Injection therapy for Peyronie’s disease: pearls of wisdom
Peyronie’s disease (PD) is a localized connective tissue disorder of the penis that may result in formation of plaque, penile deformity, pain, erectile dysfunction and emotional stress. It can affect the tunica albuginea, septum, or intracavernous struts leading to curvature, shortening, indentation, or hourglass deformity of the erect penis. Because it is a localized disease, a focal therapy seems to be the most rational approach. Additionally, patients are understandably hesitant to have surgery on the penis. This commentary summarizes the combined experience of verapamil and Xiaflex injection by the authors. Other practitioners use interferon and other medications. We do not use these and therefore have eliminated this from the discussion.
Verapamil injection
Although not FDA approved for use in PD, verapamil has been used commonly for many years (1-3). Verapamil is administered as 10 mg in 10 cc of NS, every 2 weeks. Our practice is to perform a penile block, use a 21 g needle to administer the medication, and to give six injections prior to reevaluation of the clinical situation. If there is good improvement but not quite enough, the patient may elect to have another six injections of 20 mg in 10 cc.
Although the number of patients receiving verapamil has decreased since the FDA approved Xiaflex, there still is a patient population that seems to benefit from this medication. Unlike Xiaflex, verapamil is given in a larger volume. In other studies, injection of saline alone has a good response rate, and it is unclear to us the relative role of the drug itself versus the hydro-distension effect of the large volume of saline.
Cost
Verapamil is substantially cheaper than Xiaflex, and thus may be used when insurance coverage or other financial considerations prohibit the use of Xiaflex.
Pain
Although Xiaflex is not uncomfortable to receive, some patients have significant pain for up to 48 hours after the injection, with rare patients having discomfort beyond this period. Verapamil is more painful to receive, likely due to the volume of fluid, but is not significantly painful thereafter. It hastens the resolution of PD-related pain. Although many studies have noted that resolution of pain is an eventuality in PD patients, it is often a considerable source of bother in those patients who have it, and resolution of pain as rapidly as possible is a very desirable outcome. We have found that Xiaflex may be extremely uncomfortable in patients in whom pain is a predominant symptom.
Non-curvature deformities
Verapamil seems to have a superior outcome for deformities that are not purely curvature in nature. These include waists, hourglass, and areas of instability or hinging. Although the deformity in these cases appears lateral, a lateral plaque is relatively uncommon and these defects usually are associated with a typical, dorsally located plaque. Our surgical experience has shown us that the area of indentation is a contracture, rather than an area of underlying corporal fibrosis. The dorsal plaque is associated with abnormalities in the intracorporal struts, which causes local contracture. Our theory is that verapamil and/or the associated hydrodistension allows the struts to expand and thus corrects these types of abnormalities.
Stage of disease
With stable disease and heavy plaque calcification, verapamil seems to have much less efficacy than when used in the context of early disease and softer plaques. Overall, we prefer to use Xiaflex in the context of stable plaques.
Xiaflex (collagenase clostridium histolyticum) injection
The main difference between Xiaflex and other injectable therapy is Xiaflex’s ability to dissolve the collagenous fibrous tissue within the plaque (4,5). However, Xiaflex also carries the risks of hematoma and penile fracture due to thinning/softening of the tunica albuginea. The modeling/stretching maneuver to expand/lengthen the contracture following Xiaflex injection is as important as the injection itself. Clinical trials have clearly shown that the combination of injection plus modeling has the best results in reduction of penile curvature.
Location of injection
Anatomically, the thinnest portions of the tunica albuginea are on the lateral aspect (3 and 9 o’clock positions) and between the corpus spongiosum and the cavernosa (6 o’clock position). At this time, the company does not recommend injection to the ventral plaque for fear of damaging the urethra. After more than 1,000 injections, we feel that the ventral plaque is not necessarily a contraindication as long as the plaque is clearly palpable, not calcified, and thick (>0.3 cm by ultrasound measurement). We have also found that ventral plaques respond, in these situations, as well as dorsal plaques. The urethra can always be spared as long as the plaque can be firmly pinched between the thumb and index finger. The injection should be directed to the 5 and 7 o’clock positions not 6 o’clock position. We have seen herniation, hematoma, and micro-rupture of the lateral tunica after injection of Xiaflex to the lateral aspect of the penis. Therefore, we do not recommend Xiaflex injection to lateral aspects of the penis for men with true lateral curvature. We have not injected Xiaflex to sites of intracavernous or septal fibrosis and therefore cannot recommend it at this time.
Injection technique
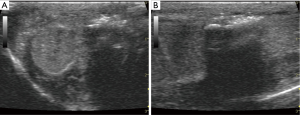
The instruction from the company is to insert the needle to the plaque and slowly withdraw while injecting Xiaflex solution. We feel that this may “waste” part of the injected Xiaflex because it is very difficult to be certain that the needle is still inside the plaque if one is injecting while withdrawing. Additionally, we have seen higher rates of ecchymosis and swelling, likely due to extravasation of Xiaflex outside of the plaque via the needle track. Instead, we prefer to forcefully inject Xiaflex to the plaque against the high resistance (Figure 1A,B). We also prefer to inject into at least two sites within the plaque to avoid rupturing the thin plaque with the total amount 0.25 mL. Of course, a large and thick plaque is not a problem with 0.25 mL.
