage of medication (62,68-71). Additionally, the presence of residual erections after injury or an incomplete SCI (ASI-A vs. ASIB-D) also improve the chance of PDE5i treatment success (59,67,68,71).
Adverse effects related to PDE5i use with mild-moderate and transient (58). Furthermore, side effects usually attenuate if use is not discontinued. Autonomic dysreflexia, a life-threatening phenomenon characterized by bradycardia, hypertension, facial flushing and headaches associated with SCI lesions above T6, has not been reported with use. However, hypotension leading to dizziness in individuals treated with sildenafil has been noted with high thoracic and cervical levels of injury (72). No adverse events were noted within the study; however, the dizziness was reported by use of sildenafil 50 mg in the cervical LOI and 100 mg in the thoracic LOI patients. Headache is the most reported side effect of all PDE5i, followed by dyspepsia and flushing. Priapism, and death have not been reported after use of PDE5i by SCI patients.
Ultimately, PDE5i have had a significant impact on the treatment of ED in men with SCI. The ease of use and tolerability of the medication has also led to improved satisfaction and quality of life that had been previously affected by SD. Head to head trials evaluating specific PDE5i within the SCI population are required to further elucidate drug preference. PDE5i should be considered first line therapy, however men with high thoracic and cervical lesions should be warned about an increased chance of dizziness with sildenafil and possibly other PDE5i use.
Parkinson’s disease (PD)
PDE5i use in PD has not been well studied; however its benefits have been shown. Raffaele performed an open label, prospective study evaluating the efficacy of sildenafil 50 mg on demand and depressive symptoms experienced by the PD patient (73). Erections were improved in approximately 85% of men and 75% noted improvements in their depressive symptoms as well. Sildenafil was well tolerated without significant side effects. Zesiewicz et al., performed a shorter study showing improvements in erectile function but no change in depression and parkinsonisms after ED treatment (74).
Iatrogenic hypotension can occur in men in neurodegenerative disease using sildenafil (49). Hussain et al. placed men with PD and MSA on sildenafil and recorded blood pressure before and after. Half of the 12 MSA patients developed postural hypotension, while none of the twelve PD patients did. Since MSA can be difficult to distinguished diagnostically from PD, baseline blood pressure measurements prior to prescribing the medication and seeking medical assistance if symptomatic hypotension occurred was recommended for all patients with PD, and MSA. Of note, none of the men with MSA who developed hypotension discontinued sildenafil use due to its effectiveness at improving their erections.
Multiple sclerosis (MS)
PDE5i for ED in patients with MS can be considered as reasonably effective and safe. Fowler et al. performed a randomized, multicenter, double-blind, flexible dose trial with open label extensions comparing sildenafil to placebo (75). A nearly 4-fold increase in effective erections was noted in the treatment arm, 96% vs. 24%. Sexual satisfaction and overall satisfaction were also improved in the treatment group based on IIEF scores, and quality of life assessments. Lombardi et al. evaluated tadalafil use in men with MS (71). Seventy eight percent of the men responded with improved erections, better quality of life with regards to sexual function, partner relationship and family life. Just less than half the men who responded to the tadalafil did so at the lower dosage of 10 mg. Subjects in either studies did not have any significant adverse side effects beyond flushing, and headache with PDE5i use.
Spina bifida (SB)
One study by Palmer and colleagues evaluated sildenafil use in SB males with thoracic lesions (76). A prospective, blinded, randomized, placebo-controlled, dose-escalation, crossover study in 17 patients with SB and ED was performed. All study participates took sets of tablet in groups, two sets of placebo, one of 25 mg, and the last 50 mg. Overall response to the tablet sets was measured by IIEF response and self-report of erectile rigidity. Patients reported that taking 50 mg of sildenafil led to improved erections, duration of erections, frequency of erections and level of confidence compared to sildenafil 25 mg and more significantly compared to placebo. Of the five patients who reported side effects, two experienced mild hematological changes that reverted to baseline after study completion.
Epilepsy
Sildenafil has been previously suggested as a treatment option for ED in men with epilepsy (77,78). However, Matos et al. warned that PDE5i are potentially pro-convulsant and should be used with great caution in men with epilepsy (79). Animal studies in rat and mice overwhelmingly suggest PDE5i can reduce seizure threshold. In human trials, seizures were rare but reported. PDE5i exerted their proconvulsive effect by lower seizure threshold possibly by worsening sleep or obstructive sleep apnea, causing cardiovascular changes, or leading to EEG changes specifically with tadalafil use.
Apomorphine
Apomorphine is a non-selective D1/D2 receptor agonist with moderate efficacy and good tolerability in the treatment of mild ED (80). Apomorphine can be administered via subcutaneous injection or sublingually. However, studies have shows a lower efficacy for apomorphine compared to oral sildenafil (81,82). Apomorphine has a set role in the management of PD for non-motor symptoms, and has been reported to cause spontaneous erections and possible hypersexuality in PD men (83,84). Its role in the management of ED has been postulated for men with PD but should be considered as an alternative to sildenafil.
