Emotional and sexual concerns in women undergoing pelvic surgery and associated treatment for gynecologic cancer
Introduction
Gynecologic cancers account for more than 90,000 of all new cancer diagnoses in the United States (1) and approximately one million worldwide annually (2). The most common types of gynecologic malignancies are endometrial (54%), ovarian (24%), and cervical (13%) cancers (1); vaginal and vulvar cancers are less prevalent. Regardless of site of disease or age of onset, coping with cancer has physical and emotional consequences. Recommended therapeutic modalities can create short- and long-term challenges to quality of life (QoL) (i.e., sexual dysfunction, menopause, lymphedema). Surgical treatment often involves the removal of some or all of the reproductive organs, including the uterus, cervix, ovaries, and fallopian tubes, and can also include the removal of lymph nodes.
Nearly 90% of patients with a history of cancer have sexual dysfunction at some point in their cancer experience (3), with the most frequent challenges being vaginal dryness, dyspareunia, and loss of desire (4-7). In addition, approximately 15-25% of patients will report depression and 10-30% will experience an anxiety disorder (8-11). Assessment and treatment are essential, as depression and anxiety not only adversely affect QoL but also compliance with treatment, ability to care for oneself, and length of hospitalization (8). Physical and emotional factors can also negatively influence a woman’s sexual response (desire, arousal, and orgasm). Therefore, it is important to address these factors in the context of cancer diagnosis and treatment.
This article provides an overview of the various pelvic surgeries and multimodality cancer treatments by anatomic site and highlights the potential emotional and sexual consequences that can influence cancer survivorship and QoL. This article also provides suggestions for clinical intervention and screening tools that can be used in clinical practice to identify some of these concerns and treatment side effects.
Ovarian cancer
The treatment for ovarian cancer usually consists of surgery involving a hysterectomy, bilateral salpingo-oophorectomy (BSO), omentectomy, lymph node removal, and tumor debulking with the goal of optimal cytoreduction (12). The removal of the ovaries and the fallopian tubes during a BSO can cause surgical menopause or even potentially aggravate menopausal symptoms in peri- or post-menopausal women. Menopausal symptoms triggered by cancer treatment are typically more abrupt, intense, and/or prolonged (13), which is caused by a sudden fall in estrogen and androgen levels; and these symptoms are qualitatively different than those of a natural menopausal decline (5-7). Cancer patients who experience a menopausal transition due to treatment can be more susceptible to urinary tract infections, emotional lability, and increased irritability (14). Unmanaged menopausal symptoms like hot flashes, changes in mood, and difficulty sleeping may impact overall QoL, function, and desire for intimacy (15-17). Low-dose antidepressants can be extremely helpful in addressing vasomotor symptoms (18), and when used for the treatment of these symptoms, may not impair sexual function (19).
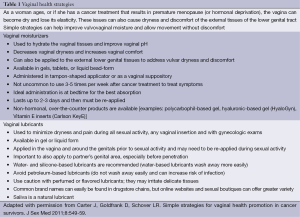
Vulvovaginal tissue quality issues also tend to be severe and chronic in female cancer patients, which directly impact their ability to feel sexual desire and achieve a fulfilling sex life without pain and discomfort (7). An internet-based evaluation of patients diagnosed with ovarian cancer showed that 63% of women felt like their diagnosis negatively affected their sex life, with both physical and emotional issues leading to diminished rates of sexual activity (20). Suggestions for addressing vulvovaginal issues are described in detail later in the article (see “Vaginal and Sexual Health Promotion Strategies” section and Table 1).
Full table
Serum CA-125 levels are often elevated in advanced ovarian cancers, providing a good biomarker for this disease (21); however, a patient’s preoccupation with these levels throughout cancer care can cause heightened anxiety and significant depressive symptomatology (6,22). Screening tools can be helpful in the clinical setting to monitor distress levels and refer patients for additional support and mental health services (see “Screening and Assessment Tools” section). These women, however, often cope with a delicate balance of wanting information on their health, knowing their “numbers”, and the fear of progression or recurrence. Although the biomarker has its limitations as a cancer screening tool in the general population and as a predictor of outcome (23), it is still a valuable clinical tool for oncologists caring for women diagnosed with ovarian cancer.
The majority of advanced-stage ovarian cancer patients will recur, prompting the need for intermittent and/or chronic chemotherapy treatment. Although the literature is more extensive in the breast cancer population, we can infer from studies since similar chemotherapeutic agents can be used in gynecologic cancer patients. Negative sequelae from chemotherapy, such as estrogen deprivation and menopause resulting in vulvovaginal dryness and atrophy, can affect sexual functioning and levels of interest and desire (24,25). Neurotoxicity from chemotherapy (i.e., neuropathy) can also directly impact QoL and function (26). Neuropathy is commonly linked to sensory changes in the hands and feet. This can alter daily activities and serve as a chronic reminder of their cancer. Nerve changes can also occur in the pelvic and clitoral area, diminishing pleasurable sensations and intimacy (27). The frequency and severity of toxicity can be enhanced by multimodal therapy and methods of administration (28,29). Patients receiving intraperitoneal (IP) therapy have reported poor health-related QoL (HRQoL) and significant neurotoxicity 3-6 weeks post-chemotherapy and 1 year later (26). Due to these adverse outcomes, less toxic therapeutic combinations are being explored. Chemotherapy can also result in nausea, vomiting, diarrhea, mucositis and fatigue, which understandably can negatively impact overall well-being and sexual activity, highlighting the need for symptom management strategies. In addition, alopecia from chemotherapy can challenge a woman’s view of herself and visibly symbolize her cancer experience (16,30).
BRCA1 and BRCA2 mutation carriers have an approximate 10-60% lifetime risk of developing ovarian cancer and an 84% risk of developing breast cancer (31). Risk-reducing salpingo-oophorectomy (RRSO) can lower the risk for ovarian, breast, and fallopian tube cancer in these women. It is recommended that prophylactic surgery be performed once childbearing is completed or at 35 years of age. One study showed an 80% risk reduction in ovarian, fallopian tube, and peritoneal cancers in women between the ages of 35 and 40 as a result of ovary and fallopian tube removal (32). However, hormonal decline and premature menopause can trigger symptoms such as hot flashes, vaginal dryness/discomfort, and a decrease in sexual function in these women to a much greater extent than in women who undergo ovarian cancer surveillance (33-37). Many women delay or defer RRSO due to reproductive and menopausal concerns (38,39). RRSO rates for women who are at risk for ovarian cancer range from 17-80% (40-43).
Psychosocial factors can influence a woman’s decision to undergo RRSO, although there is conflicting evidence regarding what these factors are (40,44-47). In one study involving a representative sample of women at high risk for ovarian cancer, decisions about prophylactic surgery were based on risk and individual sociodemographic circumstances (i.e., being parous, knowing mutation status, having a mother or sister who died from ovarian cancer) and not necessarily anxiety or distress over disease development (47). Choosing prophylactic surgery can actually be viewed as an empowering decision when women are provided with adequate information and simple strategies to address negative sexual sequelae (48,49). This consequently minimizes distress and also positively impacts overall QoL postoperatively (50).
Cognitive behavioral therapy combined with sexual health education has been demonstrated as a feasible and effective mechanism for alleviating sexual dysfunction and psychological distress in women at high risk for ovarian cancer (50). Preoperative and postoperative counseling regarding the short- and long-term negative sequelae of RRSO, the potential benefits of the surgery, and coping techniques is essential for these women as they consider this risk-reducing strategy (50). Ovarian cancer clinical trials should include patient-reported outcomes (PROs; i.e., physical symptoms and QoL domains) to help us better evaluate and manage these issues after surgery (51).
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States, with an estimated 52,630 new cases in 2014 (52). Endometrial cancer is more common in postmenopausal patients, with only 3% to 5% of cases occurring in women younger than 40 years of age (53). The standard of care for endometrial cancer usually includes a hysterectomy, BSO, and may include the removal of lymph nodes. However, treatment varies by stage of disease, and in some cases, by the age of the patient.
Many women who have early-stage disease can be observed postoperatively, with no further treatment. Over the past several decades, minimally invasive surgery has been increasingly used in lieu of open procedures to decrease morbidity (54,55). Reduction in blood loss, complications, postoperative pain, and length of hospitalization has been found with minimally invasive approaches. The Gynecologic Oncology Group (GOG) conducted a prospective cooperative trial (LAP2) comparing laparoscopy (minimally invasive approach) with laparotomy (open approach) for comprehensive surgical staging of uterine cancer. Laparoscopic staging was found to be a feasible and safe alternative to laparotomy (56), with laparoscopic patients reporting better QoL, better physical functioning, less pain, more positive body image, and quicker recovery (57,58).
