Diagnosis and treatment of benign prostate hyperplasia in Asia
Introduction
Benign prostatic hyperplasia (BPH) is a common disease, not only in Asia but worldwide. The spectrum of disease may vary in differently region, but the basic pathophysiology is the same. To manage the disease, we need to define what it is, before the diagnosis. Management would be according to the basic fundamentals of good clinical practice. That is, whatever we do is for the benefit of the patient that we should manage the patient as a whole, as taught by Professor Jieping Wu, a pioneer of modern Urology in China.
Definition of BPH
Clinical BPH has been defined as benign prostatic enlargement (BPE) (1), but in our practice and clinical observation, many patients with smaller prostates less than 20 grams may still cause obstruction and symptoms. In our study to characterize normal prostate on transabdominal ultrasound (TAUS) on patients who presented with asymptomatic microscopic haematuria who had flexible cystoscopy done, we could find only four normal patients out of 77 patients studied (2). Many patients with small prostate can still have obstruction, if not symptoms due to prostate adenoma, and this may be the cause of the microscopic haematuria. The adenoma causes obstruction by virtual of where it is sited, rather than its size. An adenoma siting at the strategic bladder outlet would cause more obstruction than one sited in the lateral lobe of the prostate. When it arises from the middle and protrudes into the bladder, it forms the classical median lobe obstruction due to the ball valve effect (3). If it is sited beneath the bladder neck, in the subcervical region, it would lift the bladder neck high and causes obstruction. Thus the previously described bladder neck obstruction, in relatively young patients is not due to primary bladder neck pathology, but is essentially a variant of BPH. Bladder neck dyskinesia, as a primary diagnosis is rare.
In transurethral enucleation and resection of prostate, the adenoma can be separated from the false capsule, and often the adenoma coalesces together to form multiple adenomata and cause obstruction. This can be seen on histology of the BPH, which is described as nodular BPH by the pathologist.
The adenoma is essentially similar to that of the fibroadenoma of the breast, except that the prostate is sited at the bladder outlet and causes varying degree of obstruction, and may further progress.
Thus we can define clinical BPH, simply as a prostate adenoma or adenomata, irrespective of size, causing obstruction to the bladder outlet, with or without symptoms.
Diagnosis of BPH
With the above definition, BPH can be diagnosed with some confidence using transabdominal or transrectal ultrasound (TRUS) and estimating the urinary flow rate. TAUS is less invasive than TRUS. In Asian region patients has lower body mass index (BMI) and imaging the prostate with some accuracy is seldom a problem, as in obese patients. TAUS can easily be repeated.
As BPH can present with or without symptoms, therefore relying on the International Prostate Symptoms Score (IPSS) solely, to decide on treatment is not reliable. Digital rectal examination (DRE) is inaccurate; estimation of size is inaccurate especially if big. Further, a seemingly small prostate can also cause obstruction and symptoms. The DRE is mainly to assess the consistency of the prostate to detect possible carcinoma.
Although lower urinary tract symptoms (LUTS) is the commonest presentation of BPH, it is not diagnostic as there are many other causes of LUTS, ranging from bladder dysfunctions due to diabetes and age, neurogenic bladders and urethral strictures. BPH can also present with acute retention of urine (AUR) without previous history of LUTS. In our study on AUR in Singapore, 50% denied any history of LUTS before the acute episode (4). A more serious complication is that of chronic retention of urine which is often seen in less developed part of Asia. This would result in significant obstruction leading to back pressure changes with severe hydronephrosis and chronic renal impairment. In a report from Sri Langka, 30 patients with chronic retention of urine were seen within a period of 1 year, presenting with nocturnal enuresis (5). With the advent of using prostate specific antigen (PSA) as a marker for detecting possible prostate cancer, many asymptomatic patients present with elevated PSA. In a most recent report of TRUS biopsy for elevated PSA in Taiwan, out of 12,968 patients biopsied, 36% of patients were positive (6). Presumably the rest is mainly due to BPH or BPH with chronic prostatitis.
Thus, after taking a detailed history and physical examination, a clinic ultrasound would be useful. In fact, it is essential in the proper diagnosis of BPH to differentiate it from the many other pathologies. The ultrasound machine need not be sophisticated, and often an old machine from the diagnostic radiology would suffice, for the measurement of the size (PV) and shape, looking at the intravesical prostatic protrusion (IPP). It can also be used for estimation of the postvoid residual urine (PVR).