Since the volume of Xiaflex is small, it is important to pick the best spot for injection. This can be done in several ways, but we prefer to compare the palpable plaque with the patient’s erection and choose the site that corresponds to the site of maximum deformity. One author prefers to have the patient mark this site with a permanent marker the day prior to the injection so he has the correspondence of the palpable plaque, the patient’s subjective view of the area of maximum deformity, and the view of this area as seen on auto-photography. The other authors prefer to inject a vasodilator (most of time with 0.05 mL of phentolamine/papavarine solution) and self-stimulation to induce erection and mark it with a marker before giving the local anesthetic.
Patient taking anticoagulants
Discontinuation of an anticoagulant or antiplatelet medication for 5 days prior to injection is preferred. If contraindicated (e.g., cardiac stents that require aspirin), we teach the patient to apply a loose compressive dressing and change this daily for 2-3 days to prevent excessive ecchymosis.
To operate or not to operate
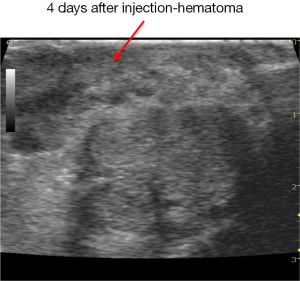
Bleeding during or after nocturnal erections can present with ecchymosis (bleeding within the subcutaneous tissue) (Figure 2) or hematoma (blood clots between Buck’s fascia and tunica) (Figure 3). In both conditions, a penile ultrasound to confirm the diagnosis is all that needed (Figure 4). Ultrasound examination of the tunica is operator dependent, and such examinations should only be done if the examiner is comfortable with this. On the other hand, if ecchymosis /hematoma developed suddenly during or after sexual intercourse, penile fracture is the most likely diagnosis until proven otherwise. If penile ultrasound confirms a sizeable tunical rupture, surgical repair is recommended.
Hourglass deformity or unilateral indentation
If the plaque is palpable at the dorsal or ventral aspect, we have injected Xiaflex into the plaque followed by daily stretching with a vacuum erection device with reasonably good results. If only lateral plaque is palpable, we do not recommend Xiaflex injection anymore because we have seen hematoma and herniation after Xiaflex injection in several cases.
Injection schedule
The package insert recommends two injections 1-3 days apart, followed by daily stretching and manipulation by the patient for 6 weeks. In some patients who developed severe skin edema and ecchymosis, we have waited up to 1 week to give the second injection. In some men with small plaque, we elected to give one Xiaflex injection followed by modeling to prevent potential tunical rupture.
Conclusions
If a patient is interested in the most definitive, rapid treatment of a stable Peyronie’s deformity, surgical approaches continue to be the gold standard. However, most of our patients are understandably hesitant to pursue surgery and are willing to undergo the inconvenience of repeated injections to achieve a less invasive approach to their deformities. Our combined experience with over 1,000 patients receiving verapamil and over 400 patients receiving Xiaflex has shown us that these medications can be very successful and satisfying, but rely on (I) careful consideration of the patient’s individual characteristics, (II) adherence to good techniques for injecting and (III) patient’s willingness to comply with their at-home physical therapy. Verapamil is appropriate for less stable disease and in softer plaques, whereas we prefer Xiaflex for more stable disease and denser plaques. We avoid Xiaflex in true lateral plaques (which are very uncommon). For technique, a fanning technique is appropriate for verapamil, administered via a 21 g needle for maximum hydrodistention. For Xiaflex, the needle should remain within the densest portion of the plaque, corresponding the point of maximum deformity, in order to minimize extravasation and subsequent ecchymoses. The best results are seen when patients comply with manipulation of the plaque, via a combination of stretching, gentle bending of the erect penis in the opposite direction of the curve, and massage of the plaque.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author TF Lue was a consultant to Auxillium Pharmaceuticals, Inc., the others have no conflicts of interest to declare.
References
- Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie's disease. J Sex Med 2012;9:288-95. Erratum in J Sex Med 2012;9:945. [PubMed]
- Alizadeh M, Karimi F, Fallah MR. Evaluation of verapamil efficacy in Peyronie's disease comparing with pentoxifylline. Glob J Health Sci 2014;6:23-30. [PubMed]
- Chung E, Garcia F, Young LD, et al. A comparative study of the efficacy of intralesional verapamil versus normal saline injection in a novel Peyronie disease animal model: assessment of immunohistopathological changes and erectile function outcome. J Urol 2013;189:380-4. [PubMed]
- Dhillon S. Collagenase Clostridium Histolyticum: A Review in Peyronie's Disease. Drugs 2015;75:1405-12. [PubMed]
- Gelbard M, Goldstein I, Hellstrom WJ, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol 2013;190:199-207. [PubMed]