Local therapies
Intracavernosal injections (ICI)
Intracavenosal therapy involves injection of a vasoactive agent into the corpora cavernosa to effect smooth muscle relaxation and tumescence.
In 1983, Brindley injected the corpora of several SCI men with phentolamine (85). Two out of the three men had a sufficient erection produced. Since then multiple reports on the efficacy of intracavernosal therapy have been published using, phentolamine, papaverine, prostaglandin, vasoactive intestinal peptide (VIP), and these medications in combination (86-90). These medications have been found to be extremely effective for neurogenic ED due to their ability act locally and essentially bypassing neuronal pathways. Local therapies are usually considered second-line after PDE5i fail to elicit a desired response which can occur in about 25–30% of men with ED, in general (91). Furthermore, the locally delivered medications can be quite dangerous if not used appropriately as priapism and significant pain with injections can occur. These specific occurrences have been suggested as a reason for high discontinuation rates with intracavernosal therapy (92).
Papaverine
Papaverine is an opium alkaloid that acts as a non-specific PDEi that increases intracellular cAMP and cGMP leading corporal smooth muscle relaxation (93). Intracavernosal papaverine injection was the first clinically effective pharmacological therapy for ED and led to a full erection in at least half of the patient in early studies (94,95).
Alprostodil/prostoglandin E1
Alprostadil is a potent vasodilator and smooth muscle relaxant identical to the naturally occurring PGE1. PGE1 binds with specific receptors on smooth muscle cells and activates intracellular adenylate cyclase to produce cAMP, which in turn induces tissue relaxation through a second messenger system (96). PGE1 is the only FDA approved form of intracavernosal therapy and is available commercailly as EDEX, or Caverject. Its efficacy was demonstrated in several clinical trials where the rate of responders ranged from 40% to 80% (97,98). The most common adverse event is penile pain, which is not related to the injection of the medication itself. In men with prolonged use the pain is usually self-limited (99).
Vasoactive intestinal peptide (VIP)
VIP is a neurotransmitter with regulatory actions on blood flow, secretion and muscle tone with intracorporal adenylate cyclase activation and smooth muscle relaxation. VIP has been shown to elevate cAMP intracellular concentrations without affecting cGMP levels. However, when VIP is given alone it may not induce erection and requires combination with phentolamine or papaverine for it to be effective (88). Common associated adverse effects were facial flushing and headache. VIP in combination with phentolamine is currently being used in the UK and Europe and is seeking regulatory approval for use in the United States.
Phentolamine
Phentolamine blocks post synaptic adrenergic α1 receptors preventing smooth muscle contraction. However, it also may interfere with prejunctional α2 receptors, which may counteract the process (100). Consequently, this may be a reason phentolamine is not prescribed as monotherapy, and frequently is combined with papaverine, alprostadil or VIP.
Combination therapy
Multiple combinations of intracavernosal therapy exist and the effectiveness of them varies based on patient characteristics and varying dosing strength (Table 1). Combination therapy have been extremely effective in the SCI population, and have several advantages including a reduction in cost per dose and side effects base on the lowered dose of each component (101,102). Effectiveness of combination therapy in the spinal cord population is well established, but no specific dose recommendations can be made based on the data (103-106). The use of combination therapy on other forms of neurogenic ED have not been well studied, but there use can be trialed as second-line therapy, or for populations were the side effects of PDE5i may preclude use such as in MSA due to hypotension.
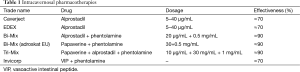
Full table
Intraurethral alprostadil
Alprostadil may be delivered via the urethra in the form of a pellet (MUSE) (107). This form of therapy has been trialed in SCI men with intermediate success (108). Bodner trialed MUSE dose escalation in SCI men and found 1,000 μg to be the most effective dose. Several men had hypotension when a constriction ring was not used in conjunction with the MUSE therapy.
Vacuum erection devices (VED)
VED involved placing the penis in a clear plastic tube where negative pressure created by the vacuum pump leads to penile engorgement and tumescence. Usually a constriction ring can be placed on the base of penis following penile engorgement. Some men complain of bruising, a “cold” penis and pain associated with the constriction ring; however, in some men with NED sensation may not be intact mitigating the side effects of VEDs. VEDs have reported effectiveness up to 90% in certain ED populations and it remains a non-invasive means to achieve and erection.
Chancellor et al. (109) compared VEDs with papaverine injections in 18 males with SCI. The injections and pumps were equally effective in inducing erections and no adverse effects from the treatments were reported. Treatment arms were crossed over, subsequently seven men chose the VED and seven men chose the papavarine highlighting equal efficacy in this population. In another treatment arm topical minoxidil was applied without any effective erections achieved by the study subjects.
VEDs in general have great success in the neurogenic population. Limitations that may affect use are limited manual dexterity, cost due to non-insurance coverage, lack of spontaneity, artificiality of erection, obesity/buried penis, and anticoagulant use.