Lymph node sampling as a part of endometrial cancer treatment is a source of debate due to the lack of data supporting its overall and recurrence-free survival benefits (59,60). Recent research has shown sentinel lymph node mapping procedures may be a viable option and prevent the need for regional lymphadenectomy in patients with grade 1 endometrial cancer, thereby minimizing the possibility that these patients will develop lymphedema as a result of lymph node dissection (59-62). The greater the number of lymph nodes removed surgically, the higher the risk for lymphedema of the lower extremity (63). Lymphedema is characterized by localized fluid retention and tissue swelling. It is a chronic, disfiguring, and disruptive condition that necessitates long-term management, which can impact QoL and sexual function (64). Although lymphedema is not fatal, this late effect of cancer treatment is gaining more attention as survivorship increases and adjustment issues persist years after treatment. Currently, a landmark national cooperative group trial is prospectively studying over 1,000 women receiving pelvic surgery for gynecologic cancer to determine the incidence of lower extremity lymphedema, risk factors, and the impact of this condition on emotional and functioning outcomes (GOG244). These results will guide and inform the field about this condition.
For those with higher stage disease, radiotherapy and chemotherapy are often recommended. The Post-Operative Radiotherapy in Endometrial Cancer trial (PORTEC-2) showed that treatment burden was greatly reduced by using vaginal brachytherapy (VBT) instead of external beam radiation therapy (EBRT) for many endometrial cancer patients (65,66). Longitudinal research evaluating the efficacy and toxicity of EBRT versus VBT in endometrial cancer patients found VBT to be associated with better social functioning and less symptoms of fecal leakage, diarrhea, and limitations of daily activities due to bowel symptoms (65). However, VBT has been shown to cause atrophic changes to the vaginal mucosa. These changes can result in vaginal dryness, dyspareunia, and vaginal fibrosis causing tightening and shortening of the vagina (65,67,68), and in turn can result in higher rates of sexual dysfunction and diminished sexual interest (69,70). Although increased vaginal atrophy has been seen in patients who have undergone VBT compared to ERBT, some research has shown no significant differences in sexual symptoms or sexual functioning between the two groups (65). Vaginal health strategies, including vaginal dilators, can be extremely helpful to both groups, as discussed in a later section of this article (see section on “Vaginal and Sexual Health Promotion Strategies”).
Regardless of surgical technique, if the ovaries are removed, estrogen decline can result in hot flashes, vaginal dryness, dyspareunia, and lower overall QoL (7) as well as impact future fertility and sexual function. In two recent studies, 89% of early-stage endometrial cancer survivors scored below the diagnostic clinical cut-off on the female sexual dysfunction index (FSFI), indicating sexual dysfunction (70). These patients present with symptoms of dysfunction both before and after surgical intervention (71). This highlights the need to discuss sexual health throughout the cancer care continuum.
Conservative approaches may be considered in younger women to allow for subsequent childbearing (72,73). Progesterone therapy can slow or stop the growth of cancer cells while maintaining fertility by preserving the uterus and ovaries and has shown positive obstetric outcomes (72,74-76). Duration and type of progestin treatment are debatable. Oral progestin is an alternative to hysterectomy for women younger than 45 years of age; however, live birth rates are low, necessitating fertility specialist involvement (76). When choosing an appropriate progestin, efficacy, side effects, and patient tolerability should be considered (73). A hysterectomy with ovarian preservation in women with early-stage endometrial cancer is another conservative approach that can deter premature surgical menopause and allow for future oocyte (egg) harvesting, but evaluation of possible synchronous ovarian cancer is required and patients must be committed to regular follow-up (77). The depth of myometrial invasion in the uterus, histologic grade, and potential ovarian cancer risk and that of late recurrences must be taken into account when deciding to use any treatment method (53,72,74,76,78,79).
Since endometrial cancer is typically detected at an early stage, few studies have evaluated QoL using validated measurement tools in women who present with more advanced disease (80). The few studies that have been conducted show that women faced with chronic disease and chronic therapy experience both emotional and physical challenges, with poor sexual function and other negative urinary and gynecologic sequelae (65,81). Although women who undergo chemotherapy for advanced, recurrent, or metastatic disease may experience longer progression-free survival, they may be at greater risk for the development of acute toxicity through the use of more intense chemotherapy regimens (82). Furthermore, although most endometrial cancer patients will survive their cancer, they will die from comorbidities, such as obesity (80), which underscores the need for PROs and symptom assessments in future clinical trials with advanced-disease patients to elucidate their specific needs/concerns (83). Most recently, exercise and dietary interventions have been developed for women diagnosed with endometrial cancer to decrease the risk of comorbidities and in turn have improved QoL and mental health in these women (84).
Cervical cancer
Radical hysterectomy is recommended for the treatment of early-stage cervical cancer. This surgery, however, is associated with short- and long-term changes in sexual function and overall QoL (85). Sexual function can be adversely affected by a radical hysterectomy as a result of the resection of the nerves and vascular supply to the vagina (14). Lack of libido (25-57%), lack of sensation in the labia (71%), decreased vaginal lubrication (10-26%), shortening of the vagina (25-26%), and dyspareunia (18%) have been reported by women who have undergone this intervention (86-88).
Simple hysterectomy for non-malignant indications compared to radical hysterectomy has been associated with lower vaginal blood flow responses in women (89). Denervation of the vagina and surrounding tissues (i.e., perineum) as a result of dissection of the pelvic connective tissue (or the parametrium) can alter bladder sensations. Loss of control over bodily functions (urinary and bowel) in conjunction with sexual morbidity can create major psychological distress and threaten self-esteem, identity, feelings of intimacy, and relationships (90). As a result, nerve-sparing approaches have received further attention as a means to reduce treatment ramifications and improve women’s QoL without compromising oncologic outcomes (91,92). Studies comparing nerve-sparing techniques versus standard radical hysterectomy show improved function (sexual, bowel, bladder) and less postoperative complications (91,92) together with earlier return of bladder function (93) reduced fecal incontinence and irregularity (94) and improved vaginal blood flow during arousal (95).
Cervical cancer is most common in women under 49 years of age (96,97); therefore, fertility preservation may be considered in select women. Radical vaginal trachelectomy has emerged as a safe surgical alternative for young early-stage cervical cancer patients (98-101). This procedure spares the uterus when resecting the cervix. Approximately 48% of women diagnosed with early-stage cervical cancer meet the criteria for radical trachelectomy (102). This procedure has shown similar recurrence rates to radical hysterectomy and has excellent obstetrical outcomes (99,103-106). Most often performed with a vaginal approach, radical abdominal trachelectomy has shown promising results (107,108).
In prospective studies comparing women undergoing radical hysterectomy versus radical trachelectomy, no group differences of distress, sexual function, QoL, or mood were seen (109-111). However, the results illustrated the challenges faced by all early-stage patients with regard to depression, distress, and sexual function (109-111). Although adaptive trends were seen over time, scores suggest persistent sexual function concerns for these women in comparison to healthy controls and/or normative data (109-112). In addition, many radical trachelectomy patients reported issues of neocervical stenosis (10-40%), dysmenorrhea (24%), and/or dyspareunia (10-30%). Dilators can be a helpful strategy to assist in managing neocervical stenosis and dyspareunia in these women. Ultimately, preoperative counseling regarding these potential side effects is essential for realistic expectations and adjustment in the postoperative setting (106,113,114).
Another conservative treatment option currently being explored is large conization and/or simple trachelectomy with pelvic lymphadenectomy for early-stage cervical cancer. Patients must be selected carefully, but this methodology is promising for women who want to maintain fertility after treatment for cervical cancer (115,116). This conservative surgery may also result in fewer sexual side effects compared to other fertility-preserving options such as trachelectomy, but more research is warranted (117). Women with lesions larger than 2 cm or who have deep stromal involvement are typically unable to undergo trachelectomy (118). In these patients, in whom bulky tumor is present but fertility preservation is important, researchers are exploring neoadjuvant chemotherapy to reduce tumor and lymph node metastasis so that these women can become eligible for fertility-sparing surgery (118,119). In addition, a national cooperative group trial is evaluating large conization with pelvic lymphadenectomy to simple hysterectomy with pelvic lymphadenectomy in order to answer these questions (GOG278). Though not the current standard of care, these are treatment modalities worthy of further investigation.
Multimodal therapy may be recommended for more advanced or recurrent cervical cancer, including radiation therapy with or without chemotherapy, and in some patients, a radical surgical approach may be suggested for a centralized recurrence. Radiation treatment can be delivered either prior to surgery, concurrently, or postoperatively based on the prescribed treatment plan (12). This combination of treatments can result in major vaginal toxicity and can severely impact sexual function (i.e., vaginal dryness, stenosis, dyspareunia, and atrophy) (30,120). The narrowing or shortening of the vaginal canal can result from vaginal fibrosis (68,120), and in some instances, may result in total closure, precluding sexual intercourse and vaginal examination (121,122). Dilator therapy and vaginal health strategies should be suggested (see “Vaginal and Sexual Health Promotion Strategies” section and Table 1). Changes to bowel and bladder function may also result from pelvic radiotherapy, creating concerns with sexual activity (67,123,124). Embarrassment related to bowel or bladder incontinence, diarrhea, rectal pain, and cystitis may cause feelings of unattractiveness and interfere with sexual functioning (68).