IPP is the distance measured from the inner most tip of the prostate to the base, at the circumference of the bladder, seen on the sagittal view of the prostate ultrasound (3). The measurement is done in patient with a comfortably full bladder (7). Normal prostate with no BPH, is inverted similar to the female bladder neck and the flow rate would also be normal. IPP has 100% specificity and positive predictive value in the diagnosis of BPH (2), Therefore patients with LUTS but no BPH can easily be differentiated in the clinic, and other possible causes of LUTS, such as over active bladder or nocturnal polyuria can then be suspected and managed accordingly.
The urinary flow rate can be determined with the simple uroflow machine. If not available, the average flow rate can be done easily with a measuring jar and using a timing device (the stop watch or the smart phone) which is readily available, even in the remotest part of Asia.
Predicting obstruction and progression of BPH
Patients with IPP can further be graded according to the degree of IPP to predict obstruction. It has been established that the greater the IPP the more the obstruction on pressure flow studies (8). Of 200 patients studied, for grade 1 IPP ≤5 mm, 79% of patients are not obstructed, whereas for grade 3 IPP more than 10 mm, almost 94% of the patients are obstructed urodynamically. IPP has also been found to be a good predictor of success in trial off catheter after episode of AUR in a study of 100 patients (6). For patients with grade 1 IPP, 36% failed trail off, while 67% failed if there is a grade 3 IPP.
As IPP is related to obstruction, it is also related to the progression of the disease BPH. Our studies showed that of 259 patients with a mean follow-up of 32 months, for grade 1 IPP, 6% progressed in terms of the need for surgery and complications. Whereas if it is a grade 3 IPP, 44% of patients will progress (9).
However, patients should not be treated just on the findings of IPP alone, even though with grade 3 IPP, 44% of patients will progress with deterioration of symptoms, increased PVR or retention of urine, 56% of them do not progress. Therefore, for a more balanced decision making, treatment of BPH should be according to the severity of the disease as a whole.
Classifying the severity of BPH
Fundamentally the prostate adenoma (clinical BPH) causes obstruction and symptoms. Obstruction is more important than symptoms, as obstruction if not relieved, would progress and cause organs dysfunctions.
Therefore, the severity of BPH can be classified according to the obstruction and symptoms. The symptoms can be quantified with the IPSS, and the quality of life index (QOL). There is poor co relation between IPSS and obstruction and therefore the symptoms score should not be used as the sole parameter in the decision making on further treatment (10). Also the IPSS is not related to QOL, which depends on patients’ life style and occupation. A retiree with nocturia 4 times may not be bothered while a young executive with a score of nocturia 2 times, may be bothered. Therefore QOL is more important than IPSS in the assessment of symptoms.
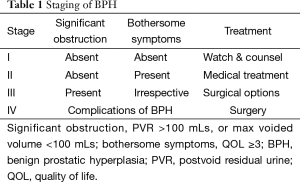
Prostate adenoma (PA) causes varying degree of obstruction. Obstruction would be significant when there is organ dysfunction. The two main functions of the bladder are storage and emptying. When the emptying function is affected patient would develop persistent high residual urine. When the storage function is affected the maximum voided urinary volume would be low, and this can easily be measured. Thus significant obstruction can be defined as when there is persistent residual more than 100 mL and/or maximum voided volume less than 100 mL (10,11). With these cut off and definitions, the severity of BPH can be classified accordingly:
- Stage I would be a patient with no significant obstruction, and no bothersome symptoms;
- Stage II would be a patient with bothersome symptoms but no significant obstruction;
- Stage III would be a patient with significant obstruction, irrespective of symptoms;
- Stage IV would be a patient with complications of BPH such as retention of urine, recurrent gross haematuria, urinary infection and bladder stones formation.
Generally, there is good concordance between the grade and stage of the disease. Stage I patients can be treated conservatively with advised on proper fluid intake and healthy life style. Stage I Grade 1 can be reassured and discharge from follow-up, while the stage I grade 2 or 3 patients need to be followed up at 6 months to 1 year interval as it is predicted that they are more likely to progress. Stage II patients can be treated with medication, while, Stage III grade 3 patients would be advised more aggressive treatment with surgery as an option. Stage IV patients would generally require surgical treatment (Table 1).