Penile implant surgery
Prior to the introduction of PDE5i in 1998, intracavernosal vasoactive medications and penile implant surgery were the mainstays of treatment. Penile implant surgery involves placement of inflatable or malleable rods within the corpora cavernosa to provide rigidity for intercourse. Choice of which implant to place usually depends upon manual dexterity and function of the patient, patient anatomy, physician preference and surgical approach.
Zerman et al. performed penile implant surgery in 245 men with neurolgic impairment caused by spinal cord injury, CNS neoplasm, CNS infection, MS and SB (110). Mean follow-up time of 7.2 years was achieved in 195 patients, 50 patients were excluded for lost to follow-up or death from nonurological causes. Interestingly, 135 patients underwent penile implantation to assist with management of urinary incontinence and improve ability for condom/intermittent catheterization. Ninety-two patients patient underwent implantation for ED. Eighty two percent of patients were satisfied with implantation for ED, and 67% of partners were satisfied. Complications included infection (5%), perforation (0–18%), and technical dysfunction (7–33%). Perforation rates were high with the malleable device when it was placed through a subcoronal incision. After adopting an infrapubic approach the perforation rates dropped substantially.
Future directions
Since the advent of PDE5i, many other selective and non-selective peripheral acting compounds have been developed or are in development. Avanafil has shown promising results in treating ED in post-prostatectomy patients with suspected cavernous nerve injury (111). Other PDE5i marked in Asia such as udenafil, and mirodenafil also effective at treating ED may minimize side effects due to shorter half-lives (112-114). Soluable guanylate-cyclase inhibitors and potassium channel activators are compounds that have induced erections in animal models but remain experimental requiring further investigation (115-117).
Centrally active compounds such as apomorphine have been used in men with ED whose cardiovascular comorbidity may prohibit PDE5i use, or in men who have concurrent apomorphine use for its anti-parkinsonian properties. Unfortunately, its side effect profile and poor effectiveness compared to other ED treatments have impaired its mainstream utilization (118). It is suspected that the side effects of apomorphine relate to its D2 receptor affinity. D4 receptor agonists, such as ABT-724 and azulenylmethylpiperazines, may not have the same associated side effects and show potent pro-erectile effects in animal models compared to apomorphine (32,119).
Melanocortin receptor agonists were found to induce erections serendipitously. A study investigating the dermatologic use of Melanotan-II (MT-II) was found to generate erections unexpectedly leading to the development of MTII derivatives for ED treatment (120). MT-II was initially used to induce pigment changes in the skin for artificial tanning but has been suspected to induce melanoma, however (121).
Finally, gene therapy and stem cell research has widened the frontier of ED treatment proposed as possibility to even reverse ED. Specifically, gene therapy pertains to repairing the cause of ED by restoring defective gene function and/or altering the expression of the mutant gene (32). Most of the available data on gene therapy are in the animal model. However, a phase I clinical trial in men with ED undergoing intracavernous injection with a DNA plasmid carrying the alpha-subunit of the corporal smooth muscle Maxi-K channel showed promise in increased erectile function based on IIEF assessment sustained throughout the 3-month study period (122).
Recently, several advances in the uses of stem cells have bet met with great anticipation. Stem cells have the ability to differentiate into different cell lines based on the cellular signaling they receive. Bone marrow mononuclear cells in particular have been used for the treatment of ED in animal models. Yiou et al. recently delivered bone marrow-mononuclear cells (BM-MNC) into the intracavernous smooth muscle of post radical prostatectomy men (123). The open label, dose escalation phase I/II trial showed improvements in IIEF-15 assessment as well as increased vascularization of the corpora based on penile Doppler arterial velocity measurements. Although promising, further investigation in humans is required to substantiate BM-MNCs impact on erections, and erectile function recovery going forward.
Conclusions
Clearly, PDE5i have revolutionized the treatment of ED in general and the neurogenic ED population is no exception. They remain safe and effective in most men with neurogenic ED; however, care must be taken in prescribing PDE5i to men high spinal cord lesions, MSA or possibly PD. VEDs are minimally-invasive and can be as effective as other modalities at leading to erection. However, high discontinuation rates are associated with VED use related to pain, difficulty using the device or cold penis. Intracavernosal therapy has been a mainstay of treatment for neurogenic ED and remains extremely successful in the SCI population. Trial of intracavernosal therapy for other causes of neurogenic ED can be considered second-line therapy, but there is a relative paucity of data for clinical outcomes related to its use outside of SCI men. Surgical therapy via penile implantation remains another second line approach and may also be utilized to assist men with bladder management. Higher complication rates of infections, and perforation have been reported compared to neurologically intact men. Many other compounds are currently being evaluated for the treatment of neurogenic ED as well as gene and stem cell therapy, but still should be considered investigational until substantiated by randomized controlled trials.