One of the most radical gynecologic surgical interventions is the pelvic exenteration, a surgery involving the en bloc resection of the pelvic organs (i.e., rectosigmoid colon, lower urinary tract, ovaries, fallopian tubes, vagina, cervix, and uterus) (12). The body is changed fundamentally through the creation of ostomies and, for some, vaginal reconstruction (125,126). This surgery is potentially curative for women with recurrent or advanced disease centrally located in the pelvis, without any sign of distant metastasis; otherwise, palliative care would be indicated. Exenterative surgery was developed to treat cervical cancer but can be used to treat other select gynecologic cancers (e.g., endometrial, vulvar cancer). Improved screening and patient selection to identify individuals without distant metastases has resulted from technological improvements in imaging (127). The best candidates appear to be those who are younger, have recurrent cervical cancer, and can achieve pathologically negative surgical margins (127). After pelvic exenteration, women often view their bodies differently, and in some cases, as less desirable or attractive (128,129). Reconstruction of a neovagina is an option best performed at the time of resection (130), but some research indicates that only 35% of patients who underwent pelvic exenteration opted to have vaginal reconstruction (127). Regardless of reconstruction decisions, sexual function changes can be expected (130,131). Ostomies for bladder and bowel elimination, for example, can trigger feelings of embarrassment, shame, and an altered body image (30). Therefore it is imperative that the healthcare team and patient discuss potential body changes (i.e., ostomy care and sexual function) preoperatively in order to optimize postoperative adjustment (128,132). A motivated patient with a good support network to assist during the recovery period is a good candidate for this type of invasive surgical procedure.
The human papillomavirus (HPV), a sexually transmitted infection, is the leading cause of cervical cancer worldwide. For many women, feelings of stigma and shame are associated with this diagnosis (133). Recent research within the general population has shown that cervical cancer patients may be judged and blamed for their diagnosis (133,134). Understanding the societal context of cervical cancer is necessary in order to assist patients managing any feelings of stigma and alienation (133). Furthermore, this stigma can be a significant barrier to screening and early detection (133,134).
Vulvar cancer
Management of vulvar cancer ranges from local vulvar excision to radical vulvectomy, which can include the removal of the entire vulva, nearby lymph nodes, and in some cases, the clitoris. Age of onset for this disease can also vary; typically, vulvar cancer presents in patients in the sixth or seventh decade of life; however, an increase in HPV-associated vulvar cancers has been seen in younger women (35 to 65 years of age) in recent years (135-137). This presents new challenges in understanding the long-term emotional, sexual, and physical consequences in this patient population and requires further study.
The ability of these patients to cope and adjust to postoperative surgical changes is related to the radicality of surgery (138-140), relationship factors (141,142), age (138), and physical function (143-145). Although poorer sexual function and decreased QoL has been associated with older age and more extensive vulvar excisions (138,139), it should be noted that some studies do not show differences in pre- and postoperative function scores. However, when compared to healthy controls, it appears that vulvar cancer patients have sexual dysfunction both before and after treatment (142,146). Permanent numbness, fatty tissue loss, and clitoral removal, as well as tissue quality changes (143), are all specific treatment-related issues known to affect sexual function after vulvar surgery (147). In addition, vulvectomy can lead to uncomfortable gynecologic exams as a result of the narrowing of the vaginal opening and decreased arousal response due to dyspareunia (148). If the clitoris is resected, clitoral orgasms will be absent (30).
Surgical management of vulvar cancer often necessitates inguinal lymph node dissection, unilaterally or bilaterally, to determine regional metastasis. As a result, the potential for wound breakdown, infection, and postoperative complications (e.g., lymphedema), and subsequent sexual dysfunction, is higher for these individuals (144,149-152). Screening tools to detect lymphedema of the lower extremity for early intervention would be ideal in the clinical setting (see “Screening and Assessment Tools” section). Sentinel lymph node procedures have been incorporated into the management of vulvar cancer as a way of assuaging concerns about morbidity, with promising results (139,141,153,154). Sentinel lymph node biopsy provides clinicians with information about lymph nodes while reducing morbidity in the short (i.e., infection) and long term (i.e., lower extremity lymphedema) (77,154). Sentinel lymph node biopsy has shown its value in vulvar cancer, and more recently, in early-stage cervical cancer (155,156). A novel sentinel lymph node mapping approach using fluorescence imaging is currently being investigated in endometrial, cervical, and vulvar cancer patients, with promising results (157,158). This technique provides higher resolution during surgery.
Emotional adjustment
Regardless of disease site, physical complications from illness and treatment can result in a sense of a less meaningful life and mood difficulties (159). Approximately 15-25% of cancer patients/survivors will be diagnosed with depression, a rate estimated to be at least four times greater than that of the general population (8); anxiety disorders will be diagnosed in 10-30% of these patients (8-11), illustrating the importance of screening in this patient population (160).
Negative feelings and distress can result from a lack of a partner and support during cancer treatment (161). A strong social support network has been found to be a buffering mechanism for physical symptoms and depression (162). For those in or seeking an intimate relationship, surgical scars can remind patients of their cancer experience and can influence self-perception (123). A women’s sexual self-schema, or view of the sexual self, can impact sexual function in gynecologic cancer patients (162,163). Women may equate these losses or changes as an insult to their sense of self, viewing their body differently and often as less attractive (128,129). For some, feelings of disconnection or vulnerability can be overwhelming and impact overall wellbeing and sexuality. Possessing a positive sexual self-schema has been found to counteract depressive symptoms (162).
The American Society of Clinical Oncology (ASCO) developed a set of guidelines for the screening, assessment, and care of anxiety and depression in cancer patients (164). These guidelines state that the evaluation and treatment of depressive symptoms should occur throughout the continuum of care. Failure to do so can increase the risk of poor QoL, which can include sexual function (164). The psychotropic medications can be very helpful in treating depression and anxiety. An estimated 79% of cancer patients are on psychotropic medications to assist with depression and anxiety; these medications can also be helpful in addressing sleep disturbances, hot flashes, and pain (165). However, some of these medications can negatively impact sexuality, so risks and benefits should be discussed and weighed accordingly (166,167).
Screening and assessment tools
Individuals at risk for psychological and sexual issues need to be identified in order to improve function, coping and enhance overall QoL. We offer some screening tools that can be used within the clinical setting to identify emotional and sexual concerns, allowing for a more in-depth evaluation for possible intervention and referral.
The distress thermometer (DT) is recommended by the National Comprehensive Cancer Network (NCCN) as a validated tool to assess distress in an oncology population (168). This simple, self-administered, internationally validated tool can be used to prioritize, triage, and screen patients prior to the initiation of treatment or throughout the continuum of care in a time-efficient and cost-effective manner (168). Distress is defined as “a multifactorial, unpleasant, emotional experience of a psychological, social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment” (169). A growing body of research has shown that gynecologic cancer patients may experience more significant distress than other cancer populations (170), with single and younger (under the age of 60) patients being at the greatest risk for distress (170). The DT assesses distress on three separate domains: physical, emotional, and practical. Worry was the strongest factor associated with distress. Another item shown to contribute to distress was difficulty getting around, which may be associated with treatment-related side effects such as fatigue, lower extremity lymphedema, and pain (171). Lack of sleep is associated with mood disturbances, suggesting that emotional distress and insomnia are interrelated in these patients (171). The DT can help identify patient concerns for appropriate triage. We encourage the reader to review the ASCO guidelines for “Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer” for a comprehensive overview of validated measures that could be used for a more in-depth assessment on these domains.
The NCCN also recommends the use of the Brief Sexual Symptom Checklist for Women as a screening tool for sexual dysfunction (172). This four-question checklist enables care providers to quickly ascertain if sexual dysfunction is present and to offer coping tools like moisturizers and lubricants for vaginal dryness and dyspareunia and dilator therapy for vaginal stenosis or atrophy. Once concerns have been identified, simple strategies can be offered (Table 1) or appropriate referrals can be made to clinicians with expertise in this area. For a more in-depth assessment, validated measures such as the PROMIS-SxF measure and the FSFI can be considered (173-176). The PROMIS-SxF was developed specifically for the assessment of sexual functioning in cancer patients, and the FSFI is one of the most widely accepted measures of sexual dysfunction. Both have been validated in cancer patients and survivors (177,178).
The Gynecologic Cancer Lymphedema Questionnaire (GCLQ) is a patient-self-reported survey used to assess individuals for lower extremity lymphedema. It is a brief 20-symptom assessment with four supplemental items to assess a patient’s consciousness of their lower or upper extremity lymphedema and their use of treatment and coping tools. This tool has been found to have good sensitivity and specificity and has been used in gynecologic cancer populations (179). If symptoms are detected, a referral should be made for formal limb measurement and/or a referral to specialists for evaluation. Support garments and physical therapy for lymphedema can be helpful to women living with and trying to manage this condition. Research on lower extremity lymphedema is limited and often lacks lymphedema-specific measures assessing the social, sexual, emotional, and QoL effects of this chronic condition (180). Disease-specific measurements and prospective data using lymphedema are greatly warranted so that we can better understand the extent of burden in individuals living with this disorder and further identify cohorts at risk for early intervention. The National Institutes of Health (NIH) and the GOG have recognized this need, and as mentioned, a national cooperative group trial is currently in progress to investigate lower extremity lymphedema in gynecologic cancer patients. The GCLQ is a validated measure that is being used both nationally and internationally to identify lymphedema (181,182).