Full table
There would be some patients with persistently high residual urine (suspected staged III) but low grade IPP, and these patients would require flexible cystoscopy and/or urodynamics studies to detect hypo active bladder.
For Asian region, it is more practical to have flexible cystoscopies available, rather than investing in the urodynamic set up which is far more expensive and not specific. Often, the pressure flow study would show equivocal obstruction, or in patients with more severe obstruction with no IPP, they would not be able to void, and pressure flow study cannot be done. Some of these patients had been mistakenly treated as for hypocontractile or neuropathic bladder with long-term catheterization. A flexible cystoscopy would help in diagnosing mechanical bladder outlet obstruction in the 21% of patients who are still obstructed in spite of a low IPP (9).
Modalities of treatment
The natural history of BPH is that it is a slow progressive disease. The majority of patients will do well even without any active treatment. In one study on the 5-year follow-up of 107 patients with prostatism, presumably due to BPH, 32% improve, 52% remained stable and only 16% deteriorated and 9% required surgery (12).
These 16% who are going to deteriorate, can now be more confidently identified for more active treatment with our grading and staging of BPH (13). In that study of 408 patients, 59% of patients was treated conservatively, 32% with medications and 9% had TURP done, approximating the natural history closely.
The majority of patients do well or stable even without treatment, therefore conservative management should be the main stay in the treatment of BPH.
Conservative management
This would consist of reassurance and advice on fluid intake and healthy life style, such as regular exercise with walking, qigong, yoga or tai chi. These can help in reducing symptoms for patients with mild BPH, especially the low grade and low stage disease.
The concern of most patients who come to see the family doctor or the urologist, are whether they have cancer or whether they will develop kidney problems. With normal PSA and DRE, prostate cancer is less lightly. If there is no persistent PVR more than 100 mL, most patients could be reassured, even though they may have some LUTS and bothersome symptoms. Advising more fresh fruits and vegetables in the diet and less red meat would be appropriate.
Medical treatment
There are two main groups of medications for treating BPH:
- The alpha blockers which relieve symptoms by blocking the sympathetic nerve endings at the bladder neck. They have not been shown to prevent progression of the disease (14). Therefore alpha blockers should be given only to patients who are bothered by their symptoms and not just symptoms score alone. Most literatures report the efficacy of the medication by the improvement in average reduction in symptom scores. How many patients are actually relieved of their bother, and whether the symptoms returned without the alpha blockers are not reported. It had been shown that patients with high grade IPP do not response as well to alpha blockers (15). This is due probably to the distorted bladder neck. If they are still bothered and developing bladder instability with deteriorating symptoms, surgery should be advised early.
Also patient should be informed of the efficacy of the medication and its possible side effects, that of hypotension, giddiness and possibility of falls. The final decision whether to take the medication or not should be that of the patient.
Patients who opted for the alpha blocker treatment should be given a trial of medication first for not more than 2 to 4 weeks to assess the effectiveness and the side effects. Only if patients are satisfied with the results, then they would be considered for long-term medication. Even then, patients should be advised that they may take the medications on when needed basis. In this way it would be more cost effective. Those patients with high grade IPP 2 to 3 should be followed up more closely at 6 to 12 months to monitor their progression.
For patients with prostate more than 30 to 40 grams, 5 alpha reductase inhibitors (5 ARI’s) can be added. - 5 ARI’s: the two main 5 ARI’s used in Asia are finasteride (proscar) and dutasteride (avodart). They act by preventing the conversion of testosterone to 5 hydroxytestosterone which stimulate the growth of BPH.
They have been shown to be effective only in patients with large prostate more than 40 grams, and not effective in patients with small prostate less than 30 grams, or with PSA less than 1.5 ug/L.
5 ARI’s are expensive, considering the need for long-term treatment. Even though in some Asian countries, the cheaper generic versions are available, the side effects of the drugs are that of sexual dysfunctions with loss of libido and ejaculation failure and erectile dysfunction. Therefore the drug should be prescribed to patients only with large prostate and high stage disease, at risk of developing voiding or storage problems.