Neurogenic ED remains difficult to diagnose and treat effectively. It is important to realize that many men with neurologic disorders may have ED related to disease related factors separate from the insult to the neuro-erectile pathway. These disease related factors must be addressed prior or simultaneously with pharmacologic and/or surgical therapy to effectively treat their SD. As awareness of the complexities of normal sexual function increase so will the recognition of SD in this population. This movement will lead to improved quality of life in men with neurologic disorders, as proven by the strong link between sexual function and quality of life.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abicht JH. Testing the autonomic system. In: Jonas U, Thon WF, Stief CG, editors. Erectile Dysfunction. Berlin: Springer Verlag, 1991:187-94.
- Aboseif S, Shinohara K, Borirakchanyavat S, et al. The effect of cryosurgical ablation of the prostate on erectile function. Br J Urol 1997;80:918-22. [PubMed]
- De Groat WC, Booth AM. Neural control of penile erection. In: Maggi CA, editor. The autonomic nervous system. Switzerland: Harwood Academic Publishers, 1993:467-524.
- Walsh PC, Brendler CB, Chang T, et al. Preservation of sexual function in men during radical pelvic surgery. Md Med J 1990;39:389-93. [PubMed]
- Courtois FJ, Macdougall JC, Sachs BD. Erectile mechanism in paraplegia. Physiol Behav 1993;53:721-6. [PubMed]
- Root WS, Bard P. The mediation of feline erection through sympathetic pathways with some remarks on sexual behavior after deafferentation of the genitalia. Am J Physiol 1947;151:80-90. [PubMed]
- Fazio L, Brock G. Erectile dysfunction: management update. CMAJ 2004;170:1429-37. [PubMed]
- Bors E, Comarr AE. Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv 1960;10:191-222.
- Chapelle PA, Durand J, Lacert P. Penile erection following complete spinal cord injury in man. Br J Urol 1980;52:216-9. [PubMed]
- Burnett AL, Tillman SL, Chang TS, et al. Immunohistochemical localization of nitric oxide synthase in the autonomic innervation of the human penis. J Urol 1993;150:73-6. [PubMed]
- Carrier S, Zvara P, Nunes L, et al. Regeneration of nitric oxide synthase-containing nerves after cavernous nerve neurotomy in the rat. J Urol 1995;153:1722-7. [PubMed]
- Giuliano F, Rampin O, Jardin A, et al. Electrophysiological study of relations between the dorsal nerve of the penis and the lumbar sympathetic chain in the rat. J Urol 1993;150:1960-4. [PubMed]
- Marson L, McKenna KE. CNS cell groups involved in the control of the ischiocavernosus and bulbospongiosus muscles: a transneuronal tracing study using pseudorabies virus. J Comp Neurol 1996;374:161-79. [PubMed]
- Tang Y, Rampin O, Calas A, et al. Oxytocinergic and serotonergic innervation of identified lumbosacral nuclei controlling penile erection in the male rat. Neuroscience 1998;82:241-54. [PubMed]
- Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol Clin North Am 2005;32:379-95. v. [PubMed]
- Giuliano FA, Rampin O, Benoit G, et al. Neural control of penile erection. Urol Clin North Am 1995;22:747-66. [PubMed]
- Meisel RL, Sachs BD. The physiology of male sexual behavior. Physiol Reprod 1994;2:3-105.
- Marson L, Platt KB, McKenna KE. Central nervous system innervation of the penis as revealed by the transneuronal transport of pseudorabies virus. Neuroscience 1993;55:263-80. [PubMed]
- Mallick HN, Manchanda SK, Kumar VM. Sensory modulation of the medial preoptic area neuronal activity by dorsal penile nerve stimulation in rats. J Urol 1994;151:759-62. [PubMed]
- Bocher M, Chisin R, Parag Y, et al. Cerebral activation associated with sexual arousal in response to a pornographic clip: A 15O-H2O PET study in heterosexual men. Neuroimage 2001;14:105-17. [PubMed]
- Mouras H, Stoléru S, Bittoun J, et al. Brain processing of visual sexual stimuli in healthy men: a functional magnetic resonance imaging study. Neuroimage 2003;20:855-69. [PubMed]
- Park K, Seo JJ, Kang HK, et al. A new potential of blood oxygenation level dependent (BOLD) functional MRI for evaluating cerebral centers of penile erection. Int J Impot Res 2001;13:73-81. [PubMed]
- Stoléru S, Grégoire MC, Gérard D, et al. Neuroanatomical correlates of visually evoked sexual arousal in human males. Arch Sex Behav 1999;28:1-21. [PubMed]
- Courtois FJ, Charvier KF, Leriche A, et al. Sexual function in spinal cord injury men. I. Assessing sexual capability. Paraplegia 1993;31:771-84. [PubMed]
- Stien R. Sexual dysfunction in men with spinal injuries. Tidsskr Nor Laegeforen 2008;128:453-6. [PubMed]
- Bedbrook GM. The care and management of spinal cord injuries. Springer Science & Business Media, 2013.