Vaginal and sexual health promotion strategies
Clinical assessment and intervention for sexual health issues, including menopausal symptom management, may assist in reducing vulvovaginal and menopausal symptoms (hot flashes, vaginal dryness, dyspareunia, chronic UTIs, and incontinence). Simple yet effective strategies such as vaginal moisturizers and lubricants, dilators, and pelvic floor exercises can be utilized to mitigate vaginal discomfort (Table 1).
Vaginal lubricants are recommended during sexual activity or with the use of dilators to decrease vaginal irritation. Moisturizers, if applied 3-5 times per week, can help alleviate vulvovaginal symptoms by hydrating the vaginal tissues and re-establishing a normal pH level and providing relief to the lower genital tract tissue if applied externally to the vulva. Unfortunately, some women do not know the differences between moisturizers and lubricants. This results in a failure to implement these strategies correctly and at a frequency that would effectively alleviate symptoms.
Dilator therapy can help to restore elasticity of the vaginal tissues and can be especially beneficial for gynecologic cancer patients who have received pelvic radiation. However, dilators can be helpful to any gynecologic cancer patient or survivor experiencing discomfort (either with gynecologic exams or dyspareunia) (183). A recent study suggests that provision of information and resources regarding dilator use for sexual rehabilitation should ideally be given to patients before treatment and tailored to an individual’s needs (e.g., age and sexual activity) for the most benefit (184). Yet, more rigorous, prospective studies of dilator therapy are needed due to some inconsistencies in the literature (185,186).
Additionally, drawing blood flow to the pelvic floor may have possible restorative effects in the vagina (187). Therefore, the use of pelvic floor muscles could be a mechanism to facilitate circulation and arousal (188). Pelvic floor exercises also can be done in conjunction with dilator therapy for a more comprehensive stretch and provide greater awareness and control over muscles that may be contributing to pain.
Healthcare professionals are encouraged to discuss sexual and vaginal health concerns with their cancer patients (189), but there is a lack of consensus on how to best discuss the topic. In a 2012 literature review, only three studies were found that tested an intervention addressing sexual concerns for gynecologic cancer survivors (90,190-192). Several small studies have shown that education can help decrease the morbidity of vaginal atrophy (90). Telephone counseling and online psychoeducational interventions have been shown to be effective modalities for extending psychosocial services to cancer survivors (193,194).
Several models have been offered to facilitate communication between cancer patients and the healthcare team. The 5As for sexual health communication is an adaptation of a behavioral health counseling model that targets the oncology team and uses a multi-disciplinary approach (195,196). They consist of: (I) ask—raise the topic throughout the continuum of care; (II) advise—normalize any difficulties/concerns and reassure that help is available; (III) assess—brief assessment to identify symptoms in order to initiate further discussion and provide treatment recommendations; (IV) assist—provide resources such as patient educational materials, information sheets, or booklets (i.e., ACS cancer and sexuality) and referral for specialists (counselor, gynecologist urologist); and (V) arrange follow-up—patients should receive follow-up on the topic or referral at subsequent visits. The PLISSIT model can also help enhance communication about sexual function in the clinical setting (197,198). This graduated counseling system consists of four parts: (I) permission giving—letting patients know that it is common to have and discuss sexual concerns; (II) limited information—giving patients a brief education of how cancer and its associated treatments can impact sexual function; (III) specific suggestions—giving patients resources for improving sexual activity and information on interventions; and (IV) Intensive therapy—initiating or referring patients to individual therapy or sexual health counseling (199). Utilizing these models may be helpful in facilitating a discussion regarding sensitive topics such as sexual health. It is important to acknowledge the potential for sexual side effects due to treatment and to provide patients the opportunity to discuss their sexual health in a comfortable setting.
Conclusions
Surgical intervention is not typically the only treatment modality used to treat gynecologic cancer (i.e., chemotherapy, radiation therapy), and the multimodal nature of gynecologic cancer treatment has a significant impact on adjustment and QoL (85,200). QoL issues, emotional and sexual wellbeing, and treatment side effects (lymphedema/menopause) are important to women in survivorship and those living with chronic disease. The treatment decision-making process should include the potential impact of gynecologic cancer surgical treatment, associated treatment modalities, and their ramifications on physical, sexual, and emotional function and QoL. Brief assessments can be useful in the clinical care setting to assist in the identification of and addressing problematic issues throughout the continuum of care. This optimizes quality of care and ultimately the QoL in these women. Prospective clinical trials with gynecologic oncology populations should include PROs to identify subgroups at risk for difficulties during and following treatment for early intervention.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013;63:11-30. [PubMed]
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [PubMed]
- Andersen BL. How cancer affects sexual functioning. Oncology (Williston Park) 1990;4:81-8. [PubMed]
- Carter J, Rowland K, Chi D, et al. Gynecologic cancer treatment and the impact of cancer-related infertility. Gynecol Oncol 2005;97:90-5. [PubMed]
- Ganz PA, Rowland JH, Desmond K, et al. Life after breast cancer: understanding women's health-related quality of life and sexual functioning. J Clin Oncol 1998;16:501-14. [PubMed]
- Matulonis UA, Kornblith A, Lee H, et al. Long-term adjustment of early-stage ovarian cancer survivors. Int J Gynecol Cancer 2008;18:1183-93. [PubMed]
- Schover LR. Premature ovarian failure and its consequences: vasomotor symptoms, sexuality, and fertility. J Clin Oncol 2008;26:753-58. [PubMed]
- Brown LF, Kroenke K, Theobald DE, et al. The association of depression and anxiety with health related quality of life in cancer patients with depression and/or pain. Psychooncology 2010;19:734-41. [PubMed]
- Ferrell B, Smith SL, Cullinane CA, et al. Psychological well being and quality of life in ovarian cancer survivors. Cancer 2003;98:1061-71. [PubMed]
- Kamer S, Ozsaran Z, Celik O, et al. Evaluation of anxiety levels during intracavitary brachytherapy applications in women with gynecological malignancies. Eur J Gynaecol Oncol 2007;28:121-4. [PubMed]
- Norton TR, Manne SL, Rubin S, et al. Prevalence and predictors of psychological distress among women with ovarian cancer. J Clin Oncol 2004;22:919-26. [PubMed]
- Barakat RR, Markman M, Randall ME. eds. Principles and Practice of Gynecologic Oncology. 5th ed. Baltimore: Lippincott, Williams & Wilkins, 2009.
- Bodurka-Bevers D, Basen-Engquist K, Carmack CL, et al. Depression, anxiety and quality of life in patients with epithelial ovarian cancer. Gynecol Oncol 2000;78:302-8. [PubMed]
- Vrzackova P, Weiss P, Cibula D. Sexual morbidity following radical hysterectomy for cervical cancer. Expert Rev Anticancer Ther 2010;10:1037-42. [PubMed]
- Graziottin A, Basson R. Sexual dysfunction in women with premature menopause. Menopause 2004;11:766-77. [PubMed]
- Krychman ML, Pereira L, Carter J. Sexual oncology: sexual health issues in women with cancer. Oncology 2006;71:18-25. [PubMed]
- Carter J, Chi DS, Brown CL, et al. Cancer-related infertility in survivorship. Int J Gynecol Cancer 2010;20:2-8. [PubMed]
- Handley AP, Williams M. The efficacy and tolerability of SSRI/SNRIs in the treatment of vasomotor symptoms in menopausal women: a systematic review. J Am Assoc Nurse Pract 2015;27:54-61. [PubMed]
- Reed SD, Guthrie KA, Joffe H, et al. Sexual function in nondepressed women using escitalopram for vasomotor symptoms: a randomized controlled trial. Obstet Gynecol 2012;119:527-38. [PubMed]
- Hopkins TG, Stravraka C, Gabra H, et al. Sexual activity and functioning in ovarian cancer survivors: an internet-based evaluation. Climacteric 2015;18:94-8. [PubMed]
- Menon U, Griffen M, Gentry-Maharaj A. Ovarian cancer-screening – current status, future directions. Gynecol Oncol 2014;132:490-5. [PubMed]
- Reid A, Ercolano E, Schwartz P, et al. The management of anxiety and knowledge of serum CA-125 after an ovarian cancer diagnosis. Clin J Oncol Nurs 2011;15:625-32. [PubMed]
- Reade CJ, Riva JJ, Busse JW, et al. Risks and benefits of screening asymptomatic women for ovarian cancer: a systematic review and meta-analysis. Gynecol Oncol 2013;130:674-81. [PubMed]
- Carmack Taylor CL, Basen-Engquist K, Shinn EH, et al. Predictors of sexual functioning in ovarian cancer patients. J Clin Oncol 2004;22:881-9. [PubMed]
- Rosenberg SM, Tamimi RM, Gelber S, et al. Treatment-related amenorrhea and sexual functioning in young breast cancer survivors. Cancer 2014;120:2264-71. [PubMed]
- Wenzel LB, Huang HQ, Armstrong DK, et al. Baseline quality of life (QOL) as a predictor of tolerance to intraperitoneal (IP) chemotherapy for advanced epithelial ovarian cancer (EOC): a Gynecologic Oncology Group (GOG) study. J Clin Oncol 2006;24:abstr 5007.