5 ARI’s help to reduce the need for surgery for many patients, especially the older patients and those with co morbidities. However, not all patients with large prostate response to the 5 ARI’s as the medication can shrink the size, but cannot alter the shape of the adenoma. In the flow dynamics of obstruction, the middle lobe distorts the flow, while the lateral compress the flow and distortion is more obstructive than compression. So even though the 5 ARI’s may shrink the prostate, it cannot change the shape. Some patients, with protruding lobes may still continue to progress and this may lead to surgical intervention (16).
Surgical treatment
Surgery would ideally restore the prostate to normal shape (normal anatomy) to achieve normal functions. For that the best procedure would be the enucleation of the prostate adenoma/adenomata, be it by open method, laparoscopic or transurethral.
With understanding of the basic pathology, that BPH is not diffused enlargement, but nodular hyperplastic adenoma, to remove the pathology completely should be the goal of any surgical procedure. Incomplete removal would lead to recurrent symptoms and obstruction due to the progression of the residual adenoma.
Because of the irregularity of the adenomata, the problem with conventional TURP is that often, adenomatous tissue is left behind. To remove the tissue completely may lead to resecting too deep, and cause perforation of the false capsule leading to bleeding. To avoid this, varying amount of adenoma would be left behind leading to recurrent problems, often many years later.
Therefore, retrograde enucleation of the adenoma would be the procedure of choice to remove the pathology tissue more completely. Also there would be less bleeding as the perforating vessels are diathermised at source, instead of being resected repeatedly (17).
Holmium laser enucleation of prostate (HoLEP) had been shown to have good long-term results, but for Asian countries, transurethral enucleation and resection of prostate (TUERP) would be more practical and more cost effective. This had been pioneered by Liu et al. in China, with good results (18). No extra instrument is needed. The prostate is enucleated in a retrograde fashion and with the lobe attached at the bladder neck; it can then be rapidly resected. Compared to conventional TURP, TUERP is better, as evidence by the fact that the flow rate is better and that the PSA, as a surrogate measure of prostate volume is statistically less than after TURP (19).
The incidence of post-operative incontinence is higher in the enucleation of prostate but often the incontinence is temporary. With better experience and technique of marking out the distal margin of the apical lobe and preventing tearing of the membranous urethra, the incidence of temporary incontinence can be reduced.
Currently, at the last EAU meeting in Madrid 2015, TURP is still considered as the gold standard for significantly obstructing prostate. The problem with TURP is the retreatment rate of 3-14.5% after 5 years (20) presumably due mainly to recurrent/remnant adenoma.
Apart from recurrent LUTS, another common presentation is that of painless gross haematuria, due to the congested neovascularity on the recurrent/remnant adenomatous tissue.
TUERP would help to reduce this problem.
The vaporization procedure, using various types of laser (KTP green light laser, etc.) and electrodes, though result in less bleeding than TURP, often also leave residual adenoma post procedure, and long-term results are not favorable compared to standard TURP (21).
Thus for Asian countries, TUERP with bipolar resection, using saline would be the way forward for the significantly obstructing prostate.
Comments
Clinic ultrasound is essential in diagnosing BPH.
The machine is also useful for assessing other urological problems such as urinary stone and haematuria and urinary infections. In Asia, an ultrasound machine in the clinic should have priority to the urodynamic unit which is far more expensive.
The phosphodiesterase type 5 inhibitor (PDE 5), tadalafil for medical treatment should be reserved for those who present mainly with erectile dysfunction and LUTS. It is probably effective only for patients with minimal BPH, small gland with minimal protrusion and obstruction.
The anticholinergics for patients with over active bladders, having frequency and urgency should be reserved for patients mainly with bladder problem and minimal BPH, with low grade IPP and low PV. It should be prescribed with caution in patients with high grade IPP as it may result in worsening of PVR and retention of urine.
The aim of surgery should be complete removal of the adenoma to minimized recurrent problem. Less minimally invasive procedures such as transurethral microwave thermotherapy, transurethral needle ablation, do not address the fundamental problem and do not have good long-term results.
Conclusions
BPH can be defined as prostate adenoma causing obstruction and can be diagnosed confidently with non-invasive transabdominal ultrasound in the clinic. The disease can then be graded according to the IPP on TAUS for predicting the obstruction and progression. Treatment can then be tailored to the severity of obstruction and symptoms. In this way, by considering the whole picture, BPH as a common disease, can be treated more cost effectively, avoiding overtreatment and under treatment.
Acknowledgements
The author thanks Dr. John Yuen for valuable suggestions in the scripts.