- Anderson KD, Borisoff JF, Johnson RD, et al. The impact of spinal cord injury on sexual function: concerns of the general population. Spinal Cord 2007;45:328-37. [PubMed]
- Kimura M, Murata Y, Shimoda K, et al. Sexual dysfunction following stroke. Compr Psychiatry 2001;42:217-22. [PubMed]
- Bener A, Al-Hamaq AO, Kamran S, et al. Prevalence of erectile dysfunction in male stroke patients, and associated co-morbidities and risk factors. Int Urol Nephrol 2008;40:701-8. [PubMed]
- Smaldone M, Sukkarieh T, Reda A, et al. Epilepsy and erectile dysfunction: a review. Seizure 2004;13:453-9. [PubMed]
- Lambert MV. Seizures, hormones and sexuality. Seizure 2001;10:319-40. [PubMed]
- Calabro RS, Polimeni G, Bramanti P. Recent advances in the treatment of neurogenic erectile dysfunction. Recent Pat CNS Drug Discov 2014;9:41-53. [PubMed]
- Kirkeby HJ, Poulsen EU, Petersen T, et al. Erectile dysfunction in multiple sclerosis. Neurology 1988;38:1366-71. [PubMed]
- Valleroy ML, Kraft GH. Sexual dysfunction in multiple sclerosis. Arch Phys Med Rehabil 1984;65:125-8. [PubMed]
- Zorzon M, Zivadinov R, Monti Bragadin L, et al. Sexual dysfunction in multiple sclerosis: a 2-year follow-up study. J Neurol Sci 2001;187:1-5. [PubMed]
- Betts CD, Jones SJ, Fowler CG, et al. Erectile dysfunction in multiple sclerosis. Associated neurological and neurophysiological deficits, and treatment of the condition. Brain 1994;117:1303-10. [PubMed]
- Frohman EM. Multiple sclerosis, other myelopathies and spinal cord injury. In: Fowler CJ, editor. Neurologic Bladder, Bowel and Sexual Dysfunction. 1st ed. Elsevier, 2001:51-62.
- Foley FW, LaRocca NG, Sanders AS, et al. Rehabilitation of intimacy and sexual dysfunction in couples with multiple sclerosis. Mult Scler 2001;7:417-21. [PubMed]
- Singer C, Weiner WJ, Sanchez-Ramos JR, et al. Sexual Dysfunction in Men with Parkinson's Disease. Neurorehabil Neural Repair 1989;3:199-204.
- Bronner G, Royter V, Korczyn AD, et al. Sexual dysfunction in Parkinson's disease. J Sex Marital Ther 2004;30:95-105. [PubMed]
- Wermuth L, Stenager E. Sexual problems in young patients with Parkinson's disease. Acta Neurol Scand 1995;91:453-5. [PubMed]
- Koller WC, Vetere-Overfield B, Williamson A, et al. Sexual dysfunction in Parkinson's disease. Clin Neuropharmacol 1990;13:461-3. [PubMed]
- Bronner G, Vodušek DB. Management of sexual dysfunction in Parkinson's disease. Ther Adv Neurol Disord 2011;4:375-83. [PubMed]
- Weintraub D, Siderowf AD, Potenza MN, et al. Association of dopamine agonist use with impulse control disorders in Parkinson disease. Arch Neurol 2006;63:969-73. [PubMed]
- Lipe H, Longstreth WT Jr, Bird TD, et al. Sexual function in married men with Parkinson's disease compared to married men with arthritis. Neurology 1990;40:1347-9. [PubMed]
- Kirchhof K, Apostolidis AN, Mathias CJ, et al. Erectile and urinary dysfunction may be the presenting features in patients with multiple system atrophy: a retrospective study. Int J Impot Res 2003;15:293-8. [PubMed]
- Beck RO, Betts CD, Fowler CJ. Genitourinary dysfunction in multiple system atrophy: clinical features and treatment in 62 cases. J Urol 1994;151:1336-41. [PubMed]
- Papatsoris AG, Papapetropoulos S, Singer C, et al. Urinary and erectile dysfunction in multiple system atrophy (MSA). Neurourol Urodyn 2008;27:22-7. [PubMed]
- Hussain IF, Brady CM, Swinn MJ, et al. Treatment of erectile dysfunction with sildenafil citrate (Viagra) in parkinsonism due to Parkinson's disease or multiple system atrophy with observations on orthostatic hypotension. J Neurol Neurosurg Psychiatry 2001;71:371-4. [PubMed]
- Wenning GK, Scherfler C, Granata R, et al. Time course of symptomatic orthostatic hypotension and urinary incontinence in patients with postmortem confirmed parkinsonian syndromes: a clinicopathological study. J Neurol Neurosurg Psychiatry 1999;67:620-3. [PubMed]
- Basson R. Sexuality and parkinson's disease. Parkinsonism Relat Disord 1996;2:177-85. [PubMed]
- Yen IH, Khoury MJ, Erickson JD, et al. The changing epidemiology of neural tube defects. United States, 1968-1989. Am J Dis Child 1992;146:857-61. [PubMed]