- Hughes MK. Alterations of sexual function in women with cancer. Semin Oncol Nurs 2008;24:91-101. [PubMed]
- Pignata S, De Placido S, Biamonte R, et al. Residual neurotoxicity in ovarian cancer patients in clinical remission after first-line chemotherapy with carboplatin and paclitaxel: the Multicenter Italian Trial in Ovarian Cancer (MITO-4) retrospective study. BMC Cancer 2006;6:5. [PubMed]
- Dunton CJ. Management of treatment-related toxicity in advanced ovarian cancer. The Oncologist 2002;7 Suppl 5:11-19. [PubMed]
- Katz A. eds. Breaking the silence on cancer and sexuality: A handbook for healthcare providers. 1 ed. Pittsburgh: Oncology Nursing Society, 2007.
- Kehoe SM, Kauff ND. Screening and prevention of hereditary gynecologic cancers. Semin Oncol 2007;34:406-10. [PubMed]
- Finch A, Beiner M, Lubinski J, et al. Hereditary Ovarian Cancer Clinical Study Group. Salpingo-oophorectomy and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 Mutation. JAMA 2006;296:185-92. [PubMed]
- Elit L, Esplen MJ, Butler K, et al. Quality of life and psychosexual adjustment after prophylactic oophorectomy for a family history of ovarian cancer. Fam Cancer 2001;1:149-56. [PubMed]
- Benshushan A, Rojansky N, Chaviv M, et al. Climacteric symptoms in women undergoing risk-reducing bilateral salpingo-oophorectomy. Climacteric 2009;12:404-9. [PubMed]
- Hallowell N, Baylock B, Heiniger L, et al. kConFab Psychosocial Group on behalf of the kConFab Investigators, Price MA. Looking different, feeling different: women's reactions to risk-reducing breast and ovarian surgery. Fam Cancer 2012;11:215-24. [PubMed]
- van Oostrom I, Meijers-Heijboer H, Lodder LN, et al. Long-term psychological impact of carrying a BRCA1/2 mutation and prophylactic surgery: a 5-year follow-up study. J Clin Oncol 2003;21:3867-74. [PubMed]
- Erekson EA, Martin D, Ratner E. Oophorectomy: the debate between ovarian conservation and elective oophorectomy. Menopause 2013;20:110-4. [PubMed]
- Bradbury AR, Ibe CN, Dignam JJ, et al. Uptake and timing of bilateral prophylactic salpingo-oophorectomy among BRCA1 and BRCA2 mutation carriers. Genet Med 2008;10:161-6. [PubMed]
- Evans DG, Lalloo F, Ashcroft L, et al. Uptake of risk-reducing surgery in unaffected women at high risk of breast and ovarian cancer is risk, age, and time dependent. Cancer Epidemiol Biomarkers Prev 2009;18:2318-24. [PubMed]
- Julian-Reynier C, Bouhnik AD, Mouret-Fourme E, et al. Time to prophylactic surgery in BRCA1/2 carriers depends on psychological and other characteristics. Genet Med 2010;12:801-7. [PubMed]
- Manchanda R, Burnell M, Abdelraheim A, et al. Factors influencing uptake and timing of risk reducing salpingo-oophorectomy in women at risk of familial ovarian cancer: a competing risk time to event analysis. BJOG 2012;119:527-36. [PubMed]
- Miller SM, Roussi P, Daly MB, et al. New strategies in ovarian cancer: uptake and experience of women at high risk of ovarian cancer who are considering risk-reducing salpingo-oophorectomy. Clin Cancer Res 2010;16:5094-106. [PubMed]
- Pezaro C, James P, McKinley J, et al. The consequences of risk reducing salpingo-oophorectomy: the case for a coordinated approach to long-term follow up post surgical menopause. Fam Cancer 2012;11:403-10. [PubMed]
- Schwartz MD, Kaufman E, Peshkin BN, et al. Bilateral prophylactic oophorectomy and ovarian cancer screening following BRCA1/BRCA2 mutation testing. J Clin Oncol 2003;21:4034-41. [PubMed]
- Meiser B, Butow P, Barratt A, et al. Attitudes to prophylactic oophorectomy and screening utilization in women at increased risk of developing hereditary breast/ovarian cancer. Gynecol Oncol 1999;75:122-9. [PubMed]
- Meiser B, Butow P, Price M, et al. Attitudes to prophylactic strategies in Australian women at increased risk for breast cancer. J Womens Health (Larchmt) 2003;12:769-78. [PubMed]
- Meiser B, Price MA, Butow PN, et al. Psychosocial factors and uptake of risk-reducing salpingo-oophorectomy in women at high risk for ovarian cancer. Fam Cancer 2013;12:101-9. [PubMed]
- Finch A, Narod SA. Quality of life and health status after prophylactic salpingo-oophorectomy in women who carry a BRCA mutation: A review. Maturitas 2011;70:261-5. [PubMed]
- Litton JK, Westin SN, Reasy K, et al. Perception of screening and risk reduction surgeries in patients tested for a BRCA deleterious mutation. Cancer 2009;115:1598-604. [PubMed]
- Bober SL, Recklitis C, Bakan J, et al. Addressing sexual dysfunction after risk-reducing salpingo-oophorectomy: effects of a brief psychosexual intervention. J Sex Med 2015;12:189-97. [PubMed]
- Donovan KA, Donovan HS, Cella D, et al. Recommended patient-reported core set of symptoms and quality-of-life domains to measure in ovarian cancer treatment trials. J Natl Cancer Inst 2014;106:dju128. [PubMed]
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Available online: http://seer.cancer.gov/statfacts/html/corp.html
- Gallup DG, Stock RJ. Adenocarcinoma of the endometrium in women under 40 years of age or younger. Obstet Gynecol 1984;64:417-20. [PubMed]
- Boggess JF, Gehrig PA, Cantrell L, et al. A comparative study of 3 surgical methods for hysterectomy with staging for endometrial cancer: robotic assistance, laparoscopy, laparotomy. Am J Obstet Gynecol 2008;199:360.e1-9.
- Boggess JF, Gehrig PA, Cantrell L, et al. A case-control study of robot-assisted type III radical hysterectomy with pelvic lymph node dissection compared with open radical hysterectomy. Am J Obstet Gynecol 2008;199:357.e1-7.
- Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol 2009;27:5331-6. [PubMed]
- Kornblith AB, Huang HQ, Walker JL, et al. Quality of life of patients with endometrial cancer undergoing laparoscopic international federation of gynecology and obstetrics staging compared with laparotomy: a Gynecologic Oncology Group study. J Clin Oncol 2009;27:5337-42. [PubMed]
- Carter J, Huang H, Chase DM, et al. Sexual function of patients with endometrial cancer enrolled in the Gynecologic Oncology Group LAP2 Study. Int J Gynecol Cancer 2012;22:1624-33. [PubMed]
- Kitchener H, Swart AM, Qian Q, et al. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet 2009;373:125-36. [PubMed]
- Benedetti Panici P, Basile S, Maneschi F, et al. Systematic pelvic lymphadenectomy vs no lymphadenectomy in early-stage endometrial carcinoma: ramdonized clinical trial. J Natl Cancer Inst 2008;100:1707-16. [PubMed]
- Abu-Rustum NR, Khoury-Collado F, Pandit-Taskar N, et al. Sentinel lymph node mapping for grade 1 endometrial cancer: is it the answer to the surgical staging dilemma? Gynecol Oncol 2009;113:163-9. [PubMed]
- May K, Bryant A, Dickinson HO, et al. Lymphadenectomy for the management of endometrial cancer. Cochrane Database Syst Rev 2010;20:CD007585. [PubMed]
- Abu-Rustum NR, Alektiar K, Iasonos A, et al. The incidence of symptomatic lower-extremity lymphedema following treatment of uterine corpus malignancies: a 12-year experience at Memorial Sloan-Kettering Cancer Center. Gynecol Oncol 2006;103:714-8. [PubMed]
- Ryan M, Stainton MC, Jaconelli C, et al. The experience of lower limb lymphedema for women after treatment for gynecologic cancer. Oncol Nurs Forum 2003;30:417-23. [PubMed]
- Nout RA, Putter H, Jurgenliemk-Schulz IM, et al. Five-year quality of life of endometrial cancer patients treated in the randomized Post Operative Radiation Therapy in Endometrial Cancer (PORTECT-2) trial and comparison with norm data. Eur J Cancer 2012;48:1638-48. [PubMed]
- Nout RA, van de Poll-Franse LV, Lybeert ML, et al. Long-term outcome and quality of life of patients with endometrial carcinoma treated with or without pelvic radiotherapy in the post operative radiation therapy in endometrial carcinoma 1 (PORTEC-1) trial. J Clin Oncol 2011;29:1692-700. [PubMed]
- White ID. The assessment and management of sexual difficulties after treatment of cervical and endometrial malignancies. Clin Oncol (R Coll Radiol) 2008;20:488-96. [PubMed]
- Katz A, Njuguna E, Rakowsky E, et al. Early development of vaginal shortening during radiation therapy for endometrial or cervical cancer. Int J Gynecol Cancer 2001;11:234-5. [PubMed]
- Damast S, Alektiar KM, Goldbfarb S, et al. Sexual functioning among endometrial cancer patients treated with adjuvant high-dose-rate intra-vaginal radiation therapy. Int J Radiat Oncol Biol Phys 2012;84:e187-93. [PubMed]
- Onujiogu N, Johnson T, Seo S, et al. Survivors of endometrial cancer: who is at risk for sexual dysfunction? Gynecol Oncol 2011;123:356-9. [PubMed]
- Aerts L, Enzlin P, Verhaeghe J, et al. Sexual functioning in women after surgical treatment for endometrial cancer: a prospective controlled study. J Sex Med 2015;12:198-209. [PubMed]
- Lowe MP, Bender D, Sood AK, et al. Two successful pregnancies after conservative treatment of endometrial cancer and assisted reproduction. Fertil Steril 2002;77:188-9. [PubMed]
- Kesterson JP, Fanning J. Fertility-sparing treatment of endometrial cancer: options, outcomes, pitfalls. J Gynecol Oncol 2012;23:120-4. [PubMed]
- Wang CJ, Chao A, Yang LY, et al. Fertility-preserving treatment in young women with endometrial adenocarcinoma: A long-term cohort study. Int J Gynecol Cancer 2014;24:718-28. [PubMed]
- Park JY, Kim DY, Kim JH, et al. Long-term oncologic outcomes after fertility-sparing management using oral progestin for young women with endometrial cancer (KGOG 2002). Eur J Cancer 2013;49:868-74. [PubMed]
- Simpson AN, Feigenberg T, Clarke B, et al. Fertility sparing treatment of complex atypical hyperplasia and low grade endometrial cancer using oral progestin. Gynecol Oncol 2014;133:229-33. [PubMed]
- Zivanovic O, Khoury-Collado F, Abu-Rustum NR, et al. Sentinel lymph node biopsy in the management of vulvar carcinoma, cervical cancer, and endometrial cancer. Oncologist 2009;14:695-705. [PubMed]
- Benshushan A. Endometrial adenocarcinoma in young patients: evaluation and fertility-preserving treatment. Eur J Obstet Gynecol Reprod Biol 2004;117:132-7. [PubMed]
- Crissman JD, Azoury RS, Barnes AE, et al. Endometrial carcinoma in women 40 years of age or younger. Obstet Gynecol 1981;57:699-704. [PubMed]
- Chase DM, Watanabe T, Monk BJ. Assessment and significance of quality of life in women with gynecologic cancer. Future Oncol 2010;6:1279-87. [PubMed]
- von Gruenigen VE, Gibbons HE, Kavanagh MB, et al. A randomized trial of a lifestyle intervention in obses endometrial cancer survivors: quality of life outcomes and mediators of behavioral change. 2009. Health Qual Life Outcomes 2009;7:17. [PubMed]
- Vale CL, Tierney J, Bull SJ, et al. Chemotherapy for advanced, recurrent or metastatic endometrial carcinoma. Cochrane Database Syst Rev 2012;8:CD003915. [PubMed]
- Joly F, McAlpine J, Nout R, et al. Quality of life and patient-reported outcomes in endometrial cancer clinical trials: A call for action! Int J Gynecol Cancer 2014;24:1693-9. [PubMed]
- Basen-Engquist K, Carmack C, Brown K, et al. Response to an exercise intervention after endometrial cancer: differences between obese and non-obese survivors. Gynecol Oncol 2014;133:48-55. [PubMed]
- Greimel ER, Winter R, Kapp KS, et al. Quality of life and sexual functioning after cervical cancer treatment: a long-term follow-up study. Psychooncology 2009;18:476-82. [PubMed]
- Bergmark K, Avall-Lundqvist E, Dickman PW, et al. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med 1999;340:1383-9. [PubMed]
- Jensen PT, Klee MC, Thranov I, et al. Validation of a questionnaire for self-assessment of sexual function and vaginal changes after gynaecological cancer. Psycho-Oncology 2004;13:577-92. [PubMed]
- Pieterse QD, Maas CP, ter Kuile MM, et al. An observational longitudinal study to evaluate miction, defecation, and sexual function after radical hysterectomy with pelvic lymphadenectomy for early-stage cervical cancer. Int J Gynecol Cancer 2006;16:1119-29. [PubMed]
- Maas CP, ter Kuile MM, Laan E, et al. Objective assessment of sexual arousal in women with a history of hysterectomy. BJOG 2004;111:456-62. [PubMed]
- Brotto LA, Heiman JR, Goff B, et al. A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Arch Sex Behav 2008;37:317-29. [PubMed]
- Ditto A, Martinelli F, Mattana F, et al. Class III nerve-sparing radical hysterectomy versus standard class III radical hysterectomy: an observational study. Ann Surg Oncol 2011;18:3469-78. [PubMed]
- Ceccaroni M, Roviglione G, Spagnolo E, et al. Pelvic dysfunctions and quality of life after nerve-sparing radical hysterectomy: a multicenter comparative study. Anticancer Res 2012;32:581-8. [PubMed]
- Espino-Strebel EE, Luna JT, Domingo EJ. A comparison of the feasibility and safety of nerve-sparing radical hysterectomy with the conventional radical hysterectomy. Int J Gynecol Cancer 2010;20:1274-83. [PubMed]
- de Kroon CD, Gaarenstroom KN, van Poelgeest MI, et al. Nerve sparing in radical surgery for early-stage cervical cancer: yes we should! Int J Gynecol Cancer 2010;20:S39-41. [PubMed]
- Pieterse QD, Ter Kuile MM, Deruiter MC, et al. Vaginal blood flow after radical hysterectomy with and without nerve sparing. A preliminary report. Int J Gynecol Cancer 2008;18:576-83. [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [PubMed]
- SEER Stat Fact Sheets: Cervix Uteri Cancer. National Cancer Institute. Surveillance, Epidemiology and End Results Program. Available online: http://www.seer.cancer.gov/statistics/html/cervix.html
- Plante M. Evolution in fertility-preserving options for early-stage cervical cancer: radical trachelectomy, simple trachelectomy, neoadjuvant chemotherapy. Int J Gynecol Cancer 2013;23:982-9. [PubMed]
- Boss EA, van Golde RJ, Beerendonk CC, et al. Pregnancy after radical trachelectomy: a real option? Gynecol Oncol 2005;99:S152-6. [PubMed]
- Plante M, Renaud MC, Hoskins IA, et al. Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature. Gynecol Oncol 2005;98:3-10. [PubMed]
- Shepherd JH, Mould T, Oram DH. Radical trachelectomy in early stage carcinoma of the cervix: outcome as judged by recurrence and fertility rates. BJOG 2001;108:882-5. [PubMed]
- Sonoda Y, Abu-Rustum NR, Gemignani ML, et al. A fertility-sparing alternative to radical hysterectomy: how many patients may be eligible? Gynecol Oncol 2004;95:534-8. [PubMed]
- Wethington SL, Cibula D, Duska LR, et al. An international series on abdominal radical trachelectomy: 101 patients and 28 pregnancies. Int J Gynecol Cancer 2012;22:1251-7. [PubMed]
- Kim CH, Abu-Rustum NR, Chi DS, et al. Reproductive outcomes of patients undergoing radical trachelectomy for early-stage cervical cancer. Gynecol Oncol 2012;125:585-8. [PubMed]