Funding: The clinical research is supported by Singapore National Medical Research grant (NMRC-0388/1999, NMRC-0712/2002).
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Garraway WM, Armstrong C, Auld S, et al. Follow-up of a cohort of men with untreated benign prostatic hyperplasia. Eur Urol 1993;24:313-8. [PubMed]
- Luo GC, Foo KT, Kuo T, et al. Diagnosis of prostate adenoma and the relationship between the site of prostate adenoma and bladder outlet obstruction. Singapore Med J 2013;54:482-6. [PubMed]
- Tan YH, Foo KT. Intravesical prostatic protrusion predicts the outcome of a trial without catheter following acute urine retention. J Urol 2003;170:2339-41. [PubMed]
- Lim KB, Wong MY, Foo KT. The outcome of trial off catheter after acute retention of urine. Ann Acad Med Singapore 1999;28:516-8. [PubMed]
- Abeygunasekera AM, Jayasinghe RJ, Duminda MT, et al. Significance of recent onset nocturnal enuresis in adult men: a prospective study. Ceylon Med J 2004;49:79-81. [PubMed]
- Wei TC, Lin TP, Chang YH, et al. Transrectal ultrasound-guided prostate biopsy in Taiwan: A nationwide database study. J Chin Med Assoc 2015. [Epub ahead of print]. [PubMed]
- Yuen JS, Ngiap JT, Cheng CW, et al. Effects of bladder volume on transabdominal ultrasound measurements of intravesical prostatic protrusion and volume. Int J Urol 2002;9:225-9. [PubMed]
- Chia SJ, Heng CT, Chan SP, et al. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int 2003;91:371-4. [PubMed]
- Lee LS, Sim HG, Lim KB, et al. Intravesical prostatic protrusion predicts clinical progression of benign prostatic enlargement in patients receiving medical treatment. Int J Urol 2010;17:69-74. [PubMed]
- Foo KT. Decision making in the management of benign prostatic enlargement and the role of transabdominal ultrasound. Int J Urol 2010;17:974-9. [PubMed]
- Foo KT. Current assessment and proposed staging of patients with benign prostatic hyperplasia. Ann Acad Med Singapore 1995;24:648-51. [PubMed]
- Ball AJ, Feneley RC, Abrams PH. The natural history of untreated "prostatism". Br J Urol 1981;53:613-6. [PubMed]
- Wang D, Foo KT. Staging of benign prostate hyperplasia is helpful in patients with lower urinary tract symptoms suggestive of benign prostate hyperplasia. Ann Acad Med Singapore 2010;39:798-802. [PubMed]
- McConnell JD, Roehrborn CG, Bautista OM, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 2003;349:2387-98. [PubMed]
- Cumpanas AA, Botoca M, Minciu R, et al. Intravesical prostatic protrusion can be a predicting factor for the treatment outcome in patients with lower urinary tract symptoms due to benign prostatic obstruction treated with tamsulosin. Urology 2013;81:859-63. [PubMed]
- Hirayama K, Masui K, Hamada A, et al. Evaluation of Intravesical Prostatic Protrusion as a Predictor of Dutasteride-Resistant Lower Urinary Tract Symptoms/Benign Prostatic Enlargement With a High Likelihood of Surgical Intervention. Urology 2015. [Epub ahead of print]. [PubMed]
- Foo KT, Liu CX. Transurethral Enucleation and Resection of Prostate. In: Manickam Ramalingam, David M. Albala, editors. Benign Prostatic Hyperplasia, Chapter 21. 2012. Macmillan Medical Communications, 2012:245-53.
- Liu C, Zheng S, Li H, et al. Transurethral enucleation and resection of prostate in patients with benign prostatic hyperplasia by plasma kinetics. J Urol 2010;184:2440-5. [PubMed]
- Zhang KY, Xing JC, Chen BS, et al. Bipolar plasmakinetic transurethral resection of the prostate vs. transurethral enucleation and resection of the prostate: pre- and postoperative comparisons of parameters used in assessing benign prostatic enlargement. Singapore Med J 2011;52:747-687514. [PubMed]
- Rassweiler J, Teber D, Kuntz R, et al. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol 2006;50:969-79; discussion 980. [PubMed]
- Horasanli K, Silay MS, Altay B, et al. Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology 2008;71:247-51. [PubMed]