- Bowman RM, McLone DG, Grant JA, et al. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg 2001;34:114-20. [PubMed]
- Gamé X, Moscovici J, Gamé L, et al. Evaluation of sexual function in young men with spina bifida and myelomeningocele using the International Index of Erectile Function. Urology 2006;67:566-70. [PubMed]
- Diamond DA, Rickwood AM, Thomas DG. Penile erections in myelomeningocele patients. Br J Urol 1986;58:434-5. [PubMed]
- Decter RM, Furness PD 3rd, Nguyen TA, et al. Reproductive understanding, sexual functioning and testosterone levels in men with spina bifida. J Urol 1997;157:1466-8. [PubMed]
- Montague DK, Jarow JP, Broderick GA, et al. Chapter 1: The management of erectile dysfunction: an AUA update. J Urol 2005;174:230-9. [PubMed]
- Lombardi G, Nelli F, Celso M, et al. Treating erectile dysfunction and central neurological diseases with oral phosphodiesterase type 5 inhibitors. Review of the literature. J Sex Med 2012;9:970-85. [PubMed]
- Ergin S, Gunduz B, Ugurlu H, et al. A placebo-controlled, multicenter, randomized, double-blind, flexible-dose, two-way crossover study to evaluate the efficacy and safety of sildenafil in men with traumatic spinal cord injury and erectile dysfunction. J Spinal Cord Med 2008;31:522-31. [PubMed]
- Moemen MN, Fahmy I, AbdelAal M, et al. Erectile dysfunction in spinal cord-injured men: different treatment options. Int J Impot Res 2008;20:181-7. [PubMed]
- Giuliano F, Sanchez-Ramos A, Löchner-Ernst D, et al. Efficacy and safety of tadalafil in men with erectile dysfunction following spinal cord injury. Arch Neurol 2007;64:1584-92. [PubMed]
- Giuliano F, Hultling C, El Masry WS, et al. Randomized trial of sildenafil for the treatment of erectile dysfunction in spinal cord injury. Sildenafil Study Group. Ann Neurol 1999;46:15-21. [PubMed]
- Giuliano F, Rubio-Aurioles E, Kennelly M, et al. Efficacy and safety of vardenafil in men with erectile dysfunction caused by spinal cord injury. Neurology 2006;66:210-6. [PubMed]
- Del Popolo G, Li Marzi V, Mondaini N, et al. Time/duration effectiveness of sildenafil versus tadalafil in the treatment of erectile dysfunction in male spinal cord-injured patients. Spinal Cord 2004;42:643-8. [PubMed]
- Gans WH, Zaslau S, Wheeler S, et al. Efficacy and safety of oral sildenafil in men with erectile dysfunction and spinal cord injury. J Spinal Cord Med 2001;24:35-40. [PubMed]
- Hultling C, Giuliano F, Quirk F, et al. Quality of life in patients with spinal cord injury receiving Viagra (sildenafil citrate) for the treatment of erectile dysfunction. Spinal Cord 2000;38:363-70. [PubMed]
- Sánchez Ramos A, Vidal J, Jáuregui ML, et al. Efficacy, safety and predictive factors of therapeutic success with sildenafil for erectile dysfunction in patients with different spinal cord injuries. Spinal Cord 2001;39:637-43. [PubMed]
- Lombardi G, Macchiarella A, Cecconi F, et al. Ten-year follow-up of sildenafil use in spinal cord-injured patients with erectile dysfunction. J Sex Med 2009;6:3449-57. [PubMed]
- Soler JM, Previnaire JG, Denys P, et al. Phosphodiesterase inhibitors in the treatment of erectile dysfunction in spinal cord-injured men. Spinal Cord 2007;45:169-73. [PubMed]
- Khorrami MH, Javid A, Moshtaghi D, et al. Sildenafil efficacy in erectile dysfunction secondary to spinal cord injury depends on the level of cord injuries. Int J Androl 2010;33:861-4. [PubMed]
- Lombardi G, Macchiarella A, Cecconi F, et al. Efficacy and safety of medium and long-term tadalafil use in spinal cord patients with erectile dysfunction. J Sex Med 2009;6:535-43. [PubMed]
- Ethans KD, Casey AR, Schryvers OI, et al. The effects of sildenafil on the cardiovascular response in men with spinal cord injury at or above the sixth thoracic level. J Spinal Cord Med 2003;26:222-6. [PubMed]
- Raffaele R, Vecchio I, Giammusso B, et al. Efficacy and safety of fixed-dose oral sildenafil in the treatment of sexual dysfunction in depressed patients with idiopathic Parkinson's disease. Eur Urol 2002;41:382-6. [PubMed]
- Zesiewicz TA, Helal M, Hauser RA. Sildenafil citrate (Viagra) for the treatment of erectile dysfunction in men with Parkinson's disease. Mov Disord 2000;15:305-8. [PubMed]