- Speiser D, Mangler M, Kohler C, et al. Fertility outcomes after radical trachelectomy: a prospective study of 212 patients. Int J Gynecol Cancer 2011;21:1635-9. [PubMed]
- Plante M, Gregoire J, Renaud MC, et al. The Vaginal radical trachelectomy: an update of a series of 125 cases and 106 pregnancies. Gynecol Oncol 2011;121:290-7. [PubMed]
- van Gent MD, van den Haak LW, Gaarenstroom KN, et al. Nerve-sparing radical abdominal trachelectomy versus nerve-sparing radical hysterectomy in early-stage (FIGO IA2-IB) cervical cancer: a comparative study on feasibility and outcome. Int J Gynecol Cancer 2014;24:735-43. [PubMed]
- Pareja R, Rendon G, Sanz-Lomana CM, et al. Surgical, oncological and obstetrical outcomes after abdominal radical trachelectomy – A systematic literature review. Gynecol Oncol 2013;131:77-82. [PubMed]
- Carter J, Sonoda Y, Baser RE, et al. A 2-year prospective study assessing the emotional, sexual, and quality of life concerns of women undergoing radical trachelectomy versus radical hysterectomy for treatment of early-stage cervical cancer. Gynecol Oncol 2010;119:358-65. [PubMed]
- Song T, Choi CH, Lee YY, et al. Sexual function after surgery for early-stage cervical cancer: is there a difference in it according to the extent of surgical radicality? J Sex Med 2012;9:1697-704. [PubMed]
- Froeding LP, Ottosen C, Rung-Hansen H, et al. Sexual functioning and vaginal changes after radical vaginal trachelectomy in early stage cervical cancer patients: a longitudinal study. J Sex Med 2014;11:595-604. [PubMed]
- Brotto LA, Smith KB, Breckon E, et al. Pilot study of radical hysterectomy verses radical trachelectomy on sexual distress. J Sex Marital Ther 2013;39:510-25. [PubMed]
- Alexander-Sefre F, Chee N, Spencer C, et al. Surgical morbidity associated with radical trachelectomy and radical hysterectomy. Gynecol Oncol 2006;101:450-4. [PubMed]
- Carter J, Sonoda Y, Chi DS, et al. Radical trachelectomy for cervical cancer: postoperative physical and emotional adjustment concerns. Gynecol Oncol 2008;111:151-7. [PubMed]
- Maneo A, Sideri M, Scambia G, et al. Simple Conization and lymphadenectomy for the conservative treatment of stage IB1 cervical cancer. An Italian experience. Gynecol Oncol 2011;123:557-60. [PubMed]
- Rob L, Pluta M, Strnad P, et al. A less radical treatment option to the fertility-sparing radical trachelectomy in patients with stage I cervical cancer. Gynecol Oncol 2008;111:S116-20. [PubMed]
- Fanfani F, Landoni F, Gagliardi ML, et al. Sexual and reproductive outcomes in early stage cervical cancer patients after excisional cone as a fertility-sparing surgery: an Italian experience. J Reprod Infertil 2014;15:29-34. [PubMed]
- Robova H, Halaska M, Pluta M, et al. The role of neoadjuvant chemotherapy and surgery in cervical cancer. Int J Gynecol Cancer 2010;20:S42-6. [PubMed]
- Marchiole P, Tigaud JD, Costantini S, et al. Neoadjuvant chemotherapy and vaginal radical trachelectomy for fertility-sparing treatment in women affected by cervical cancer (FIGO stage IB-IIA1). Gynecol Oncol 2011;122:484-90. [PubMed]
- Schover LR, Fife M, Gershenson D. Sexual dysfunction and treatment for early stage cervical cancer. Cancer 1989;63:204-12. [PubMed]
- Brand AH, Bull CA, Cakir B. Vaginal stenosis in patients treated with radiotherapy for carcinoma of the cervix. Int J Gynecol Cancer 2006;16:288-93. [PubMed]
- Decruze SB, Guthrie D, Magnani R. Prevention of vaginal stenosis in patients following vaginal brachytherapy. Clin Oncol (R Coll Radiol) 1999;11:46-8. [PubMed]
- Roth AJ, Carter J, Nelson CJ. Sexuality after cancer. In: Holland JC, Breitbart WS, Jacobsen PB, et al. eds. Psycho-oncology. 2nd ed. New York: Oxford University Press, Inc., 2010:245-50.
- Katz A. Interventions for sexuality after pelvic radiation therapy and gynecological cancer. Cancer J 2009;15:45-7. [PubMed]
- Hawighorst-Knapstein S, Schonefussrs G, Hoffmann SO, et al. Pelvic exenteration: effects of surgery on quality of life and body image--a prospective longitudinal study. Gynecol Oncol 1997;66:495-500. [PubMed]
- Ratliff CR, Gershenson DM, Morris M, et al. Sexual adjustment of patients undergoing gracilis myocutaneous flap vaginal reconstruction in conjunction with pelvic exenteration. Cancer 1996;78:2229-35. [PubMed]
- Benn T, Brooks RA, Zhang Q, et al. Pelvic exenteration in gynecologic oncology: a single institution study over 20 years. Gynecol Oncol 2011;122:14-8. [PubMed]
- Carter J, Chi DS, Abu-Rustum N, et al. Brief report: total pelvic exenteration--a retrospective clinical needs assessment. Psycho-Oncology 2004;13:125-31. [PubMed]
- Corney RH, Crowther ME, Everett H, et al. Psychosexual dysfunction in women with gynaecological cancer following radical pelvic surgery. Br J Obstet Gynaecol 1993;100:73-8. [PubMed]
- Pusic AL, Mehrara BJ. Vaginal reconstruction: An algorithm approach to defect classificiation and flap reconstruction. J Surg Oncol 2006;94:515-21. [PubMed]
- Rezk YA, Hurley K, Carter J, et al. A prospective study of quality of life in patients undergoing pelvic exenteration: Interim results. Gynecol Oncol 2013;128:191-7. [PubMed]
- Maggioni A, Roviglione G, Landoni F, et al. Pelvic exenteration: ten-year experience at the European Institute of Oncology in Milan. Gynecol Oncol 2009;114:64-8. [PubMed]
- Shepherd MA, Gerend M. The blame game: cervical cancer,knowledge of its link to human papillomavirus and stigma. Psychol Health 2013;29:94-109. [PubMed]
- Kwan TT, Tam K, Lee P, et al. Destigmatising human papillomavirus in the context of cervical cancer: a randomized controlled trial. Psychooncology 2010;19:1329-39. [PubMed]
- Del Pino M, Rodriguez-Caruchio L, Ordi J. Pathways of vulvar intra-epithelial neoplasia and squamous cell carcinoma. Histopathology 2013;62:161-75. [PubMed]
- Barton DP. The prevention and management of treatment related morbidity in vulvar cancer. Best Pract Res Clin Obstet Gynaecol 2003;17:683-701. [PubMed]
- Joura EA, Losch A, Haider-Angeler MG, et al. Trends in vulvar neoplasia. Increasing incidence of vulvar intraepithelial neoplasia and squamous cell carcinoma of the vulva in young women. J Reprod Med 2000;45:613-5. [PubMed]
- Likes WM, Stegbauer C, Tillmanns T, et al. Correlates of sexual function following vulvar excision. Gynecol Oncol 2007;105:600-3. [PubMed]
- Novackova M, Halaska M, Robova H, et al. A prospective study in the evaluation of quality of life after vulvar cancer surgery. Int J Gynecol Cancer 2015;25:166-73. [PubMed]
- Günther V, Malchow B, Schubert M, et al. Impact of radical operative treatment on the quality of life in women with vulvar cancer-A retrospective study. Eur J Surg Oncol 2014;40:875-82. [PubMed]
- Barlow EL, Hacker NF, Hussain R, et al. Sexuality and body image following treatment for early-stage vulvar cancer: a qualitative study. J Adv Nurs 2014;70:1856-66. [PubMed]
- Hazewinkel MH, Laan ET, Sprangers MA, et al. Long-term sexual function in survivors of vulvar cancer: A cross-sectional study. Gynecol Oncol 2012;126:87-92. [PubMed]
- Janda M, Obermair A, Cella D, et al. Vulvar cancer patients' quality of life: a qualitative assessment. Int J Gynecol Cancer 2004;14:875-81. [PubMed]
- Forner DM, Dakhil R, Lampe B. Quality of life and sexual function after surgery in early stage vulvar cancer. Eur J Surg Oncol 2015;41:40-5. [PubMed]
- Mirabeau-Beale KL, Viswanathan AN. Quality of life (QOL) in women treated for gynecologic malignancies with radiation therapy: A literature review of patient-reported outcomes. Gynecol Oncol 2014;134:403-9. [PubMed]
- Aerts L, Enzlin P, Verhaeghe J, et al. Psychologic, relational, and sexual functioning in women after surgical treatment of vulvar malignancy: a prospective controlled study. Int J Gynecol Cancer 2014;24:372-80. [PubMed]
- Andersen BL, Hacker NF. Psychosexual adjustment after vulvar surgery. Obstet Gynecol 1983;62:457-62. [PubMed]
- Audette C, Waterman J. The sexual health of women after gynecologic malignancy. J Midwifery Womens Health 2010;55:357-62. [PubMed]
- Carlson JW, Kauderer J, Walker JL, et al. A randomized phase III trial of VH fibrin sealent to reduce lymphedema after inguinal lymph node dissection: A Gynecologic Oncology Group Study. Gynecol Oncol 2008;110:76-82. [PubMed]
- Burke TW, Stringer CA, Gershenson DM, et al. Radical wide excision and selective inguinal node dissection for squamous cell carcinoma of the vulva. Gynecol Oncol 1990;38:328-32. [PubMed]
- Hacker NF, Leuchter RS, Berek JS, et al. Radical vulvectomy and bilateral inguinal lymphadenectomy through separate groin incisions. Obstet Gynecol 1981;58:574-9. [PubMed]
- Berman ML, Soper JT, Creasman WT, et al. conservative surgical management of superficially invasive stage I vulvar carcinoma. Gynecol Oncol 1989;35:352-7. [PubMed]
- Frumovitz M, Levenback CF. Lymphatic mapping and sentinel node biopsy in vulvar, vaginal, and cervical cancers. Oncology (Williston Park) 2008;22:529-36; discussion 38-9, 42-3.