- Fowler CJ, Miller JR, Sharief MK, et al. A double blind, randomised study of sildenafil citrate for erectile dysfunction in men with multiple sclerosis. J Neurol Neurosurg Psychiatry 2005;76:700-5. [PubMed]
- Palmer JS, Kaplan WE, Firlit CF. Erectile dysfunction in patients with spina bifida is a treatable condition. J Urol 2000;164:958-61. [PubMed]
- Harden CL. Treatment of sexual disorders in people with epilepsy. Epilepsy Behav 2002;3:38-41. [PubMed]
- Montouris G, Morris GL 3rd. Reproductive and sexual dysfunction in men with epilepsy. Epilepsy Behav 2005;7 Suppl 2:S7-14. [PubMed]
- Matos G, Scorza FA, Cavalheiro EA, et al. PDEI-5 for erectile dysfunction: a potential role in seizure susceptibility. J Sex Med 2012;9:2111-21. [PubMed]
- Heaton JP, Morales A, Adams MA, et al. Recovery of erectile function by the oral administration of apomorphine. Urology 1995;45:200-6. [PubMed]
- Eardley I, Wright P, MacDonagh R, et al. An open-label, randomized, flexible-dose, crossover study to assess the comparative efficacy and safety of sildenafil citrate and apomorphine hydrochloride in men with erectile dysfunction. BJU Int 2004;93:1271-5. [PubMed]
- Perimenis P, Gyftopoulos K, Giannitsas K, et al. A comparative, crossover study of the efficacy and safety of sildenafil and apomorphine in men with evidence of arteriogenic erectile dysfunction. Int J Impot Res 2004;16:2-7. [PubMed]
- Chaudhuri KR, Schapira AH. Non-motor symptoms of Parkinson's disease: dopaminergic pathophysiology and treatment. Lancet Neurol 2009;8:464-74. [PubMed]
- O'Sullivan JD, Hughes AJ. Apomorphine-induced penile erections in Parkinson's disease. Mov Disord 1998;13:536-9. [PubMed]
- Brindley GS. Cavernosal alpha-blockade: a new technique for investigating and treating erectile impotence. Br J Psychiatry 1983;143:332-7. [PubMed]
- Vidal J, Curcoll L, Roig T, et al. Intracavernous pharmacotherapy for management of erectile dysfunction in multiple sclerosis patients. Rev Neurol 1995;23:269-71. [PubMed]
- Kapoor VK, Chahal AS, Jyoti SP, et al. Intracavernous papaverine for impotence in spinal cord injured patients. Paraplegia 1993;31:675-7. [PubMed]
- Dinsmore WW, Wyllie MG. Vasoactive intestinal polypeptide/phentolamine for intracavernosal injection in erectile dysfunction. BJU Int 2008;102:933-7. [PubMed]
- Hirsch IH, Smith RL, Chancellor MB, et al. Use of intracavernous injection of prostaglandin E1 for neuropathic erectile dysfunction. Paraplegia 1994;32:661-4. [PubMed]
- Bodner DR, Lindan R, Leffler E, et al. The application of intracavernous injection of vasoactive medications for erection in men with spinal cord injury. J Urol 1987;138:310-1. [PubMed]
- Eardley I, Donatucci C, Corbin J, et al. Pharmacotherapy for erectile dysfunction. J Sex Med 2010;7:524-40. [PubMed]
- Coombs PG, Heck M, Guhring P, et al. A review of outcomes of an intracavernosal injection therapy programme. BJU Int 2012;110:1787-91. [PubMed]
- Pöch G, Kukovetz WR. Papaverine-induced inhibition of phosphodiesterase activity in various mammalian tissues. Life Sci I 1971;10:133-44. [PubMed]
- Fallon B. Intracavernous injection therapy for male erectile dysfunction. Urol Clin North Am 1995;22:833-45. [PubMed]
- Goldstein I, Payton T, Padma-Nathan H. Therapeutic roles of intracavernosal papaverine. Cardiovasc Intervent Radiol 1988;11:237-9. [PubMed]
- Palmer LS, Valcic M, Melman A, et al. Characterization of cyclic AMP accumulation in cultured human corpus cavernosum smooth muscle cells. J Urol 1994;152:1308-14. [PubMed]
- Linet OI, Ogrinc FG. Efficacy and safety of intracavernosal alprostadil in men with erectile dysfunction. The Alprostadil Study Group. N Engl J Med 1996;334:873-7. [PubMed]
- Costa P, Potempa AJ. Intraurethral alprostadil for erectile dysfunction: a review of the literature. Drugs 2012;72:2243-54. [PubMed]
- Lakin MM, Montague DK, VanderBrug Medendorp S, et al. Intracavernous injection therapy: analysis of results and complications. J Urol 1990;143:1138-41. [PubMed]
- Wein AJ, Kavoussi LR, Novick AC, et al. Campbell-Walsh Urology. 10th edition. Elsevier Health Sciences, 2011.
- Seyam R, Mohamed K, Akhras AA, et al. A prospective randomized study to optimize the dosage of trimix ingredients and compare its efficacy and safety with prostaglandin E1. Int J Impot Res 2005;17:346-53. [PubMed]
- Deforge D, Blackmer J, Garritty C, et al. Male erectile dysfunction following spinal cord injury: a systematic review. Spinal Cord 2006;44:465-73. [PubMed]
- Beretta G, Zanollo A, Fanciullacci F, et al. Intracavernous injection of papaverine in paraplegic males. Acta Eur Fertil 1986;17:283-4. [PubMed]
- Sidi AA, Cameron JS, Dykstra DD, et al. Vasoactive intracavernous pharmacotherapy for the treatment of erectile impotence in men with spinal cord injury. J Urol 1987;138:539-42. [PubMed]
- Earle CM, Keogh EJ, Ker JK, et al. The role of intracavernosal vasoactive agents to overcome impotence due to spinal cord injury. Paraplegia 1992;30:273-6. [PubMed]
- Tang SF, Chu NK, Wong MK. Intracavernous injection of prostaglandin E1 in spinal cord injured patients with erectile dysfunction. A preliminary report. Paraplegia 1995;33:731-3. [PubMed]
- Hellstrom WJ, Bennett AH, Gesundheit N, et al. A double-blind, placebo-controlled evaluation of the erectile response to transurethral alprostadil. Urology 1996;48:851-6. [PubMed]
- Bodner DR, Haas CA, Krueger B, et al. Intraurethral alprostadil for treatment of erectile dysfunction in patients with spinal cord injury. Urology 1999;53:199-202. [PubMed]
- Chancellor MB, Rivas DA, Panzer DE, et al. Prospective comparison of topical minoxidil to vacuum constriction device and intracorporeal papaverine injection in treatment of erectile dysfunction due to spinal cord injury. Urology 1994;43:365-9. [PubMed]
- Zermann DH, Kutzenberger J, Sauerwein D, et al. Penile prosthetic surgery in neurologically impaired patients: long-term followup. J Urol 2006;175:1041-4; discussion 1044. [PubMed]
- Jung J, Choi S, Cho SH, et al. Tolerability and pharmacokinetics of avanafil, a phosphodiesterase type 5 inhibitor: a single- and multiple-dose, double-blind, randomized, placebo-controlled, dose-escalation study in healthy Korean male volunteers. Clin Ther 2010;32:1178-87. [PubMed]
- Chung JH, Kang DH, Oh CY, et al. Safety and efficacy of once daily administration of 50 mg mirodenafil in patients with erectile dysfunction: a multicenter, double-blind, placebo controlled trial. J Urol 2013;189:1006-13. [PubMed]
- Ding H, Du W, Wang H, et al. Efficacy and safety of udenafil for erectile dysfunction: a meta-analysis of randomized controlled trials. Urology 2012;80:134-9. [PubMed]
- Kim BH, Yi S, Kim J, et al. Influence of alcohol on the hemodynamic effects and pharmacokinetic properties of mirodenafil: a single-dose, randomized-sequence, open-label, crossover study in healthy male volunteers in Korea. Clin Ther 2009;31:1234-43. [PubMed]
- Evgenov OV, Pacher P, Schmidt PM, et al. NO-independent stimulators and activators of soluble guanylate cyclase: discovery and therapeutic potential. Nat Rev Drug Discov 2006;5:755-68. [PubMed]
- Spektor M, Rodriguez R, Rosenbaum RS, et al. Potassium channels and human corporeal smooth muscle cell tone: further evidence of the physiological relevance of the Maxi-K channel subtype to the regulation of human corporeal smooth muscle tone in vitro. J Urol 2002;167:2628-35. [PubMed]
- Mizusawa H, Hedlund P, Brioni JD, et al. Nitric oxide independent activation of guanylate cyclase by YC-1 causes erectile responses in the rat. J Urol 2002;167:2276-81. [PubMed]
- Mulhall JP. Sublingual apomorphine for the treatment of erectile dysfunction. Expert Opin Investig Drugs 2002;11:295-302. [PubMed]
- Sanna F, Succu S, Hübner H, et al. Dopamine D2-like receptor agonists induce penile erection in male rats: differential role of D2, D3 and D4 receptors in the paraventricular nucleus of the hypothalamus. Behav Brain Res 2011;225:169-76. [PubMed]
- Hadley ME, Dorr RT. Melanocortin peptide therapeutics: historical milestones, clinical studies and commercialization. Peptides 2006;27:921-30. [PubMed]
- Paurobally D, Jason F, Dezfoulian B, et al. Melanotan-associated melanoma. Br J Dermatol 2011;164:1403-5. [PubMed]
- Melman A, Bar-Chama N, McCullough A, et al. hMaxi-K gene transfer in males with erectile dysfunction: results of the first human trial. Hum Gene Ther 2006;17:1165-76. [PubMed]
- Yiou R, Hamidou L, Birebent B, et al. Safety of Intracavernous Bone Marrow-Mononuclear Cells for Postradical Prostatectomy Erectile Dysfunction: An Open Dose-Escalation Pilot Study. Eur Urol 2015. [Epub ahead of print]. [PubMed]