- Van der Zee AG, Oonk MH, De Hullu JA, et al. Sentinel node dissection is safe in the treatment of early-stage vulvar cancer. J Clin Oncol 2008;26:884-9. [PubMed]
- Roy M, Bouchard-Fortier G, Popa I, et al. Value of sentinel node mapping in cancer of the cervix. Gynecol Oncol 2011;122:269-74. [PubMed]
- Cormier B, Diaz JP, Shih K, et al. Establishing a sentinel lymph node mapping algorithm for the treatment of early cervical cancer. Gynecol Oncol 2011;122:275-80. [PubMed]
- Crane LM, Themelis G, Arts HJ, et al. Intraoperative near-infrared fluorescence imaging for sentinel lymph node detection in vulvar cancer: first clinical results. Gynecol Oncol 2011;120:291-5. [PubMed]
- Hutteman M, van der Vorst JR, Gaarenstroom KN, et al. Optimization of near-infrared fluorescent sentinel lymph node mapping for vulvar cancer. Am J Obstet Gynecol 2012;206:89.e1-5.
- Simonelli LE, Fowler J, Maxwell GL, et al. Physical sequelae and depressive symptoms in gynecologic cancer survivors: meaning in life as a mediator. Ann Behav Med 2008;35:275-84. [PubMed]
- Linden W, Vodermaier A, MacKenzie R, et al. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J Affect Disord 2012;141:343-51. [PubMed]
- Kagan SH, Holland N, Chalian AA. Sexual issues in special populations: geriatric oncology – sexuality and older adults. Semin Oncol Nurs 2008;24:120-6. [PubMed]
- Carpenter KM, Fowler JM, Maxwell GL. Direct and buffering effects of social support among gynecologic cancer survivors. Ann Behav Med 2010;39:79-90. [PubMed]
- Andersen BL, Woods XA, Copeland LJ. Sexual self-schema and sexual morbidity among gynecologic cancer survivors. J Consult Clin Psychol 1997;65:221-9. [PubMed]
- Andersen BL, DeRubeis RJ, Berman BS, et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology Guideline Adaptation. J Clin Oncol 2014;32:1605-19. [PubMed]
- Kim HF, Fisch MJ. Antidepressant use in ambulatory cancer patients. Curr Oncol Rep 2006;8:275-81. [PubMed]
- Werneke U, Northey S, Bhugra D. Antidepressants and sexual dysfunction. Acta Psychiatr Scand 2006;114:384-97. [PubMed]
- Balon R. SSRI-associated sexual dysfunction. Am J Psychiatry 2006;163:1504-9. [PubMed]
- Donovan KA, Grassi L, McGinty H, et al. Validation of the distress thermometer worldwide: state of science. Psychooncology 2014;23:241-50. [PubMed]
- National Comprehensive Cancer Network (2007) Clinical practice guidelines in oncology: distress management (v.1.2008). Available online: http://www.nccn.org/professionals/physician_gls/PDF/distress.pdf, accessed on November 26, 2014.
- Johnson RL, Gold M, Wyche K. Distress in women with gynecologic cancer. Psychooncology 2010;19:665-8. [PubMed]
- VanHoose L, Black LL, Doty K, et al. An analysis of the distress thermometer problem list and distress in patients with cancer. Support Care Cancer 2015;23:1225-32. [PubMed]
- Denlinger CS, Carlson RW, Are M, et al. Survivorship: sexual dysfunction (female), version 1.2013. J Natl Compr Canc Netw 2014;12:184-92. [PubMed]
- Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): Ccross-validation and development of clinical cutoff scores. J Sex Marital Ther 2005;31:1-20. [PubMed]
- Flynn KE, Jeffery DD, Keefe FJ, et al. Sexual functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)). Psychooncology 2011;20:378-86. [PubMed]
- Flynn KE, Reese JB, Jeffery DD, et al. Patient experiences with communication about sex during and after treatment for cancer. Psychooncology 2012;21:594-601. [PubMed]
- Jeffery DD, Tzeng JP, Keefe FJ, et al. Initial report of the cancer Patient-Reported Outcomes Measurement Information System (PROMIS) sexual function committee: review of sexual function measures and domains used in oncology. Cancer 2009;115:1142-53. [PubMed]
- Baser RE, Li Y, Carter J. Psychometric validation of the Female Sexual Function Index (FSFI) in cancer survivors. Cancer 2012;118:4606-18. [PubMed]
- Flynn KE, Reeve BB, Lin L, et al. Construct validity of the PROMIS sexual function and satisfaction measures in patients with cancer. Health Qual Life Outcomes 2013;11:40. [PubMed]
- Carter J, Raviv L, Appollo K, et al. A pilot study using the Gynecologic Cancer Lymphedema Questionnaire (GCLQ) as a clinical care tool to identify lower extremity lymphedema in gynecologic cancer survivors. Gynecol Oncol 2010;117:317-23. [PubMed]
- Cella DF, Wiklund I, Shumaker SA, et al. Integrating health-related quality of life into cross-national clinical trials. Qual Life Res 1993;2:433-40. [PubMed]
- Lim MC, Lee JS, Nam BH, et al. Lower extremity edema in patients with early ovarian cancer. J Ovarian Res 2014;7:28. [PubMed]
- Lim MC, Lee JS. Development and evaluation of the Korean version of the Gynecologic Cancer Lymphedema Questionnaire in gynecologic cancer survivors. Gynecol Oncol 2014;133:111-6. [PubMed]
- Carter J, Goldfrank D, Schover LR. Simple strategies for vaginal health promotion in cancer survivors. J Sex Med 2011;8:549-59. [PubMed]
- Bakker RM, Kuile MM, Vermeer WM, et al. Sexual rehabilitation after pelvic radiotherapy and vaginal dilator use. Int J Gynecol Cancer 2014;24:1499-506. [PubMed]
- Johnson N, Miles TP, Cornes P. Dilating the vagina to prevent damage from radiotherapy: systematic review of the literature. BJOG 2010;117:522-31. [PubMed]
- Miles T, Johnson N. Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev 2014;9:CD007291. [PubMed]
- Schroder M, Mell LK, Hurteau JA, et al. Clitoral therapy device for treatment of sexual dysfunction in irradiated cervical cancer patients. Int J Radiat Oncol Biol Phys 2005;61:1078-86. [PubMed]
- Lowenstein L, Gruenwald I, Gartman I, et al. Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J 2010;21:553-6. [PubMed]
- Hautamäki-Lamminen K, Lipiainen L, Beaver K, et al. Identifying cancer patients with greater need for information about sexual issues. Eur J Oncol Nurs 2013;17:9-15. [PubMed]
- Abbott-Anderson K. Kwekkeboom. A systematic review of sexual concerns reported by gynecologic cancer survivors. Gynecol Oncol 2012;124:477-89. [PubMed]
- Caldwell R, Classen C, Lagana L, et al. Changes in sexual functioning and mood among women treated for gynecological cancer who receive group therapy: a pilot study. J Clin Psychol Med Settings 2003;10:149-56.
- Robson M, Hensley M, Barakat R, et al. Quality of life in women at risk for ovarian cancer who have undergone risk-reducing oophorectomy. Gynecol Oncol 2003;89:281-7. [PubMed]
- Classen CC, Chivers ML, Urowitz S, et al. Psychosexual distress in women with gynecologic cancer: a feasibility study of an online support group. Psychooncology 2013;22:930-5. [PubMed]
- Schover LR, Yuan Y, Fellman BM, et al. Efficacy trial of an internet-based intervention for cancer-related female sexual dysfunction. J Natl Compr Canc Netw 2013;11:1389-97. [PubMed]
- Park ER, Norris RL, Bober SL. Sexual health communication during cancer care: barriers and recommendations. Cancer J 2009;15:74-7. [PubMed]
- Bober SL, Carter J, Falk S. Addressing female sexuality after cancer by internist and primary care providers. J Sex Med 2013;10 Suppl 1:112-9. [PubMed]
- Penson RT, Gallagher J, Gioiella ME, et al. Sexuality and cancer: conversation comfort zone. Oncologist 2000;5:336-44. [PubMed]
- von Eschenbach AC, Schover LR. The role of sexual rehabilitation in the treatment of patients with cancer. Cancer 1984;54:2662-7. [PubMed]
- Bodurka DC, Sun CC. Sexual function after gynecologic cancer. Obstet Gynecol Clin North Am 2006;33:621-30. [PubMed]
- Liavaag AH, Dorum A, Bjoro T, et al. A controlled study of sexual activity and functioning in epithelial ovarian cancer survivors. A therapeutic approach. Gynecol Oncol 2008;108:348-54. [PubMed]


